Approach to a Safer Insulin Sensitizer
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Insulin Aspart Sanofi, If It Is Coloured Or It Has Solid Pieces in It
ANNEX I SUMMARY OF PRODUCT CHARACTERISTICS 1 This medicinal product is subject to additional monitoring. This will allow quick identification of new safety information. Healthcare professionals are asked to report any suspected adverse reactions. See section 4.8 for how to report adverse reactions. 1. NAME OF THE MEDICINAL PRODUCT Insulin aspart Sanofi 100 units/ml solution for injection in vial Insulin aspart Sanofi 100 units/ml solution for injection in cartridge Insulin aspart Sanofi 100 units/ml solution for injection in pre-filled pen 2. QUALITATIVE AND QUANTITATIVE COMPOSITION One ml solution contains 100 units insulin aspart* (equivalent to 3.5 mg). Insulin aspart Sanofi 100 units/ml solution for injection in vial Each vial contains 10 ml equivalent to 1,000 units insulin aspart. Insulin aspart Sanofi 100 units/ml solution for injection in cartridge Each cartridge contains 3 ml equivalent to 300 units insulin aspart. Insulin aspart Sanofi 100 units/ml solution for injection in pre-filled pen Each pre-filled pen contains 3 ml equivalent to 300 units insulin aspart. Each pre-filled pen delivers 1-80 units in steps of 1 unit. *produced in Escherichia coli by recombinant DNA technology. For the full list of excipients, see section 6.1. 3. PHARMACEUTICAL FORM Solution for injection (injection). Clear, colourless, aqueous solution. 4. CLINICAL PARTICULARS 4.1 Therapeutic indications Insulin aspart Sanofi is indicated for the treatment of diabetes mellitus in adults, adolescents and children aged 1 year and above. 4.2 Posology and method of administration Posology The potency of insulin analogues, including insulin aspart, is expressed in units, whereas the potency of human insulin is expressed in international units. -

Type 2 Diabetes Mellitus: a Review of Multi-Target Drugs
Molecules 2020, 25, 1987 1 of 20 Review Type 2 Diabetes Mellitus: A Review of Multi-Target Drugs Angelica Artasensi, Alessandro Pedretti, Giulio Vistoli and Laura Fumagalli * Dipartimento di Scienze Farmaceutiche, University Degli Studi di Milano, 20133 Milano, Italy; [email protected] (A.A.); [email protected] (A.P.); [email protected] (G.V.) * Correspondence: [email protected]; Tel.: +39-02-5031-9303 Academic Editor: Massimo Bertinaria, Derek J. McPhee Received: 01 April 2020; Accepted: 21 April 2020; Published: 23 April 2020 Abstract: Diabetes Mellitus (DM) is a multi-factorial chronic health condition that affects a large part of population and according to the World Health Organization (WHO) the number of adults living with diabetes is expected to increase. Since type 2 diabetes mellitus (T2DM) is suffered by the majority of diabetic patients (around 90–95%) and often the mono-target therapy fails in managing blood glucose levels and the other comorbidities, this review focuses on the potential drugs acting on multi-targets involved in the treatment of this type of diabetes. In particular, the review considers the main systems directly involved in T2DM or involved in diabetes comorbidities. Agonists acting on incretin, glucagon systems, as well as on peroxisome proliferation activated receptors are considered. Inhibitors which target either aldose reductase and tyrosine phosphatase 1B or sodium glucose transporters 1 and 2 are taken into account. Moreover, with a view at the multi-target approaches for T2DM some phytocomplexes are also discussed. Keywords: diabetes mellitus; type 2 diabetes mellitus; multi-target compounds; multi-target drugs 1. -

Dualism of Peroxisome Proliferator-Activated Receptor Α/Γ: a Potent Clincher in Insulin Resistance
