Nicotinamide Activates Latent HIV-1 Ex Vivo in ART Suppressed
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Steroid Recognition and Regulation of Hormone Action: Crystal
Research Article 799 Steroid recognition and regulation of hormone action: crystal structure of testosterone and NADP+ bound to 3a-hydroxysteroid/ dihydrodiol dehydrogenase Melanie J Bennett1†, Ross H Albert1, Joseph M Jez1, Haiching Ma2, Trevor M Penning2 and Mitchell Lewis1* Background: Mammalian 3a-hydroxysteroid dehydrogenases (3a-HSDs) Addresses: 1Department of Biochemistry and modulate the activities of steroid hormones by reversibly reducing their C3 Biophysics, The Johnson Research Foundation, 37th and Hamilton Walk, Philadelphia, PA 19104- ketone groups. In steroid target tissues, 3a-HSDs act on 5a-dihydrotestosterone, 6059, USA and 2Department of Pharmacology, a potent male sex hormone (androgen) implicated in benign prostate hyperplasia University of Pennsylvania School of Medicine, 37th and prostate cancer. Rat liver 3a-HSD belongs to the aldo-keto reductase (AKR) and Hamilton Walk, Philadelphia, PA 19104-6084, superfamily and provides a model for mammalian 3a-, 17b- and 20a-HSDs, USA. which share > 65% sequence identity. The determination of the structure of 3a- †Present address: Division of Biology, California + HSD in complex with NADP and testosterone (a competitive inhibitor) will help Institute of Technology, 1200 E California Blvd., to further our understanding of steroid recognition and hormone regulation by Pasadena, CA 91125, USA. mammalian HSDs. *Corresponding author. E-mail: [email protected] Results: We have determined the 2.5 Å resolution crystal structure of recombinant rat liver 3a-HSD complexed with NADP+ and testosterone. The Key words: aldo-keto reductase, crystal structure, structure provides the first picture of an HSD ternary complex in the AKR 3a-hydroxysteroid/dihydrodiol dehydrogenase, superfamily, and is the only structure to date of testosterone bound to a protein. -

Apigenin-Loaded Solid Lipid Nanoparticle Attenuates Diabetic Nephropathy Induced by Streptozotocin Nicotinamide Through Nrf2/ HO-1/NF-Kb Signalling Pathway
International Journal of Nanomedicine Dovepress open access to scientific and medical research Open Access Full Text Article ORIGINAL RESEARCH Apigenin-Loaded Solid Lipid Nanoparticle Attenuates Diabetic Nephropathy Induced by Streptozotocin Nicotinamide Through Nrf2/ HO-1/NF-kB Signalling Pathway This article was published in the following Dove Press journal: International Journal of Nanomedicine Pingping Li1 Background: Apigenin is known to have a broad-spectrum efficacy in oxidative stress and Syed Nasir Abbas Bukhari 2 conditions due to inflammation, although weak absorption, fast metabolic rate and a fast Tahseen Khan 3 elimination (systemic) limit the pharmacological efficacy of this drug. Hence, we propose the Renukaradhya Chitti4 usage of highly bioavailable Apigenin-solid lipid nanoparticles (SLNPs) to recognize such Davan B Bevoor5 limitations. The defensive function of Apigenin-SLNPs on renal damage induced by strep 6 tozotocin (STZ) in animals was studied. Anand R Hiremath −1 7 Materials and Methods: We initially injected the rats with 35 mg kg streptozocin intraper Nagaraja SreeHarsha −1 8 itoneally, and after 7 days, the rats were then injected 150 mg kg of metformin intragastrically Yogendra Singh followed by a once-daily intragastric dose of Apigenin-SLNP (25 or 50 mg kg−1) for 9 Kumar Shiva Gubbiyappa a continuous period of 30 days. We then measured the level of insulin and blood glucose, 1Department of Nephrology, Zhengzhou superoxide dismutase, catalase and malondialdehyde in the tissues of the kidney. We also Central Hospital Affiliated to Zhengzhou observed messenger-RNA expression of Interleukin-1β, Interleukin-6 and Tumor Necrosis University, Zhengzhou City, Henan Province 450007, People’s Republic of Factor-alpha in renal tissue through RT-PCR technique. -

