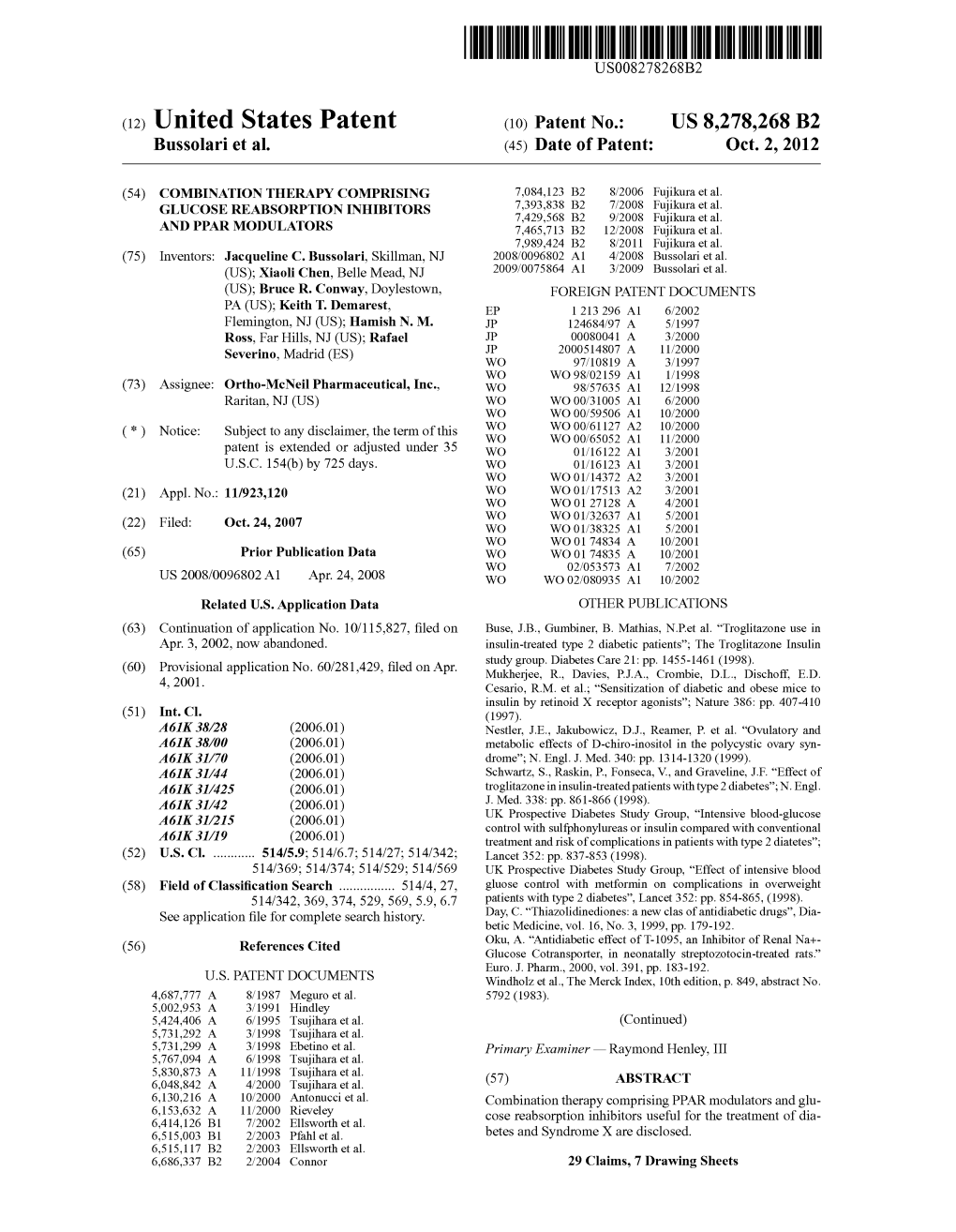
(12) United States Patent (10) Patent No.: US 8,278.268 B2 Bussolariet Al
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Type 2 Diabetes Mellitus: a Review of Multi-Target Drugs
Molecules 2020, 25, 1987 1 of 20 Review Type 2 Diabetes Mellitus: A Review of Multi-Target Drugs Angelica Artasensi, Alessandro Pedretti, Giulio Vistoli and Laura Fumagalli * Dipartimento di Scienze Farmaceutiche, University Degli Studi di Milano, 20133 Milano, Italy; [email protected] (A.A.); [email protected] (A.P.); [email protected] (G.V.) * Correspondence: [email protected]; Tel.: +39-02-5031-9303 Academic Editor: Massimo Bertinaria, Derek J. McPhee Received: 01 April 2020; Accepted: 21 April 2020; Published: 23 April 2020 Abstract: Diabetes Mellitus (DM) is a multi-factorial chronic health condition that affects a large part of population and according to the World Health Organization (WHO) the number of adults living with diabetes is expected to increase. Since type 2 diabetes mellitus (T2DM) is suffered by the majority of diabetic patients (around 90–95%) and often the mono-target therapy fails in managing blood glucose levels and the other comorbidities, this review focuses on the potential drugs acting on multi-targets involved in the treatment of this type of diabetes. In particular, the review considers the main systems directly involved in T2DM or involved in diabetes comorbidities. Agonists acting on incretin, glucagon systems, as well as on peroxisome proliferation activated receptors are considered. Inhibitors which target either aldose reductase and tyrosine phosphatase 1B or sodium glucose transporters 1 and 2 are taken into account. Moreover, with a view at the multi-target approaches for T2DM some phytocomplexes are also discussed. Keywords: diabetes mellitus; type 2 diabetes mellitus; multi-target compounds; multi-target drugs 1. -