AEGAEUM JOURNAL ISSN NO: 0776-3808 Dualism of Peroxisome Proliferator-Activated Receptor α/γ: A Potent Clincher in Insulin Resistance Mr. Ravikumar R. Thakar1 and Dr. Nilesh J. Patel1* 1Faculty of Pharmacy, Shree S. K. Patel College of Pharmaceutical Education & Research, Ganpat University, Gujarat, India. [email protected] Abstract: Diabetes mellitus is clinical syndrome which is signalised by augmenting level of sugar in blood stream, which produced through lacking of insulin level and defective insulin activity or both. As per worldwide epidemiology data suggested that the numbers of people with T2DM living in developing countries is increasing with 80% of people with T2DM. Peroxisome proliferator-activated receptors are a family of ligand-activated transcription factors; modulate the expression of many genes. PPARs have three isoforms namely PPARα, PPARβ/δ and PPARγ that play a central role in regulating glucose, lipid and cholesterol metabolism where imbalance can lead to obesity, T2DM and CV ailments. It have pathogenic role in diabetes. PPARα is regulates the metabolism of lipids, carbohydrates, and amino acids, activated by ligands such as polyunsaturated fatty acids, and drugs used as Lipid lowering agents. PPAR β/δ could envision as a therapeutic option for the correction of diabetes and a variety of inflammatory conditions. PPARγ is well categorized, an element of the PPARs, also pharmacological effective as an insulin resistance lowering agents, are used as a remedy for insulin resistance integrated with type- 2 diabetes mellitus. There are mechanistic role of PPARα, PPARβ/δ and PPARγ in diabetes mellitus and insulin resistance. From mechanistic way, it revealed that dual PPAR-α/γ agonist play important role in regulating both lipids as well as glycemic levels with essential safety issues. -

Comparative Transcriptional Network Modeling of Three PPAR-A/C Co-Agonists Reveals Distinct Metabolic Gene Signatures in Primary Human Hepatocytes
Comparative Transcriptional Network Modeling of Three PPAR-a/c Co-Agonists Reveals Distinct Metabolic Gene Signatures in Primary Human Hepatocytes Rene´e Deehan1, Pia Maerz-Weiss2, Natalie L. Catlett1, Guido Steiner2, Ben Wong1, Matthew B. Wright2*, Gil Blander1¤a, Keith O. Elliston1¤b, William Ladd1, Maria Bobadilla2, Jacques Mizrahi2, Carolina Haefliger2, Alan Edgar{2 1 Selventa, Cambridge, Massachusetts, United States of America, 2 F. Hoffmann-La Roche AG, Basel, Switzerland Abstract Aims: To compare the molecular and biologic signatures of a balanced dual peroxisome proliferator-activated receptor (PPAR)-a/c agonist, aleglitazar, with tesaglitazar (a dual PPAR-a/c agonist) or a combination of pioglitazone (Pio; PPAR-c agonist) and fenofibrate (Feno; PPAR-a agonist) in human hepatocytes. Methods and Results: Gene expression microarray profiles were obtained from primary human hepatocytes treated with EC50-aligned low, medium and high concentrations of the three treatments. A systems biology approach, Causal Network Modeling, was used to model the data to infer upstream molecular mechanisms that may explain the observed changes in gene expression. Aleglitazar, tesaglitazar and Pio/Feno each induced unique transcriptional signatures, despite comparable core PPAR signaling. Although all treatments inferred qualitatively similar PPAR-a signaling, aleglitazar was inferred to have greater effects on high- and low-density lipoprotein cholesterol levels than tesaglitazar and Pio/Feno, due to a greater number of gene expression changes in pathways related to high-density and low-density lipoprotein metabolism. Distinct transcriptional and biologic signatures were also inferred for stress responses, which appeared to be less affected by aleglitazar than the comparators. In particular, Pio/Feno was inferred to increase NFE2L2 activity, a key component of the stress response pathway, while aleglitazar had no significant effect. -

CDR Clinical Review Report for Soliqua
