Use of Aclidinium Did Not Increase the Risk of Death
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

(Or) Aravind Doki
Available Online through www.ijpbs.com (or) www.ijpbsonline.com IJPBS |Volume 3| Issue 3 |JUL-SEP|2013|152-161 Research Article Pharmaceutical Sciences METHOD DEVELOPMENT AND VALIDATION OF RP-HPLC METHOD FOR SIMULTANEOUS ESTIMATION OF CLIDINIUM BROMIDE, CHLORDIAZEPOXIDE AND DICYCLOMINE HYDROCHLORIDE IN BULK AND COMBINED TABLET DOSAGE FORMS Aravind.Doki* and Kamarapu.SK Department of Pharmaceutical Analysis, Sri Shivani College Of Pharmacy, Mulugu Road, Warangal, Andrapradesh, India, 506001. *Corresponding Author Email: [email protected] ABSTRACT The study describes method development and subsequent validation of RP-HPLC method for simultaneous estimation of Clidinium bromide (CDB), Chlordiazepoxide (CDZ) and Dicyclomine hydrochloride (DICY) in bulk and combined tablet dosage forms. Chromatographic separation was achieved on a Kromasil C18 (250 mm × 4.6 mm id, 5µm) column using a mobile phase ratio consisting of (40:30:30) Methanol: Acetonitrile: Potassium di hydrogen phosphate buffer (0.05M, PH 4.0 adjusting with 0.5% Ortho phosphoric acid) at flow rate 1.0 ml/min. The detection wavelength is 270 nm. The retention times of Clidinium bromide, Chlordiazepoxide and Dicyclomine hydrochloride were found to be 7.457 min, 4.400 min and 3.397 min respectively. The developed method was validated as per ICH guidelines using the parameters such as accuracy, precision, linearity, LOD, LOQ, ruggedness and robustness. The developed and validated method was successfully used for the quantitative analysis of Clidinium bromide, Chlordiazepoxide and Dicyclomine hydrochloride in bulk and combined tablet dosage forms. KEY WORDS Clidinium bromide, Chlordiazepoxide and Dicyclomine hydrochloride, Normaxin tablet dosage forms, HPLC, Method validation. INTRODUCTION hydrochloride (1, 1-bicyclohexyl-1-carboxilicacid-2- Clidinium bromide (3-[(2-hydroxy-2, [diethyl amino] ethyl ester) is an anticholinergic drug 2diphenylacetyl)-oxy]-1-methyl-1-azoniabicylo- (tertiary amine). -

Muscarinic Acetylcholine Receptor
mAChR Muscarinic acetylcholine receptor mAChRs (muscarinic acetylcholine receptors) are acetylcholine receptors that form G protein-receptor complexes in the cell membranes of certainneurons and other cells. They play several roles, including acting as the main end-receptor stimulated by acetylcholine released from postganglionic fibersin the parasympathetic nervous system. mAChRs are named as such because they are more sensitive to muscarine than to nicotine. Their counterparts are nicotinic acetylcholine receptors (nAChRs), receptor ion channels that are also important in the autonomic nervous system. Many drugs and other substances (for example pilocarpineand scopolamine) manipulate these two distinct receptors by acting as selective agonists or antagonists. Acetylcholine (ACh) is a neurotransmitter found extensively in the brain and the autonomic ganglia. www.MedChemExpress.com 1 mAChR Inhibitors & Modulators (+)-Cevimeline hydrochloride hemihydrate (-)-Cevimeline hydrochloride hemihydrate Cat. No.: HY-76772A Cat. No.: HY-76772B Bioactivity: Cevimeline hydrochloride hemihydrate, a novel muscarinic Bioactivity: Cevimeline hydrochloride hemihydrate, a novel muscarinic receptor agonist, is a candidate therapeutic drug for receptor agonist, is a candidate therapeutic drug for xerostomia in Sjogren's syndrome. IC50 value: Target: mAChR xerostomia in Sjogren's syndrome. IC50 value: Target: mAChR The general pharmacol. properties of this drug on the The general pharmacol. properties of this drug on the gastrointestinal, urinary, and reproductive systems and other… gastrointestinal, urinary, and reproductive systems and other… Purity: >98% Purity: >98% Clinical Data: No Development Reported Clinical Data: No Development Reported Size: 10mM x 1mL in DMSO, Size: 10mM x 1mL in DMSO, 1 mg, 5 mg 1 mg, 5 mg AC260584 Aclidinium Bromide Cat. No.: HY-100336 (LAS 34273; LAS-W 330) Cat. -

