Heart Procedures Glossary
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Clinical Excellence in Cardiology
Clinical Excellence in Cardiology Roy C. Ziegelstein, MD* A recent study identified 7 domains of clinical excellence on the basis of interviews with “clinically excellent” physicians at academic institutions in the United States: (1) commu- nication and interpersonal skills, (2) professionalism and humanism, (3) diagnostic acu- men, (4) skillful negotiation of the health care system, (5) knowledge, (6) taking a scholarly approach to clinical practice, and (7) having passion for clinical medicine. What constitutes clinical excellence in cardiology has not previously been defined. The author discusses clinical excellence in cardiology using the framework of these 7 domains and also considers the additional domain of clinical experience. Specific aspects of the domains of clinical excellence that are of greatest relevance to cardiology are highlighted. In conclusion, this discussion characterizes what constitutes clinical excellence in cardiology and should stimulate additional discussion of the topic and an examination of how the domains of clinical excellence in cardiology are related to specific patient outcomes. © 2011 Elsevier Inc. All rights reserved. (Am J Cardiol 2011;108:607–611) On the basis of interviews with 24 academic physicians and clinical excellence has not been clearly demonstrated. deemed “clinically excellent,” Christmas et al1 identified 7 For example, the compliance of hospitals with performance domains of clinical excellence relevant to all disciplines in measures is not associated with improved heart failure out- medicine: (1) communication and interpersonal skills, (2) comes.10,11 The speed with which an interventional cardi- professionalism and humanism, (3) diagnostic acumen, (4) ologist achieves reperfusion of the culprit vessel, the so- skillful negotiation of the health care system, (5) knowl- called door-to-balloon time, is an important performance edge, (6) taking a scholarly approach to clinical practice, measure in the treatment of patients with acute ST-segment and (7) having passion for clinical medicine. -

Anemia in Heart Failure - from Guidelines to Controversies and Challenges
52 Education Anemia in heart failure - from guidelines to controversies and challenges Oana Sîrbu1,*, Mariana Floria1,*, Petru Dascalita*, Alexandra Stoica1,*, Paula Adascalitei, Victorita Sorodoc1,*, Laurentiu Sorodoc1,* *Grigore T. Popa University of Medicine and Pharmacy; Iasi-Romania 1Sf. Spiridon Emergency Hospital; Iasi-Romania ABSTRACT Anemia associated with heart failure is a frequent condition, which may lead to heart function deterioration by the activation of neuro-hormonal mechanisms. Therefore, a vicious circle is present in the relationship of heart failure and anemia. The consequence is reflected upon the pa- tients’ survival, quality of life, and hospital readmissions. Anemia and iron deficiency should be correctly diagnosed and treated in patients with heart failure. The etiology is multifactorial but certainly not fully understood. There is data suggesting that the following factors can cause ane- mia alone or in combination: iron deficiency, inflammation, erythropoietin levels, prescribed medication, hemodilution, and medullar dysfunc- tion. There is data suggesting the association among iron deficiency, inflammation, erythropoietin levels, prescribed medication, hemodilution, and medullar dysfunction. The main pathophysiologic mechanisms, with the strongest evidence-based medicine data, are iron deficiency and inflammation. In clinical practice, the etiology of anemia needs thorough evaluation for determining the best possible therapeutic course. In this context, we must correctly treat the patients’ diseases; according with the current guidelines we have now only one intravenous iron drug. This paper is focused on data about anemia in heart failure, from prevalence to optimal treatment, controversies, and challenges. (Anatol J Cardiol 2018; 20: 52-9) Keywords: anemia, heart failure, intravenous iron, ferric carboxymaltose, quality of life Introduction g/dL in men) (2). -