CADTH COMMON DRUG REVIEW Clinical Review Report Insulin glargine and lixisenatide injection (Soliqua) (Sanofi-Aventis) Indication: adjunct to diet and exercise to improve glycemic control in adults with type 2 diabetes mellitus inadequately controlled on basal insulin (less than 60 units daily) alone or in combination with metformin. Service Line: CADTH Common Drug Review Version: Final (with redactions) Publication Date: January 2019 Report Length: 118 Pages Disclaimer: The information in this document is intended to help Canadian health care decision-makers, health care professionals, health systems leaders, and policy-makers make well-informed decisions and thereby improve the quality of health care services. While patients and others may access this document, the document is made available for informational purposes only and no representations or warranties are made with respect to its fitness for any particular purpose. The information in this document should not be used as a substitute for professional medical advice or as a substitute for the application of clinical judgment in respect of the care of a particular patient or other professional judgment in any decision-making process. The Canadian Agency for Drugs and Technologies in Health (CADTH) does not endorse any information, drugs, therapies, treatments, products, processes, or services. While care has been taken to ensure that the information prepared by CADTH in this document is accurate, complete, and up-to-date as at the applicable date the material was first published by CADTH, CADTH does not make any guarantees to that effect. CADTH does not guarantee and is not responsible for the quality, currency, propriety, accuracy, or reasonableness of any statements, information, or conclusions contained in any third-party materials used in preparing this document. -

Lobeglitazone
2013 International Conference on Diabetes and Metabolism Lobeglitazone, A Novel PPAR-γ agonist with balanced efficacy and safety Kim, Sin Gon. MD, PhD. Professor, Division of Endocrinology and Metabolism Department of Internal Medicine, Korea University College of Medicine. Disclosure of Financial Relationships This symposium is sponsored by Chong Kun Dang Pharmaceutical Corp. I have received lecture and consultation fees from Chong Kun Dang. Pros & Cons of PPAR-γ agonist Pros Cons • Good glucose lowering • Adverse effects • Durability (ADOPT) (edema, weight gain, • Insulin sensitizing CHF, fracture or rare effects (especially in MS, macular edema etc) NAFLD, PCOS etc) • Possible safety issues • Prevention of new- (risk of MI? – Rosi or onset diabetes (DREAM, bladder cancer? - Pio) ACT-NOW) • LessSo, hypoglycemiathere is a need to develop PPAR-γ • Few GI troubles agonist• Outcome with data balanced efficacy and safety (PROactive) Insulin Sensitizers : Several Issues Rosi, Peak sale ($3.3 billion) DREAM Dr. Nissen Dr. Nissen ADOPT META analysis BARI-2D (5,8) Rosi, lipid profiles RECORD 1994 1997 1999 2000 2002 2004 2005 2006 2007 2008 2009 2010 2011 2012 2013 2014 Tro out d/t FDA, All diabetes hepatotoxicity drug CV safety Rosi (5) FDA, Black box Rosi, Rosi , CV safety warning - REMS in USA = no evidence - Europe out Pio (7) PIO, bladder cancer CKD 501 Lobeglitazone 2000.6-2004.6 2004.11-2007.1 2007.3-2008.10 2009.11-2011.04 Discovery& Preclinical study Phase I Phase II Phase III Developmental Strategy Efficacy • PPAR activity Discovery & Preclinical study • In vitro & vivo efficacy • Potent efficacy 2000.06 - 2004.06 Phase I 2004.11 - 2007.01 • In vitro screening • Repeated dose toxicity • Metabolites • Geno toxicity • Phase II CYP 450 • Reproductive toxicity 2007.03 - 2008.10 • DDI • Carcinogenic toxicity ADME Phase III Safety 2009.11 - 2011.04 CV Safety / (Bladder) Cancer / Liver Toxicity / Bone loss Lobeglitazone (Duvie) 1. -

Title: Combination of Pparg Agonist Pioglitazone and Trabectedin Induce Adipocyte Differentiation to Overcome Trabectedin Resistance in Myxoid Liposarcomas