CDR Clinical Review Report for Soliqua
CADTH COMMON DRUG REVIEW Clinical Review Report Insulin glargine and lixisenatide injection (Soliqua) (Sanofi-Aventis) Indication: adjunct to diet and exercise to improve glycemic control in adults with type 2 diabetes mellitus inadequately controlled on basal insulin (less than 60 units daily) alone or in combination with metformin. Service Line: CADTH Common Drug Review Version: Final (with redactions) Publication Date: January 2019 Report Length: 118 Pages Disclaimer: The information in this document is intended to help Canadian health care decision-makers, health care professionals, health systems leaders, and policy-makers make well-informed decisions and thereby improve the quality of health care services. While patients and others may access this document, the document is made available for informational purposes only and no representations or warranties are made with respect to its fitness for any particular purpose. The information in this document should not be used as a substitute for professional medical advice or as a substitute for the application of clinical judgment in respect of the care of a particular patient or other professional judgment in any decision-making process. The Canadian Agency for Drugs and Technologies in Health (CADTH) does not endorse any information, drugs, therapies, treatments, products, processes, or services. While care has been taken to ensure that the information prepared by CADTH in this document is accurate, complete, and up-to-date as at the applicable date the material was first published by CADTH, CADTH does not make any guarantees to that effect. CADTH does not guarantee and is not responsible for the quality, currency, propriety, accuracy, or reasonableness of any statements, information, or conclusions contained in any third-party materials used in preparing this document. -

The Opportunities and Challenges of Peroxisome Proliferator-Activated Receptors Ligands in Clinical Drug Discovery and Development
International Journal of Molecular Sciences Review The Opportunities and Challenges of Peroxisome Proliferator-Activated Receptors Ligands in Clinical Drug Discovery and Development Fan Hong 1,2, Pengfei Xu 1,*,† and Yonggong Zhai 1,2,* 1 Beijing Key Laboratory of Gene Resource and Molecular Development, College of Life Sciences, Beijing Normal University, Beijing 100875, China; [email protected] 2 Key Laboratory for Cell Proliferation and Regulation Biology of State Education Ministry, College of Life Sciences, Beijing Normal University, Beijing 100875, China * Correspondence: [email protected] (P.X.); [email protected] (Y.Z.); Tel.: +86-156-005-60991 (P.X.); +86-10-5880-6656 (Y.Z.) † Current address: Center for Pharmacogenetics and Department of Pharmaceutical Sciences, University of Pittsburgh, Pittsburgh, PA 15213, USA. Received: 22 June 2018; Accepted: 24 July 2018; Published: 27 July 2018 Abstract: Peroxisome proliferator-activated receptors (PPARs) are a well-known pharmacological target for the treatment of multiple diseases, including diabetes mellitus, dyslipidemia, cardiovascular diseases and even primary biliary cholangitis, gout, cancer, Alzheimer’s disease and ulcerative colitis. The three PPAR isoforms (α, β/δ and γ) have emerged as integrators of glucose and lipid metabolic signaling networks. Typically, PPARα is activated by fibrates, which are commonly used therapeutic agents in the treatment of dyslipidemia. The pharmacological activators of PPARγ include thiazolidinediones (TZDs), which are insulin sensitizers used in the treatment of type 2 diabetes mellitus (T2DM), despite some drawbacks. In this review, we summarize 84 types of PPAR synthetic ligands introduced to date for the treatment of metabolic and other diseases and provide a comprehensive analysis of the current applications and problems of these ligands in clinical drug discovery and development. -