77Da2550569e5553dc05b76601
www.ijpsonline.com 2003;13:121-7. RM, Medina-Hernandez MJ. Determination of anticonvulsant drugs in 10. French WN, Matsui FF, Smith SJ. Determination of major impurity pharmaceutical preparations by micellar liquid chromatography. J Liq in chlordiazepoxide formulations and drug substance. J Pharm Sci Chromatogr Related Techno 2004;27:153-70. 2006;64:1545-7. 15. Toral MI, Richter P, Lara N, Jaque P, Soto C, Saavedra M. 11. Stahlmann S, Karl-Artur K. Analysis of impurities by high-performance Simultaneous determination of chlordiazepoxide and clidinium bromide thin-layer chromatography with fourier transform infrared spectroscopy in pharmaceutical formulations by derivative spectrophotometry. Int J and UV absorbance detection in situ measurement: chlordiazepoxide in Pharm 1999;189:67-74. bulk powder and in tablets. J Chromatogr-A 1998;13:145-52. 16. Beckett AH, Stenlake JB. Practice Pharmaceutical Chemistry; 4th ed. 12. Saudagar RB, Saraf S. Spectrophotometric determination of Part II. New Delhi: CBS Publishers; 1997. p. 285. chlordiazepoxide and trifluoperazine hydrochloride from combined dosage form. Indian J Pharm Sci 2007;69:149-52. Accepted 13 August 2009 13. Davidson AG. Assay of chlordiazepoxide and demoxepam in Revised 20 May 2009 chlordiazepoxide formulations by difference spectrophotometry. J Received 24 June 2008 Pharm Sci 1984;73:55-8. 14. Cholbi-Cholbi MF, Martínez-Pla JJ, Sagrado S, Villanueva-Camanas Indian J. Pharm. Sci., 2009, 71 (4): 468-472 Spectrophotometric and Chromatographic Simultaneous Estimation of Amitriptyline Hydrochloride and Chlordiazepoxide in Tablet Dosage Forms SEJAL PATEL* AND N. J. PATEL S. K. Patel College of Pharmaceutical Education and Research, Department of Pharmaceutical Chemistry, Ganpat University, Kherva, Mehsana-382711, Gujarat, India Patel and Patel, et al.: Simultaneous Estimation of Amitriptyline Hydrochloride and Chlordiazepoxide A binary mixture of amitriptyline HCl and chlordiazepoxide was determined by three different methods. -

ST Louis Formulary
Learn About Your Formulary Your drug list, also called a formulary, is the list of drugs covered by St. Louis County Department of Health. Your plan with the St. Louis County Department of Health has specific guidelines you must follow to get prescription drug coverage. You must choose generic medications when they are Many drug companies offer programs to help people available. Generic medications have the same ingredients afford their drugs. We encourage you to ask your doctor as brand drugs, at lower prices. about manufacturer assistance programs. You must fill your prescription at participating pharmacies Drugs are listed on the formulary in alphabetical order by within the St. Louis area: name in the appropriate therapeutic category and class. > CVS > The Medicine Shoppe > Walmart > Schnucks Medications on the High Priority Drug List are covered for > Sam's Club > Beverly Hills Pharmacy ONLY two 30-day fills per year. > Dierbergs > If you are prescribed a High Priority Drug, contact the drug maker to request assistance in getting your medication at reduced or no cost. You must get your prescriptions from Department of > If you do not take this step, you will pay 100% of the Health Physicians discounted drug cost after getting two 30-day fills. > If a medication is prescribed by a non-panel doctor, a > The High Priority Drug List includes: special review is required and can be requested at the • Diabetes drugs: Lantus, Novolog and Novolin number below. • Asthma Inhalers: Atrovent, Spiriva, Ventolin, Proair, Respiclick, Symbicort, Advair, Flovent and Proventil Online Tools Who can I call if I have a question? Our Customer Service Center is available 24 hours a day, 7 Access your pharmacy beneft information through our days a week, 365 days a year to help answer any questions or portal, Members.EnvolveRx.com, and mobile app, concerns you have about your pharmacy benefit. -