Author Manuscript Published OnlineFirst on September 3, 2019; DOI: 10.1158/1078-0432.CCR-19-0976 Author manuscripts have been peer reviewed and accepted for publication but have not yet been edited. Title: Combination of PPARg agonist pioglitazone and trabectedin induce adipocyte differentiation to overcome trabectedin resistance in myxoid liposarcomas Roberta Frapolli1, Ezia Bello1, Marianna Ponzo1, Ilaria Craparotta2, Laura Mannarino2, Sara Ballabio2, Sergio Marchini2, Laura Carrassa3, Paolo Ubezio4, Luca Porcu5, Silvia Brich6, Roberta Sanfilippo7, Paolo Giovanni Casali7, Alessandro Gronchi8, Silvana Pilotti6, and Maurizio D’Incalci9*. 1 Unit of Preclinical Experimental Therapeutics, Department of Oncology, Istituto di Ricerche Farmacologiche Mario Negri IRCCS, 20156 Milan, Italy. 2 Unit of Translational Genomic, Department of Oncology, Istituto di Ricerche Farmacologiche Mario Negri IRCCS, 20156 Milan, Italy. 3Unit of DNA repair, Department of Oncology, Istituto di Ricerche Farmacologiche Mario Negri IRCCS, 20156 Milan, Italy. 4 Unit of Biophysics, Department of Oncology, Istituto di Ricerche Farmacologiche Mario Negri IRCCS, 20156 Milan, Italy. 5 Unit of Methodological Research, Department of Oncology, Istituto di Ricerche Farmacologiche Mario Negri IRCCS, 20156 Milan, Italy. 6Laboratory of Molecular Pathology, Department of Pathology, Fondazione IRCCS Istituto Nazionale dei Tumori, 20133 Milan, Italy. 7 Medical Oncology Unit 2, Fondazione IRCCS Istituto Nazionale dei Tumori, 20133 Milan, Italy. 8 Department of Surgery, Fondazione IRCCS Istituto Nazionale dei Tumori, 20133 Milan, Italy. 9 Department of Oncology, Istituto di Ricerche Farmacologiche Mario Negri IRCCS, 20156 Milan, Italy. Running title: Pioglitazone - trabectedin in myxoid liposarcomas. Keywords: Myxoid liposarcoma, trabectedin resistance, PPAR agonist, and patient-derived xenograft. Additional information: Financial support: This work was supported by the Italian Association for Cancer Research grant to M.D. -
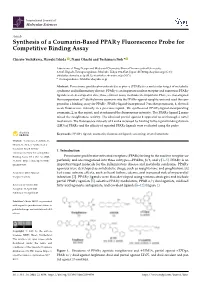
Synthesis of a Coumarin-Based PPAR Fluorescence Probe for Competitive Binding Assay
International Journal of Molecular Sciences Article Synthesis of a Coumarin-Based PPARγ Fluorescence Probe for Competitive Binding Assay Chisato Yoshikawa, Hiroaki Ishida , Nami Ohashi and Toshimasa Itoh * Laboratory of Drug Design and Medicinal Chemistry, Showa Pharmaceutical University, 3-3165 Higashi-Tamagawagakuen, Machida, Tokyo 194-8543, Japan; [email protected] (C.Y.); [email protected] (H.I.); [email protected] (N.O.) * Correspondence: [email protected] Abstract: Peroxisome proliferator-activated receptor γ (PPARγ) is a molecular target of metabolic syndrome and inflammatory disease. PPARγ is an important nuclear receptor and numerous PPARγ ligands were developed to date; thus, efficient assay methods are important. Here, we investigated the incorporation of 7-diethylamino coumarin into the PPARγ agonist rosiglitazone and used the com- pound in a binding assay for PPARγ. PPARγ-ligand-incorporated 7-methoxycoumarin, 1, showed weak fluorescence intensity in a previous report. We synthesized PPARγ-ligand-incorporating coumarin, 2, in this report, and it enhanced the fluorescence intensity. The PPARγ ligand 2 main- tained the rosiglitazone activity. The obtained partial agonist 6 appeared to act through a novel mechanism. The fluorescence intensity of 2 and 6 increased by binding to the ligand binding domain (LBD) of PPARγ and the affinity of reported PPARγ ligands were evaluated using the probe. Keywords: PPARγ ligand; coumarin; fluorescent ligand; screening; crystal structure Citation: Yoshikawa, C.; Ishida, H.; Ohashi, N.; Itoh, T. Synthesis of a Coumarin-Based PPARγ 1. Introduction Fluorescence Probe for Competitive Binding Assay. Int. J. Mol. Sci. 2021, Peroxisome proliferator-activated receptors (PPARs) belong to the nuclear receptor su- 22, 4034. -

OSENI Safely and Effectively