Thiazolidinedione Drugs Down-Regulate CXCR4 Expression on Human Colorectal Cancer Cells in a Peroxisome Proliferator Activated Receptor Á-Dependent Manner
1215-1222 26/3/07 18:16 Page 1215 INTERNATIONAL JOURNAL OF ONCOLOGY 30: 1215-1222, 2007 Thiazolidinedione drugs down-regulate CXCR4 expression on human colorectal cancer cells in a peroxisome proliferator activated receptor Á-dependent manner CYNTHIA LEE RICHARD and JONATHAN BLAY Department of Pharmacology, Faculty of Medicine, Dalhousie University, Halifax, Nova Scotia, B3H 1X5, Canada Received October 26, 2006; Accepted December 4, 2006 Abstract. Peroxisome proliferator activated receptor (PPAR) Introduction Á is a nuclear receptor involved primarily in lipid and glucose metabolism. PPARÁ is also expressed in several cancer types, Peroxisome proliferator activated receptors (PPARs) are and has been suggested to play a role in tumor progression. nuclear hormone receptors that are involved primarily in PPARÁ agonists have been shown to reduce the growth of lipid and glucose metabolism (1). Upon ligand activation, colorectal carcinoma cells in culture and in xenograft models. these receptors interact with the retinoid X receptor (RXR) Furthermore, the PPARÁ agonist thiazolidinedione has been and bind to peroxisome proliferator response elements (PPREs), shown to reduce metastasis in a murine model of rectal cancer. leading to transcriptional regulation of target genes. Members Since the chemokine receptor CXCR4 has emerged as an of the thiazolidinedione class of antidiabetic drugs act as important player in tumorigenesis, particularly in the process ligands for PPARÁ (2), as does endogenously produced 15- 12,14 of metastasis, we sought to determine if PPARÁ agonists deoxy-¢ -prostaglandin J2 (15dPGJ2) (3). might act in part by reducing CXCR4 expression. We found In addition to regulation of glucose metabolism, PPARÁ that rosiglitazone, a thiazolidinedione PPARÁ agonist used appears also to be involved in tumorigenesis, although its primarily in the treatment of type 2 diabetes, significantly exact role has yet to be elucidated (4). -

Possible Role of Rivoglitazone Thiazolidine Class of Drug As Dual
Medical Hypotheses 131 (2019) 109305 Contents lists available at ScienceDirect Medical Hypotheses journal homepage: www.elsevier.com/locate/mehy Possible role of rivoglitazone thiazolidine class of drug as dual-target therapeutic agent for bacterial infections: An in silico study T ⁎ Vidyasrilekha Yele , Niladri Saha, Afzal Azam Md Department of Pharmaceutical Chemistry, JSS College of Pharmacy, Ootacamund, JSS Academy of Higher Education & Research, Mysuru 643001, India ARTICLE INFO ABSTRACT Keywords: Infections due to resistant bacteria are the life-threatening and leading cause of mortality worldwide. The Rivoglitazone current therapy for bacterial infections includes treatment with various drugs and antibiotics. The misuse and ParE over usage of these antibiotics leads to bacterial resistance. There are several mechanisms by which bacteria MurE exhibit resistance to some antibiotics. These include drug inactivation or modification, elimination of antibiotics Docking through efflux pumps, drug target alteration, and modification of metabolic pathway. However, it is difficult to MM-GBSA treat infections caused by resistant bacteria by conventional existing therapy. In the present study binding af- Molecular dynamic simulations fi Anti-bacterial agent nities of some glitazones against ParE and MurE bacterial enzymes are investigated by in silico methods. As evident by extra-precision docking and binding free energy calculation (MM-GBSA) results, rivoglitazone ex- hibited higher binding affinity against both ParE and MurE enzymes compared to all other selected compounds. Further molecular dynamic (MD) simulations were performed to validate the stability of rivoglitazone/4MOT and rivoglitazone/4C13 complexes and to get insight into the binding mode of inhibitor. Thus, we hypothesize that structural modifications of the rivoglitazone scaffold can be useful for the development of an effective antibacterial agent. -