Title 16. Crimes and Offenses Chapter 13. Controlled Substances Article 1
TITLE 16. CRIMES AND OFFENSES CHAPTER 13. CONTROLLED SUBSTANCES ARTICLE 1. GENERAL PROVISIONS § 16-13-1. Drug related objects (a) As used in this Code section, the term: (1) "Controlled substance" shall have the same meaning as defined in Article 2 of this chapter, relating to controlled substances. For the purposes of this Code section, the term "controlled substance" shall include marijuana as defined by paragraph (16) of Code Section 16-13-21. (2) "Dangerous drug" shall have the same meaning as defined in Article 3 of this chapter, relating to dangerous drugs. (3) "Drug related object" means any machine, instrument, tool, equipment, contrivance, or device which an average person would reasonably conclude is intended to be used for one or more of the following purposes: (A) To introduce into the human body any dangerous drug or controlled substance under circumstances in violation of the laws of this state; (B) To enhance the effect on the human body of any dangerous drug or controlled substance under circumstances in violation of the laws of this state; (C) To conceal any quantity of any dangerous drug or controlled substance under circumstances in violation of the laws of this state; or (D) To test the strength, effectiveness, or purity of any dangerous drug or controlled substance under circumstances in violation of the laws of this state. (4) "Knowingly" means having general knowledge that a machine, instrument, tool, item of equipment, contrivance, or device is a drug related object or having reasonable grounds to believe that any such object is or may, to an average person, appear to be a drug related object. -
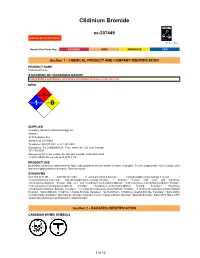
Clidinium Bromide
Clidinium Bromide sc-207449 Material Safety Data Sheet Hazard Alert Code Key: EXTREME HIGH MODERATE LOW Section 1 - CHEMICAL PRODUCT AND COMPANY IDENTIFICATION PRODUCT NAME Clidinium Bromide STATEMENT OF HAZARDOUS NATURE CONSIDERED A HAZARDOUS SUBSTANCE ACCORDING TO OSHA 29 CFR 1910.1200. NFPA FLAMMABILITY1 HEALTH1 HAZARD INSTABILITY0 SUPPLIER Company: Santa Cruz Biotechnology, Inc. Address: 2145 Delaware Ave Santa Cruz, CA 95060 Telephone: 800.457.3801 or 831.457.3800 Emergency Tel: CHEMWATCH: From within the US and Canada: 877-715-9305 Emergency Tel: From outside the US and Canada: +800 2436 2255 (1-800-CHEMCALL) or call +613 9573 3112 PRODUCT USE Quaternary ammonium antimuscarinic agent with peripheral actions similar to those of atropine. For the symptomatic relief of peptic ulcer and other gastrointestinal disorders. Taken by mouth. SYNONYMS C22-H26-Br-N-O3, C22-H26-Br-N-O3, "1-azoniabicyclo(2.2.2)octane, 3-[(hydroxydiphenylacetyl)oxy]-1-methyl-, ", "1-azoniabicyclo(2.2.2)octane, 3-[(hydroxydiphenylacetyl)oxy]-1-methyl-, ", bromide, "benzilic acid, ester with 3-hydroxy- 1-methylquinuclidinium", "benzilic acid, ester with 3-hydroxy-1-methylquinuclidinium", "3-(benziloyloxy)-1-methylquinuclidinium bromide", "3-(benziloyloxy)-1-methylquinuclidinium bromide", "3-hydroxy-1-methylquinuclidinium bromide benzilate", "3-hydroxy- 1-methylquinuclidinium bromide benzilate", "1-methyl-3-benziloxyloxy-quinuclidinium bromide", "1-methyl-3-benziloxyloxy-quinuclidinium bromide", "quinuclidinium, 3-hydroxy-1-methyl-bromide, benzilate", "quinuclidinium, 3-hydroxy-1-methyl-bromide, benzilate", "quinuclidinol methylbromide, benzilate", Apo-Chlorax, Chlorax, Clipoxide, Corium, Librax, Libraxin, Quarzan, "Quarzan bromide", RO-2-3773, RO-2-3773, "quaternary ammonium antimuscarinic/ anticholinergic" Section 2 - HAZARDS IDENTIFICATION CANADIAN WHMIS SYMBOLS 1 of 13 Clidinium Bromide sc-207449 Material Safety Data Sheet Hazard Alert Code Key: EXTREME HIGH MODERATE LOW EMERGENCY OVERVIEW RISK Harmful if swallowed. -