HIGHLIGHTS OF PRESCRIBING INFORMATION -----------------------WARNINGS AND PRECAUTIONS---------------------- These highlights do not include all the information needed to use Congestive heart failure: Fluid retention may occur and can OSENI safely and effectively. See full prescribing information for exacerbate or lead to congestive heart failure. Combination use OSENI. with insulin and use in congestive heart failure NYHA Class I and OSENI (alogliptin and pioglitazone) tablets II may increase risk. Monitor patients for signs and symptoms. Initial U.S. Approval: 2013 (5.1) Acute pancreatitis: There have been postmarketing reports of WARNING: CONGESTIVE HEART FAILURE acute pancreatitis. If pancreatitis is suspected, promptly See full prescribing information for complete boxed warning discontinue OSENI. (5.2) Thiazolidinediones, including pioglitazone, cause or Hypersensitivity: There have been postmarketing reports of exacerbate congestive heart failure in some patients. (5.1) serious hypersensitivity reactions in patients treated with alogliptin After initiation of OSENI and after dose increases, monitor such as anaphylaxis, angioedema and severe cutaneous adverse patients carefully for signs and symptoms of heart failure reactions. In such cases, promptly discontinue OSENI, assess for (e.g., excessive, rapid weight gain, dyspnea, and/or other potential causes, institute appropriate monitoring and edema). If heart failure develops, it should be managed treatment, and initiate alternative treatment for diabetes. (5.3) according to current standards of care and Hepatic effects: Postmarketing reports of hepatic failure, discontinuation or dose reduction of pioglitazone in OSENI sometimes fatal. Causality cannot be excluded. If liver injury is must be considered. detected, promptly interrupt OSENI and assess patient for OSENI is not recommended in patients with symptomatic probable cause, then treat cause if possible, to resolution or heart failure. -

The Opportunities and Challenges of Peroxisome Proliferator-Activated Receptors Ligands in Clinical Drug Discovery and Development
International Journal of Molecular Sciences Review The Opportunities and Challenges of Peroxisome Proliferator-Activated Receptors Ligands in Clinical Drug Discovery and Development Fan Hong 1,2, Pengfei Xu 1,*,† and Yonggong Zhai 1,2,* 1 Beijing Key Laboratory of Gene Resource and Molecular Development, College of Life Sciences, Beijing Normal University, Beijing 100875, China; [email protected] 2 Key Laboratory for Cell Proliferation and Regulation Biology of State Education Ministry, College of Life Sciences, Beijing Normal University, Beijing 100875, China * Correspondence: [email protected] (P.X.); [email protected] (Y.Z.); Tel.: +86-156-005-60991 (P.X.); +86-10-5880-6656 (Y.Z.) † Current address: Center for Pharmacogenetics and Department of Pharmaceutical Sciences, University of Pittsburgh, Pittsburgh, PA 15213, USA. Received: 22 June 2018; Accepted: 24 July 2018; Published: 27 July 2018 Abstract: Peroxisome proliferator-activated receptors (PPARs) are a well-known pharmacological target for the treatment of multiple diseases, including diabetes mellitus, dyslipidemia, cardiovascular diseases and even primary biliary cholangitis, gout, cancer, Alzheimer’s disease and ulcerative colitis. The three PPAR isoforms (α, β/δ and γ) have emerged as integrators of glucose and lipid metabolic signaling networks. Typically, PPARα is activated by fibrates, which are commonly used therapeutic agents in the treatment of dyslipidemia. The pharmacological activators of PPARγ include thiazolidinediones (TZDs), which are insulin sensitizers used in the treatment of type 2 diabetes mellitus (T2DM), despite some drawbacks. In this review, we summarize 84 types of PPAR synthetic ligands introduced to date for the treatment of metabolic and other diseases and provide a comprehensive analysis of the current applications and problems of these ligands in clinical drug discovery and development. -