Peroxisome Proliferator-Activated Receptors As Superior Targets to Treat Diabetic Disease, Design Strategies - Review Article
Review article DOI: 10.4274/tjps.galenos.2021.70105 Peroxisome proliferator-activated receptors as superior targets to treat diabetic disease, design strategies - review article Diyabetik hastalığı tedavi etmek için üstün hedefler olarak peroksizom proliferatör ile aktive edilmiş reseptörler, tasarım stratejileri - inceleme makalesi Mohammed T Qaoud1, Ihab Al-masri2, Tijen Önkol1 1Department of Pharmaceutical Chemistry, Faculty of Pharmacy, Gazi University, Ankara- Turkey 2Department of Pharmaceutical Chemistry and Pharmacognosy, Faculty of Pharmacy, Al Azhar University, Gaza Strip, Palestine proof Corresponding Author Mohammed T Qaoud, Department of Pharmaceutical Chemistry, Faculty of Pharmacy, Gazi University, Ankara-Turkey [email protected] +90 552 634 15 56 https://orcid.org/0000-0002-9563-9493 09.12.2020 31.05.2021 09.06.2021 Abstract Thiazolidinedione (TZD), a class of drugs that are mainly used to control type II diabetes mellitus (T2DM), acts fundamentally as a ligand of peroxisome proliferator-activated receptors (PPARs). Besides activating pathways responsible for glycemic control via enhancing insulin sensitivity and lipid homeostasis, activating PPARs leads to exciting other pathways related to bone formation, inflammation, and cell proliferation. Unfortunately, this diverse effect via activating several pathways may show in some studies adverse health outcomes as osteological, hepatic, cardiovascular, and carcinogenic effects. Thus, an argent demand is present to find and develop new active and potent antiglycemic drugs for the treatment of T2DM. To achieve this goal, the structure of TZD for research is considered as a leading structure domain. This review would guide future research in the design of novel TZD derivatives through highlighting the general modifications conducted to the structure component of TZD scaffold affecting their potency, binding efficacy, and selectivity for the control of type II diabetes mellitus. -

Tot-JNK 18S Patent Application Publication Mar
US 2010.0075894A1 (19) United States (12) Patent Application Publication (10) Pub. No.: US 2010/0075894 A1 Hotamisligil et al. (43) Pub. Date: Mar. 25, 2010 (54) REDUCINGER STRESS IN THE TREATMENT A63L/92 (2006.01) OF OBESITY AND DABETES A 6LX 3/575 (2006.01) A63/04 (2006.01) (75) Inventors: Gökhan S. Hotamisligil, Wellesley, A6II 3/55 (2006.01) MA (US); Umut Ozcan, Brookline, A613/60 (2006.01) MA (US) A6IP3/10 (2006.01) A6IP3/04 (2006.01) Correspondence Address: A6IP 9/10 (2006.01) EDWARDSANGELL PALMER & DODGE LLP (s2 usic... 514/4; 435/7.2:436/86; 514/570; P.O. BOX SS874 514/169; 514/740: 514/171; 514/635: 514/165 BOSTON, MA 02205 (US) (57) ABSTRACT (73) Assignee: HARYARPN.YERSITY, Endoplasmic reticulum stress has been found to be associated ambridge, (US) with obesity. Therefore, agents that reduce or prevent ER (21) Appl. No.: 12/541,020 stress may be used to treat diseases associated with obesity including peripheral insulin resistance, hypergylcemia, and (22) Filed: Aug. 13, 2009 type 2 diabetes. Two compounds which have been shown to reduce ER stress and to reduce blood glucose levels include Related U.S. Application Data 4-phenyl butyric acid (PBA), tauroursodeoxycholic acid (TUDCA), and trimethylamine N-oxide (TMAO). Other (63) Continuation of application No. 1 1/227.497, filed on compounds useful in reducing ER stress are chemical chap Sep. 15, 2005, now abandoned. erones Such as trimethylamine N-oxide and glycerol. The (60) Provisional application No. 60/610,093, filed on Sep. E. invention provides methods of treating a subject suf 15, 2004. -