Dizziness/Balance Evaluation Patient Instructions You Are Scheduled for a Test of Your Balance System
Dizziness/Balance Evaluation Patient Instructions You are scheduled for a test of your balance system. There are a few things you should know prior to your appointment. MEDICATIONS Certain medications affect the test results. Below is a partial list of medications that should not be taken for 48 hours prior to the test. Ask your doctor if you have concerns about discontinuing your medications. The list below is a partial list with generic name first and trademark name bolded in parenthesis. • Alcohol - beer, wine, liquor, cough medicine • Medications commonly used to reduce dizziness and nausea - Meclizine (Antivert, Bonnine, Ru-Vert-M), Hydroxyzine (Atarax, Vistaril), Lorazepam (Ativan), Diphenhydramine (Benadryl), Prochlorperazine (Compazine), Dimenhydrinate (Dramamine), Clonazepam (Klonipin), Cyclizine (Marezine), Promethazine (Phenergan), Trimethobenzamine (Tigan), Diazepam (Valium), Nearly all motion sickness patches or medications. OTHER MEDICATIONS • Analgesics/Narcotics - Codeine, Demerol, Phenaphen, Tylenol with Codeine, Percocet, Darvocet • Anti-histamines - Fexofenadine (Allegra), Loratadine (Claritin, Alavert), Chlorpheniramine (Chlor-Trimeton, Efidac, Teldrin), Brompheniramine (Dimetane), Clemastine (Tavist), Cetirizine (Zyrtec), nearly all-over-the-counter allergy or flu/cold medicines • Sedatives - Flurazepam (Dalmane), Triazolam (Halcion), Pentobarbital (Nembutal), Temazepam (Restoril), Secobarbital (Seconal), among others. • Tranquilizers/Anti-anxiety medications - Chlordiazepoxide hydrochloride and clidinium bromide (Librax), -