Muraglitazar Bristol-Myers Squibb/Merck Daniella Barlocco
Muraglitazar Bristol-Myers Squibb/Merck Daniella Barlocco Address Originator Bristol-Myers Squibb Co University of Milan . Istituto di Chimica Farmaceutica e Tossicologica Viale Abruzzi 42 Licensee Merck & Co Inc 20131 Milano . Italy Status Pre-registration Email: [email protected] . Indications Metabolic disorder, Non-insulin-dependent Current Opinion in Investigational Drugs 2005 6(4): diabetes © The Thomson Corporation ISSN 1472-4472 . Actions Antihyperlipidemic agent, Hypoglycemic agent, Bristol-Myers Squibb and Merck & Co are co-developing Insulin sensitizer, PPARα agonist, PPARγ agonist muraglitazar, a dual peroxisome proliferator-activated receptor-α/γ . agonist, for the potential treatment of type 2 diabetes and other Synonym BMS-298585 metabolic disorders. In November 2004, approval was anticipated as early as mid-2005. Registry No: 331741-94-7 Introduction [579218], [579221], [579457], [579459]. PPARγ is expressed in Type 2 diabetes is a complex metabolic disorder that is adipose tissue, lower intestine and cells involved in characterized by hyperglycemia, insulin resistance and immunity. Activation of PPARγ regulates glucose and lipid defects in insulin secretion. The disease is associated with homeostasis, and triggers insulin sensitization [579216], older age, obesity, a family history of diabetes and physical [579218], [579458], [579461]. PPARδ is expressed inactivity. The prevalence of type 2 diabetes is increasing ubiquitously and has been found to be effective in rapidly, and the World Health Organization warns that, controlling dyslipidemia and cardiovascular diseases unless appropriate action is taken, the number of sufferers [579216]. PPARα agonists are used as potent hypolipidemic will double to over 350 million individuals by the year compounds, increasing plasma high-density lipoprotein 2030. Worryingly, it is estimated that only half of sufferers (HDL)-cholesterol and reducing free fatty acids, are diagnosed with the condition [www.who.int]. -

Regulation of Enac-Mediated Sodium Reabsorption by Peroxisome Proliferator-Activated Receptors
Hindawi Publishing Corporation PPAR Research Volume 2010, Article ID 703735, 9 pages doi:10.1155/2010/703735 Review Article Regulation of ENaC-Mediated Sodium Reabsorption by Peroxisome Proliferator-Activated Receptors Tengis S. Pavlov,1 John D. Imig,2, 3 and Alexander Staruschenko1, 4 1 Department of Physiology, Medical College of Wisconsin, Milwaukee, WI 53226, USA 2 Department of Pharmacology and Toxicology, Medical College of Wisconsin, Milwaukee, WI 53226, USA 3 Cardiovascular Research Center, Medical College of Wisconsin, Milwaukee, WI 53226, USA 4 Kidney Disease Center, Medical College of Wisconsin, Milwaukee, WI 53226, USA Correspondence should be addressed to Alexander Staruschenko, [email protected] Received 6 January 2010; Revised 16 March 2010; Accepted 14 April 2010 Academic Editor: Tianxin Yang Copyright © 2010 Tengis S. Pavlov et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. Peroxisome proliferator-activated receptors (PPARs) are members of a steroid hormone receptor superfamily that responds to changes in lipid and glucose homeostasis. Peroxisomal proliferator-activated receptor subtype γ (PPARγ)hasreceivedmuch attention as the target for antidiabetic drugs, as well as its role in responding to endogenous compounds such as prostaglandin J2. However, thiazolidinediones (TZDs), the synthetic agonists of the PPARγ are tightly associated with fluid retention and edema, as potentially serious side effects. The epithelial sodium channel (ENaC) represents the rate limiting step for sodium absorption in the renal collecting duct. Consequently, ENaC is a central effector impacting systemic blood volume and pressure. The role of PPARγ agonists on ENaC activity remains controversial.