Molecular Modeling Study of Pparγ Agonists: Dehydro-Di-Isoeugenol, Macelignan, Pioglitazone, Netoglitazone, and Rosiglitazone As Antidiabetic Drugs
International Journal of Chemistry; Vol. 6, No. 2; 2014 ISSN 1916-9698 E-ISSN 1916-9701 Published by Canadian Center of Science and Education Molecular Modeling Study of PPARγ Agonists: Dehydro-Di-Isoeugenol, Macelignan, Pioglitazone, Netoglitazone, and Rosiglitazone as Antidiabetic Drugs Nyi Mekar Saptarini1, Febrina Amelia Saputri1 & Jutti Levita1 1 Faculty of Pharmacy, Padjadjaran University, West Java, Indonesia Correspondence: Nyi Mekar Saptarini, Faculty of Pharmacy, Padjadjaran University, Jl. Raya Bandung-Sumedang Km.21 Jatinangor Sumedang, West Java 45363, Indonesia. Tel: 62-815-607-8248. Fax: 62- 227-796-200. E-mail: [email protected] Received: February 23, 2014 Accepted: April 2, 2014 Online Published: April 14, 2014 doi:10.5539/ijc.v6n2p48 URL: http://dx.doi.org/10.5539/ijc.v6n2p48 Abstract The peroxisome proliferator-activated receptors (PPARs) are ligand-activated trasncription factors belonging to the nuclear receptor family. The objective of this study is to analyze the molecular aspects of PPARγ agonists which used to design of new antidiabetic drugs. The analysis method was comparing the interactions of ligands in the ligand binding domain of the PPARγ. This analysis showed that most known agonists of PPARγ interacted via hydrogen bond with Tyr473. Pioglitazone showed three hydrogen bonds with His323 and Tyr473. Netoglitazone showed four hydrogen bonds with Ser289, His323, His449, and Tyr473. Rosiglitazone showed five hydrogen bonds with Ser289, His323, His449, and Tyr473. AZ72, an agonist of PPARα and γ showed five hydrogen bonds with Ser289, His323, His449, and Tyr473. Molecular modeling was performed by redocking pioglitazone and rosiglitazone using AutoDock Vina. Docking showed that both pioglitazone (Ki 0.22 μM) and rosiglitazone (Ki 0.70 μM) occupied their origin sites and interacted with Tyr473. -

Stembook 2018.Pdf
The use of stems in the selection of International Nonproprietary Names (INN) for pharmaceutical substances FORMER DOCUMENT NUMBER: WHO/PHARM S/NOM 15 WHO/EMP/RHT/TSN/2018.1 © World Health Organization 2018 Some rights reserved. This work is available under the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 IGO licence (CC BY-NC-SA 3.0 IGO; https://creativecommons.org/licenses/by-nc-sa/3.0/igo). Under the terms of this licence, you may copy, redistribute and adapt the work for non-commercial purposes, provided the work is appropriately cited, as indicated below. In any use of this work, there should be no suggestion that WHO endorses any specific organization, products or services. The use of the WHO logo is not permitted. If you adapt the work, then you must license your work under the same or equivalent Creative Commons licence. If you create a translation of this work, you should add the following disclaimer along with the suggested citation: “This translation was not created by the World Health Organization (WHO). WHO is not responsible for the content or accuracy of this translation. The original English edition shall be the binding and authentic edition”. Any mediation relating to disputes arising under the licence shall be conducted in accordance with the mediation rules of the World Intellectual Property Organization. Suggested citation. The use of stems in the selection of International Nonproprietary Names (INN) for pharmaceutical substances. Geneva: World Health Organization; 2018 (WHO/EMP/RHT/TSN/2018.1). Licence: CC BY-NC-SA 3.0 IGO. Cataloguing-in-Publication (CIP) data. -

A Abacavir Abacavirum Abakaviiri Abagovomab Abagovomabum
A abacavir abacavirum abakaviiri abagovomab abagovomabum abagovomabi abamectin abamectinum abamektiini abametapir abametapirum abametapiiri abanoquil abanoquilum abanokiili abaperidone abaperidonum abaperidoni abarelix abarelixum abareliksi abatacept abataceptum abatasepti abciximab abciximabum absiksimabi abecarnil abecarnilum abekarniili abediterol abediterolum abediteroli abetimus abetimusum abetimuusi abexinostat abexinostatum abeksinostaatti abicipar pegol abiciparum pegolum abisipaaripegoli abiraterone abirateronum abirateroni abitesartan abitesartanum abitesartaani ablukast ablukastum ablukasti abrilumab abrilumabum abrilumabi abrineurin abrineurinum abrineuriini abunidazol abunidazolum abunidatsoli acadesine acadesinum akadesiini acamprosate acamprosatum akamprosaatti acarbose acarbosum akarboosi acebrochol acebrocholum asebrokoli aceburic acid acidum aceburicum asebuurihappo acebutolol acebutololum asebutololi acecainide acecainidum asekainidi acecarbromal acecarbromalum asekarbromaali aceclidine aceclidinum aseklidiini aceclofenac aceclofenacum aseklofenaakki acedapsone acedapsonum asedapsoni acediasulfone sodium acediasulfonum natricum asediasulfoninatrium acefluranol acefluranolum asefluranoli acefurtiamine acefurtiaminum asefurtiamiini acefylline clofibrol acefyllinum clofibrolum asefylliiniklofibroli acefylline piperazine acefyllinum piperazinum asefylliinipiperatsiini aceglatone aceglatonum aseglatoni aceglutamide aceglutamidum aseglutamidi acemannan acemannanum asemannaani acemetacin acemetacinum asemetasiini aceneuramic -