Federal Register/Vol. 77, No. 115/Thursday, June 14, 2012
Federal Register / Vol. 77, No. 115 / Thursday, June 14, 2012 / Notices 35691 TABLE 1—LIST OF SAFETY AND EFFECTIVENESS SUMMARIES FOR APPROVED PMAS MADE AVAILABLE FROM JANUARY 1, 2012, THROUGH MARCH 31, 2012—Continued PMA No., Docket No. Applicant Trade name Approval date P060008.S046, FDA–2012–M–0210 ... Boston Scientific Corp ......................... TAXUS Liberte´ Paclitaxel-Eluting Cor- February 22, 2012. onary Stent System (Monorail and Over-The-Wire Delivery Systems). P030025.S086, FDA–2012–M–0209 ... Boston Scientific Corp ......................... TAXUS Express2 Paclitaxel-Eluting February 22, 2012. Coronary Stent System (Monorail and Over-The-Wire Delivery Sys- tems). P110023, FDA–2012–M–0221 ............ ev3, Inc ................................................ Everflex Self-Expanding Peripheral March 7, 2012. Stent System (Everflex). P070004, FDA–2012–M–0250............ Sientra, Inc.......................................... SIENTRA Silicone Gel Breast Im- March 9, 2012. plants. II. Electronic Access LOCATION: The meeting will be held at submissions. In the process of Persons with access to the Internet the FDA White Oak Campus, 10903 considering these changes, FDA has may obtain the documents at http:// New Hampshire Ave., Bldg. 31 previously made available for comment www.fda.gov/MedicalDevices/ Conference Center, Great Room 1503, versions of documents that support ProductsandMedicalProcedures/ Silver Spring, MD 20993. The following making regulatory submissions in DeviceApprovalsandClearances/ link contains public meeting attendee electronic format using the (eCTD) information as well as frequently asked PMAApprovals/default.htm and http:// specifications. These draft documents questions and answers regarding public www.fda.gov/MedicalDevices/ represented FDA’s major updates to meetings at White Oak: http:// ProductsandMedicalProcedures/ Module 1 of the eCTD based on www.fda.gov/AboutFDA/ DeviceApprovalsandClearances/ previous comments. -

Rifaximin (XIFAXAN)
Rifaximin (XIFAXAN) for Irritable Bowel Syndrome with Diarrhea National Drug Monograph March 2016 VA Pharmacy Benefits Management Services, Medical Advisory Panel, and VISN Pharmacist Executives The purpose of VA PBM Services drug monographs is to provide a focused drug review for making formulary decisions. Updates will be made when new clinical data warrant additional formulary discussion. Documents will be placed in the Archive section when the information is deemed to be no longer current. FDA Approval Information Description/Mechanism of Minimally absorbed, broad-spectrum antibacterial that inhibits bacterial RNA Action synthesis. The specific mechanism of action of rifaximin in irritable bowel syndrome (IBS) has not been determined. The most likely mechanism of rifaximin is reduction in overall bacterial load, particularly in the large bowel1; however, rifaximin also seems to modulate gut microenvironment and produce cytoprotective effects.2 Indication(s) Under Review in Treatment of IBS with diarrhea (IBS-D) in adults this Document Dosage Form(s) Under 550 mg tablet Review REMS REMS No REMS Postmarketing Requirements Pregnancy Rating No data available on pregnant women to inform any drug associated risks. Executive Summary Efficacy Rifaximin had a small, statistically significant beneficial effect relative to placebo in global IBS symptom response using pooled data: 40.7% vs. 31.7%, with a difference of 9.0 percentage points, p < 0.001; NNT = 11. Rifaximin had a small, statistically significant beneficial effect relative to placebo in terms of the response rate for adequate relief of bloating (the key secondary efficacy measure): 40.2% vs. 30.3%, difference of 9.9 percentage points, p < 0.001; NNT = 10 (pooled results). -

Pharmacology and Therapeutics of Bronchodilators
1521-0081/12/6403-450–504$25.00 PHARMACOLOGICAL REVIEWS Vol. 64, No. 3 Copyright © 2012 by The American Society for Pharmacology and Experimental Therapeutics 4580/3762238 Pharmacol Rev 64:450–504, 2012 ASSOCIATE EDITOR: DAVID R. SIBLEY Pharmacology and Therapeutics of Bronchodilators Mario Cazzola, Clive P. Page, Luigino Calzetta, and M. Gabriella Matera Department of Internal Medicine, Unit of Respiratory Clinical Pharmacology, University of Rome ‘Tor Vergata,’ Rome, Italy (M.C., L.C.); Department of Pulmonary Rehabilitation, San Raffaele Pisana Hospital, Istituto di Ricovero e Cura a Carattere Scientifico, Rome, Italy (M.C., L.C.); Sackler Institute of Pulmonary Pharmacology, Institute of Pharmaceutical Science, King’s College London, London, UK (C.P.P., L.C.); and Department of Experimental Medicine, Unit of Pharmacology, Second University of Naples, Naples, Italy (M.G.M.) Abstract............................................................................... 451 I. Introduction: the physiological rationale for using bronchodilators .......................... 452 II. -Adrenergic receptor agonists .......................................................... 455 A. A history of the development of -adrenergic receptor agonists: from nonselective  Downloaded from adrenergic receptor agonists to 2-adrenergic receptor-selective drugs.................... 455  B. Short-acting 2-adrenergic receptor agonists........................................... 457 1. Albuterol........................................................................ 457 -