Your Pulse and Target Heart Rate
Skip to main content ×Close Menu We use cookies to improve your experience on our website. By closing this banner or interacting with our site, you acknowledge and agree to this. Legal Notices MobileClose Menu Find A Doctor Your Visit Pay a Bill Log in to MyGillette Learn more about MyGillette Patient Education Patient Services and Resources Your Rights and Medical Records Understanding Costs, Insurance and the Gillette Assistance Programs Services to Support Your Family Interpreter Services International Patients Parent Resources and Support Prepare for Your Visit Prepare for Clinic Visits and Tests Prepare for Surgery Take a Hospital Tour Transfer Your Medical Records Transportation and Accommodations Ways to Prepare and Comfort Your Child During Your Visit or Hospital Stay Commitment to a Safe and Healing Environment Our Hospital Units Your Hospital Room St. Paul Campus Amenities and Activities Visit or Contact a Patient Conditions & Care All Conditions Cerebral Palsy Neuromuscular Disorders Scoliosis Craniosynostosis Brain Injury All Tests & Treatments Shunt Surgery for Hydrocephalus Gait and Motion Analysis Selective Dorsal Rhizotomy (SDR) Gillette Craniocap© Orthosis Botulinum Toxin and Phenol (Injected Spasticity Medications) All Specialties & Services Orthopedics Rehabilitation Services Craniofacial and Plastic Surgery Neurology Neurosurgery Virtual Visits Pediatric Expert Consults Virtual Rehab Therapy Sleep Medicine Virtual Care Get Involved Advocating for Your Family Community Health United Cerebral Palsy of MN Donors & Supporters -

Training in Nuclear Cardiology
JOURNAL OF THE AMERICAN COLLEGE OF CARDIOLOGY VOL.65,NO.17,2015 ª 2015 BY THE AMERICAN COLLEGE OF CARDIOLOGY FOUNDATION ISSN 0735-1097/$36.00 PUBLISHED BY ELSEVIER INC. http://dx.doi.org/10.1016/j.jacc.2015.03.019 TRAINING STATEMENT COCATS 4 Task Force 6: Training in Nuclear Cardiology Endorsed by the American Society of Nuclear Cardiology Vasken Dilsizian, MD, FACC, Chair Todd D. Miller, MD, FACC James A. Arrighi, MD, FACC* Allen J. Solomon, MD, FACC Rose S. Cohen, MD, FACC James E. Udelson, MD, FACC, FASNC 1. INTRODUCTION ACC and ASNC, and addressed their comments. The document was revised and posted for public comment 1.1. Document Development Process from December 20, 2014, to January 6, 2015. Authors 1.1.1. Writing Committee Organization addressed additional comments from the public to complete the document. The final document was The Writing Committee was selected to represent the approved by the Task Force, COCATS Steering Com- American College of Cardiology (ACC) and the Amer- mittee, and ACC Competency Management Commit- ican Society of Nuclear Cardiology (ASNC) and tee; ratified by the ACC Board of Trustees in March, included a cardiovascular training program director; a 2015; and endorsed by the ASNC. This document is nuclear cardiology training program director; early- considered current until the ACC Competency Man- career experts; highly experienced specialists in agement Committee revises or withdraws it. both academic and community-based practice set- tings; and physicians experienced in defining and applying training standards according to the 6 general 1.2. Background and Scope competency domains promulgated by the Accredita- Nuclear cardiology provides important diagnostic and tion Council for Graduate Medical Education (ACGME) prognostic information that is an essential part of the and American Board of Medical Specialties (ABMS), knowledge base required of the well-trained cardiol- and endorsed by the American Board of Internal ogist for optimal management of the cardiovascular Medicine (ABIM). -

The Heart Institute
The Heart Institute Division of Cardiology 4650 Sunset Blvd., #34, Los Angeles, CA 90027 Phone: 323-361-2461 Fax: 323-361-1513 The Heart Institute at Children’s Hospital Los Angeles is CHLA.org/CARDIOLOGY one of the top-ranked pediatric heart programs in the Division of nation—with a long history of exceptional and innovative Cardiothoracic Surgery 4650 Sunset Blvd., #66 care for the most complex pediatric cardiac conditions. Los Angeles, CA 90027 Phone: 323-361-4148 Fax: 323-361-3668 We treat patients from fetus to adulthood and serve as CHLA.org/CTSurgery a major tertiary referral center for all forms of congenital Referrals Phone: 888-631-2452 and acquired heart disease. Fax: 323-361-8988 Email: [email protected] Physician Portal: https://myCHLA.CHLA.org We offer an integrated inpatient and outpatient Our Cardiothoracic Intensive Care Unit (CTICU) complement of services that brings together experts was the first of its kind on the West Coast, using in cardiology, cardiothoracic surgery, cardiothoracic innovative treatments including extracorporeal transplant, cardiothoracic intensive care and membrane oxygenation (ECMO) and ventricular cardiovascular acute care in a centrally located, assist services. state-of-the-art healing environment. With fewer steps to navigate, our patients and families receive care Our two state-of-the-art catheterization laboratories that is more streamlined and less stressful. use the latest technology to provide accurate cardiac data while reducing radiation. Our programmatic emphasis on high-complexity surgeries in neonates has produced outcomes that are among the best in the country, as shown in the most recent Society of Thoracic Surgeons report. -