Current Pharma Research ISSN: 2230-7842 CPR 3(2), 2013, 846-854
Review Article Current Pharma Research ISSN: 2230-7842 CPR 3(2), 2013, 846-854. PPAR Dual Agonist: In Treatment of Type II Diabetes. *1Kishan Patel, 1R. N. Sharma, 1L. J. Patel, 2G. M. Patel 1S. K. Patel College of Pharmaceutical Education and Research, Ganpat University, Mehsana-Gozaria Highway, Kherva, Gujarat, India, 2K. B. Institute of Pharmaceutical Education and Research, Gandhinagar, Gujarat, India. Abstract Peroxisome proliferator-activated receptors (PPARs) are central regulators of lipoprotein metabolism and glucose homeostasis that are considered particularly useful for improving glycemic control and co morbidities in patients with type II diabetes mellitus. Clinical trials of PPAR-α agonists have demonstrated efficacy in reducing cardiovascular events; however, these benefits have been confined to subgroups of patients with low levels of high-density lipoprotein cholesterol or high levels of triglycerides. While activators of PPAR-γ reduce early atherosclerotic lesions and reduce cardiovascular events, these agents have the effect of increasing fluid retention in patients, which results in more hospitalizations for congestive heart failure. The PPAR α / γ dual agonists are developed to increase insulin sensitivity and simultaneously prevent diabetic cardiovascular complications. Such compounds are under clinical trials and proposed for treatment of type II diabetes with secondary cardiovascular complications. However, PPAR α / γ dual agonists such as muraglitazar, tesaglitazar and ragaglitazar have been noted to produce several cardiovascular risks and carcinogenicity, which raised number of questions about the clinical applications of dual agonists in diabetes and its associated complications. Therefore future studies of PPAR-γ agonists or dual PPAR-α/γ agonists will require further delineation of the risk profile to avoid adverse outcomes in susceptible patients. -

Approach to a Safer Insulin Sensitizer
Hindawi Publishing Corporation PPAR Research Volume 2008, Article ID 936906, 9 pages doi:10.1155/2008/936906 Review Article The Development of INT131 as a Selective PPARγ Modulator: Approach to a Safer Insulin Sensitizer Linda S. Higgins1 and Christos S. Mantzoros2 1 InteKrin Therapeutics, Inc., 4300 El Camino Real, Suite 201, Los Altos, CA 94022, USA 2 Division of Endocrinology, Diabetes and Metabolism, Beth Israel Deaconess Medical Center, Harvard Medical School, Boston, MA 02215, USA Correspondence should be addressed to Linda S. Higgins, [email protected] Received 18 March 2008; Accepted 14 June 2008 Recommended by Anne Miller INT131 (formerly T0903131, T131, AMG131) is a potent non-thiazolidinedione (TZD) selective peroxisome proliferator-activated receptor γ modulator (SPPARM) currently in Phase 2 clinical trials for treatment of type-2 diabetes mellitus (T2DM). This new chemical entity represents a second generation SPPARM approach developed after the first generation PPARγ full agonists to address their inherent limitations. INT131 was specifically and carefully designed using preclinical models to exhibit a biological profile of strong efficacy with de minimis side effects compared to PPARγ full agonists. As a potent PPARγ modulator, INT131 binds to PPARγ with high affinity. In pharmacology models of diabetes and in early clinical studies, it achieved a high level of efficacy in terms of antidiabetic actions such as insulin sensitization and glucose and insulin lowering, but had little activity in terms of other, undesired, effects associated with TZD PPARγ full agonists such as edema and adipogenesis. Ongoing clinical development is directed at translating these findings into establishing a novel and effective treatment for T2DM patients with an improved safety profile in relation to that currently available.