REVIEW Genotoxic and Carcinogenic Effects of Gastrointestinal Drugs
Mutagenesis vol. 25 no. 4 pp. 315–326, 2010 doi:10.1093/mutage/geq025 Advance Access Publication 17 May 2010 REVIEW Genotoxic and carcinogenic effects of gastrointestinal drugs Giovanni Brambilla*, Francesca Mattioli and a further in vivo test using a tissue other than the bone marrow/ Antonietta Martelli peripheral blood should be done. Guidelines for carcinogenic- Department of Internal Medicine, Division of Clinical Pharmacology and ity testing of pharmaceuticals (4,5) indicate that a long-term Toxicology, University of Genoa, Viale Benedetto XV 2, I-16132 Genoa, Italy carcinogenicity study plus a short- or medium-term in vivo system should be performed for all pharmaceuticals whose expected clinical use is continuous for at least 6 months as *To whom correspondence should be addressed. Tel: +39 010 353 8800; well as for pharmaceuticals used frequently in an intermittent Fax: þ39 010 353 8232; Email: [email protected] manner in the treatment of chronic recurrent conditions. In the Received on January 28, 2010; revised on March 23, 2010; absence of clear evidence favouring one species, the rat should accepted on April 13, 2010 be selected. In long-term carcinogenicity assays, the highest This review provides a compendium of retrievable results dose should be at least .25-fold, on a milligram per square of genotoxicity and carcinogenicity assays performed on meter basis, than the maximum recommended human daily marketed gastrointestinal drugs. Of the 71 drugs consid- dose or represent a 25-fold ratio of rodent to human area under ered, 38 (53.5%) do not have retrievable data, whereas the curve. The maximum tolerated dose (MTD) or a limit dose the other 33 (46.5%) have at least one genotoxicity or of 2000 mg/kg can be used as alternatives. -

2021 Five-Tier Formulary Benefit
KAISER PERMANENTE OF GEORGIA 2021 FIVE-TIER FORMULARY BENEFIT This document includes Kaiser Permanente Georgia’s 5 Tier Plan Benefit Formulary as of September 9, 2021. For an updated formulary, please visit our website at members.kp.org or call 1-888-865-5813, Monday through Friday 7:00 a.m. to 7:00 p.m. TTY/TDD users should call 1-800-255-0056. What is the Kaiser Permanente Drug Brand-name drugs are capitalized in the Formulary? formulary (e.g., FLOVENT). A formulary is a list of drugs determined to There are two easy ways to find your drug be safe and effective for our members by within the formulary: our Pharmacy and Therapeutics Committee. Use of formulary drugs enables Kaiser Medical Condition Permanente to provide optimal care to you The drug list begins on page 4. The drugs and your family at reasonable costs. Kaiser on this formulary are grouped into Permanente continually updates the categories depending on the type of formulary throughout the year based on medical condition that they are used to new medical evidence, considering the treat. For example, drugs used to treat a recommendations of appropriate physician heart condition are listed under the experts. category, “Cardiovascular Drugs.” If you know what your drug is used for, simply Does the formulary ever change? look for the category name in the list that Yes, Kaiser Permanente continually updates begins on page 4. Then look under the the formulary based on new medical category name for your drug. evidence, considering the recommendations of appropriate physician Alphabetical Index experts and notifies our doctors, If you are not sure what category to look pharmacists, and other clinicians about any under, you can look for the drug in the changes.