Essentials of Cardiology Timothy C
Th e Heart SECTION IV Essentials of Cardiology Timothy C. Slesnick, Ralph Gertler, and CHAPTER 14 Wanda C. Miller-Hance Congenital Heart Disease Evaluation of the Patient with a Cardiac Murmur Incidence Basic Interpretation of the Pediatric Segmental Approach to Diagnosis Electrocardiogram Physiologic Classifi cation of Defects Essentials of Cardiac Rhythm Interpretation and Acute Arrhythmia Management in Children Acquired Heart Disease Basic Rhythms Cardiomyopathies Conduction Disorders Myocarditis Cardiac Arrhythmias Rheumatic Fever and Rheumatic Heart Disease Pacemaker Therapy in the Pediatric Age Group Infective Endocarditis Pacemaker Nomenclature Kawasaki Disease Permanent Cardiac Pacing Cardiac Tumors Diagnostic Modalities in Pediatric Cardiology Heart Failure in Children Chest Radiography Defi nition and Pathophysiology Barium Swallow Etiology and Clinical Features Echocardiography Treatment Strategies Magnetic Resonance Imaging Syndromes, Associations, and Systemic Disorders: Cardiovascular Disease and Anesthetic Implications Computed Tomography Chromosomal Syndromes Cardiac Catheterization and Angiography Gene Deletion Syndromes Considerations in the Perioperative Care of Children with Cardiovascular Disease Single-Gene Defects General Issues Associations Clinical Condition and Status of Prior Repair Other Disorders Summary Selected Vascular Anomalies and Their Implications for Anesthetic Care Aberrant Subclavian Arteries Persistent Left Superior Vena Cava to Coronary Sinus Communication Congenital Heart Disease adulthood has become the expectation for most congenital car- diovascular malformations.3 At present it is estimated that there Incidence are more than a million adults with CHD in the United States, Estimates of the incidence of congenital heart disease (CHD) surpassing the number of children similarly aff ected for the fi rst range from 0.3% to 1.2% in live neonates.1 Th is represents the time in history. -

Bed-Based Ballistocardiography: Dataset and Ability to Track Cardiovascular Parameters
sensors Article Bed-Based Ballistocardiography: Dataset and Ability to Track Cardiovascular Parameters Charles Carlson 1,* , Vanessa-Rose Turpin 2, Ahmad Suliman 1 , Carl Ade 2, Steve Warren 1 and David E. Thompson 1 1 Mike Wiegers Department of Electrical and Computer Engineering, Kansas State University, Manhattan, KS 66506, USA; [email protected] (A.S.); [email protected] (S.W.); [email protected] (D.E.T.) 2 Department of Kinesiology, Kansas State University, Manhattan, KS 66506, USA; [email protected] (V.-R.T.); [email protected] (C.A.) * Correspondence: [email protected] Abstract: Background: The goal of this work was to create a sharable dataset of heart-driven signals, including ballistocardiograms (BCGs) and time-aligned electrocardiograms (ECGs), photoplethysmo- grams (PPGs), and blood pressure waveforms. Methods: A custom, bed-based ballistocardiographic system is described in detail. Affiliated cardiopulmonary signals are acquired using a GE Datex CardioCap 5 patient monitor (which collects ECG and PPG data) and a Finapres Medical Systems Finometer PRO (which provides continuous reconstructed brachial artery pressure waveforms and derived cardiovascular parameters). Results: Data were collected from 40 participants, 4 of whom had been or were currently diagnosed with a heart condition at the time they enrolled in the study. An investigation revealed that features extracted from a BCG could be used to track changes in systolic blood pressure (Pearson correlation coefficient of 0.54 +/− 0.15), dP/dtmax (Pearson correlation coefficient of 0.51 +/− 0.18), and stroke volume (Pearson correlation coefficient of 0.54 +/− 0.17). Conclusion: A collection of synchronized, heart-driven signals, including BCGs, ECGs, PPGs, and blood pressure waveforms, was acquired and made publicly available. -