Men's Health& Testosterone
Q&A: NEW ENDOCRINE REVIEWS EIC DANIEL J. DRUCKER, MD JUNE 2018 THE LEADING MAGAZINE FOR ENDOCRINOLOGISTS Men’s Health & Testosterone ● New Endocrine Society guidelines detail why hypogonadism patients should be treated when consistently low T levels are tied to symptoms, not what the patient saw on television. ● A closer look at the T Trials shows that testosterone therapy may actually be suitable for older patients with hypogonadism. ONCE A DAY: ENS New research may finally achieve the “male pill” M ’ WHY ENDOCRINOLOGY?: A newcomer’s perspective from the bench HEALTH & TESTOSTERONE TEST YOUR KNOWLEDGE WITH PEDIATRIC ESAPTM THE LEADING MAGAZINE FOR ENDOCRINOLOGISTS 2017-2018 2017 – 2019 EDITORIAL ADVISORY BOARD Henry Anhalt, DO Bergen County Pediatric Endocrinology Chair, Hormone Health Network VP, Medical Affairs, Science 37 Sally Camper, PhD Department of Human Genetics University of Michigan Medical School Rodolfo J. Galindo, MD Assistant Professor of Medicine Mount Sinai School of Medicine Christian M. Girgis, MBBS, PhD, FRACP Royal North Shore and Westmead Hospitals University of Sydney, Australia Andrea Gore, PhD Division of Pharmacology and Toxicology University of Texas Daniel A. Gorelick, PhD Solve 100 New Cases In Department of Pharmacology & Toxicology University of Alabama at Birmingham One Module, Now Delivering: M. Carol Greenlee, MD, FACP Interactive online modules Western Slope Endocrinology Grand Junction, Colo. and printed reference book (Faculty for Transforming Clinical Practice initiative [TCPi]) Peer-review comparisons Gary D. Hammer, MD, PhD for each question Millie Schembechler Professor of Adrenal Cancer, Endocrine Oncology Program Detailed overall University of Michigan performance report Robert W. Lash, MD Chief Professional & Clinical Officer, Endocrine Society Lab values in conventional and SI Units Karl Nadolsky, DO Diabetes Obesity & Metabolic Institute 40 ABP MOC Part 2 points and Walter Reed National Military Medical Center; Uniformed Services University 40.0 AMA PRA Category 1 Credits™ Joshua D. -

Flavonoid Apigenin Is an Inhibitor of the NAD+Ase CD38: Implications for Cellular NAD+ Metabolism, Protein Acetylation, and Treatment of Metabolic Syndrome
Flavonoid Apigenin Is an Inhibitor of the NAD+ase CD38: Implications for Cellular NAD+ Metabolism, Protein Acetylation, and Treatment of Metabolic Syndrome The Harvard community has made this article openly available. Please share how this access benefits you. Your story matters Citation Escande, Carlos, Veronica Nin, Nathan L. Price, Verena Capellini, Ana P. Gomes, Maria Thereza Barbosa, Luke O’Neil, Thomas A. White, David A. Sinclair, and Eduardo N. Chini. 2013. “Flavonoid Apigenin Is an Inhibitor of the NAD+ase CD38: Implications for Cellular NAD+ Metabolism, Protein Acetylation, and Treatment of Metabolic Syndrome.” Diabetes 62 (4): 1084-1093. doi:10.2337/ db12-1139. http://dx.doi.org/10.2337/db12-1139. Published Version doi:10.2337/db12-1139 Citable link http://nrs.harvard.edu/urn-3:HUL.InstRepos:12152908 Terms of Use This article was downloaded from Harvard University’s DASH repository, and is made available under the terms and conditions applicable to Other Posted Material, as set forth at http:// nrs.harvard.edu/urn-3:HUL.InstRepos:dash.current.terms-of- use#LAA ORIGINAL ARTICLE Flavonoid Apigenin Is an Inhibitor of the NAD+ase CD38 Implications for Cellular NAD+ Metabolism, Protein Acetylation, and Treatment of Metabolic Syndrome Carlos Escande,1 Veronica Nin,1 Nathan L. Price,2 Verena Capellini,1 Ana P. Gomes,2 Maria Thereza Barbosa,1 Luke O’Neil,1 Thomas A. White,1 David A. Sinclair,2 and Eduardo N. Chini1 Metabolic syndrome is a growing health problem worldwide. It is syndrome (5). This concept was later expanded by others therefore imperative to develop new strategies to treat this using different approaches, including inhibition of poly-ADP- + pathology. -