Cocats 4 (Pdf)
JOURNAL OF THE AMERICAN COLLEGE OF CARDIOLOGY VOL. 65, NO. 17, 2015 ª 2015 BY THE AMERICAN COLLEGE OF CARDIOLOGY FOUNDATION ISSN 0735-1097/$36.00 PUBLISHED BY ELSEVIER INC. http://dx.doi.org/10.1016/j.jacc.2015.03.017 TRAINING STATEMENT ACC 2015 Core Cardiovascular Training Statement (COCATS 4) (Revision of COCATS 3) A Report of the ACC Competency Management Committee Task Force Introduction/Steering Committee Task Force 3: Training in Electrocardiography, Members Jonathan L. Halperin, MD, FACC Ambulatory Electrocardiography, and Exercise Testing (and Society Eric S. Williams, MD, MACC Gary J. Balady, MD, FACC, Chair Representation) Valentin Fuster, MD, PHD, MACC Vincent J. Bufalino, MD, FACC Martha Gulati, MD, MS, FACC Task Force 1: Training in Ambulatory, Jeffrey T. Kuvin, MD, FACC Consultative, and Longitudinal Cardiovascular Care Lisa A. Mendes, MD, FACC Valentin Fuster, MD, PHD, MACC, Co-Chair Joseph L. Schuller, MD Jonathan L. Halperin, MD, FACC, Co-Chair Eric S. Williams, MD, MACC, Co-Chair Task Force 4: Training in Multimodality Imaging Nancy R. Cho, MD, FACC Jagat Narula, MD, PHD, MACC, Chair William F. Iobst, MD* Y.S. Chandrashekhar, MD, FACC Debabrata Mukherjee, MD, FACC Vasken Dilsizian, MD, FACC Prashant Vaishnava, MD Mario J. Garcia, MD, FACC Christopher M. Kramer, MD, FACC Task Force 2: Training in Preventive Shaista Malik, MD, PHD, FACC Cardiovascular Medicine Thomas Ryan, MD, FACC Sidney C. Smith, JR, MD, FACC, Chair Soma Sen, MBBS, FACC Vera Bittner, MD, FACC Joseph C. Wu, MD, PHD, FACC J. Michael Gaziano, MD, FACC John C. Giacomini, MD, FACC Quinn R. Pack, MD Donna M. -
Heart Failure
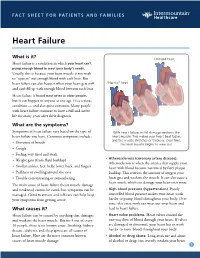
FACT SHEET FOR PATIENTS AND FAMILIES Heart Failure What is it? Enlarged heart Heart failure is a condition in which your heart can’t pump enough blood to meet your body’s needs. Usually, this is because your heart muscle is too weak to “squeeze” out enough blood with each beat. But heart failure can also happen when your heart gets stiff “Normal” heart and can’t fill up with enough blood between each beat. Heart failure is found most often in older people, but it can happen to anyone at any age. It’s a serious condition — and also quite common. Many people with heart failure continue to have a full and active life for many years after their diagnosis. What are the symptoms? Symptoms of heart failure vary based on the type of With heart failure, initial damage weakens the heart failure you have. Common symptoms include: heart muscle. This makes your heart beat faster, and the muscle stretches or thickens. Over time, • Shortness of breath the heart muscle begins to wear out. • Cough • Feeling very tired and weak • Atherosclerosis (coronary artery disease). • Weight gain (from fluid buildup) Atherosclerosis is when the arteries that supply your • Swollen ankles, feet, belly, lower back, and fingers heart with blood become narrowed by fatty plaque • Puffiness or swelling around the eyes buildup. This restricts the amount of oxygen your • Trouble concentrating or remembering heart gets and weakens the muscle. It can also cause a heart attack, which can damage your heart even more. The main cause of heart failure (heart muscle damage and weakness) cannot be cured, but symptoms can be • High blood pressure (hypertension). -

Grade 6: the Heart and Circulatory System Lesson 1: the Heart Lesson 2: the Heart Rate Lesson 3: the Circulatory System and Blood
Grade 6: The Heart and Circulatory System Lesson 1: The Heart Lesson 2: The Heart Rate Lesson 3: The Circulatory System and Blood Objectives: 1. Students will identify the four chambers of the heart 2. Students will identify four important structures of the Circulatory System and what they do. 3. Students will explain heart rate and be able to take their resting and active heart rates. 4. Students will describe the major functions of the Circulatory System. 5. Students will explain the role of the heart in circulation 6. Students will give a basic explanation of the cardio-pulmonary sequence. 7. Students will describe systemic circulation. Materials: Lesson 1: • Animal heart (Example: cow, pig, sheep) • Note cards • Picture of the heart (See Figure 1) • Dissection tools (Scissors, pan, etc.) Lesson 2: • Small drum • Watch or clock with second hand, or time • Optional: Stethoscope Lesson 3: • Corn Syrup • Plastic Beads: flat red disks, white ovals, green or blue seed beads • “Explain” experiment (per group): o Two small balloons or large finger cots o One clear tube (1/2” diameter) about 8” long o One clear tube (3/4” diameter) about 8” long o 16 - 20 oz. water o Red food coloring o Measuring cup o Funnel o Two empty plastic containers (such as cottage cheese or yogurt cartons) Activity Summary: In this lesson students will learn the basic functioning of the heart, Circulatory System and blood, the connection to lung functioning, and the activity of the Grade 6: The Heart & Circulatory System – Revised 2008 Page 1 Circulatory System in the body. -

Basic Cardiac Rhythms – Identification and Response Module 1 ANATOMY, PHYSIOLOGY, & ELECTRICAL CONDUCTION Objectives
Basic Cardiac Rhythms – Identification and Response Module 1 ANATOMY, PHYSIOLOGY, & ELECTRICAL CONDUCTION Objectives ▪ Describe the normal cardiac anatomy and physiology and normal electrical conduction through the heart. ▪ Identify and relate waveforms to the cardiac cycle. Cardiac Anatomy ▪ 2 upper chambers ▪ Right and left atria ▪ 2 lower chambers ▪ Right and left ventricle ▪ 2 Atrioventricular valves (Mitral & Tricuspid) ▪ Open with ventricular diastole ▪ Close with ventricular systole ▪ 2 Semilunar Valves (Aortic & Pulmonic) ▪ Open with ventricular systole ▪ Open with ventricular diastole The Cardiovascular System ▪ Pulmonary Circulation ▪ Unoxygenated – right side of the heart ▪ Systemic Circulation ▪ Oxygenated – left side of the heart Anatomy Coronary Arteries How The Heart Works Anatomy Coronary Arteries ▪ 2 major vessels of the coronary circulation ▪ Left main coronary artery ▪ Left anterior descending and circumflex branches ▪ Right main coronary artery ▪ The left and right coronary arteries originate at the base of the aorta from openings called the coronary ostia behind the aortic valve leaflets. Physiology Blood Flow Unoxygenated blood flows from inferior and superior vena cava Right Atrium Tricuspid Valve Right Ventricle Pulmonic Valve Lungs Through Pulmonary system Physiology Blood Flow Oxygenated blood flows from the pulmonary veins Left Atrium Mitral Valve Left Ventricle Aortic Valve Systemic Circulation ▪ Blood Flow Through The Heart ▪ Cardiology Rap Physiology ▪ Cardiac cycle ▪ Represents the actual time sequence between -

682.Full.Pdf
Endogenous and nitrovasodilator-induced release of NO in the airways of end-stage cystic fibrosis patients To the Editors: blood pressure changes recorded, as described previously [8] and in the online supplementary material. A variety of isoforms of nitric oxide (NO) synthases are constitutively expressed in human airway and vascular Nearly undetectable levels of NO were found in CF patients endothelial cells continuously generating NO. NO plays an representing an output of 7.6¡6 ppb over 30 s. This is in important role in regulating lung function in health and contrast to patients presented for routine open heart surgery disease including modulation of pulmonary vascular resis- (91.4¡21 ppb over 30 s; fig. 1). Representative traces are tance, airway calibre and host defence. Production of NO and shown in figure 1A and C of the online supplementary its consumption by fluid-phase reactions can be detected and material. monitored in the exhaled air, providing an important window There was a significant increase in gas-phase NO above baseline to assess the dynamics of NO metabolism in health and levels by 250 mg GTN boluses in CF patients (36.7¡6ppb), inflammatory lung conditions, asthma in particular [1]. which was comparable to that seen in control patients with A series of milestone studies uncovered a relative deficiency of routine open heart surgery (48.7¡4 ppb; fig. 1). Representative pulmonary NO availability in cystic fibrosis (CF), a severe traces of GTN-induced exhaled NO are presented in figure 1B chronic inflammatory lung disease with studies generally and D of the online supplementary material.