Zambia Essential Medicine List (Zeml) 03 2013
ZAMBIA ESSENTIAL MEDICINE LIST (ZEML) 03 2013 Drug Presentation Level VEN 1 Drugs used in anaesthesia 1.1. Drugs used in general anaesthesia 1.1.1 Intravenous and intramuscular anaesthetics 1.1.1.1 Ketamin injection 10mg/ml (10 ml) II-IV V 1.1.1.2 Thiopentone sodium powder for reconstitution 1g and 5g vials II-IV V 1.1.2 Inhalation anaesthetics 1.1.2.1 Halothane inhalation II-IV V 1.1.2.2 Nitrous oxide medical gas II-IV E 1.1.3 Muscle relaxants 1.1.3.1 Suxamethonium chloride injection 50mg/ml, (2ml) II-IV V 1.1.4 Anticholinesterases 1.1.4.1 Neostigmine injection 2.5mg/ml, (1ml) II-IV V 1.2 Drugs used in local anaesthesia 1.2.1. Lignocaine injection 1% (10ml, 50ml) I-IV V 1.2.2 Lignocaine + adrenaline dental cartridge injection 2% (1 in 80,000) II-IV V 1.3 Drugs used in spinal anaesthesia 1.3.1 Bupivacaine/glucose injection 0.5%, (4ml) IV E 1 Drug Presentation Level VEN 2. Drugs acting on the gastrointestinal system 2.1 Antacids 2.1.1 Aluminium hydroxide gel, chewable tablets I-IV E 2.12 Magnesium trisilicate Compound chewable tablets, mixture I-IV E 2.2. Antispasmodics 2.2.1 Hyoscine butyl bromide injection 20mg/ml, (1ml) II-IV E 2.2.2 Propantheline bromide tablets 15mg I-IV E 2.3 Ulcer healing drugs 2.3.1 Cimetidine tablets 200mg II-IV E 2.3.2 Omeprazole tablets 10mg, II-IV E 2.3.3 Ranitidine tablets 150mg II-IV E 2.3.4 Tripotassium dicitratobismuthate tablets 120mg II-IV E 2.3.5 Clarithromycin tablets 250mg II-IV E 2.4. -

World Health Organization Model List of Essential Medicines, 21St List, 2019
World Health Organizatio n Model List of Essential Medicines 21st List 2019 World Health Organizatio n Model List of Essential Medicines 21st List 2019 WHO/MVP/EMP/IAU/2019.06 © World Health Organization 2019 Some rights reserved. This work is available under the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 IGO licence (CC BY-NC-SA 3.0 IGO; https://creativecommons.org/licenses/by-nc-sa/3.0/igo). Under the terms of this licence, you may copy, redistribute and adapt the work for non-commercial purposes, provided the work is appropriately cited, as indicated below. In any use of this work, there should be no suggestion that WHO endorses any specific organization, products or services. The use of the WHO logo is not permitted. If you adapt the work, then you must license your work under the same or equivalent Creative Commons licence. If you create a translation of this work, you should add the following disclaimer along with the suggested citation: “This translation was not created by the World Health Organization (WHO). WHO is not responsible for the content or accuracy of this translation. The original English edition shall be the binding and authentic edition”. Any mediation relating to disputes arising under the licence shall be conducted in accordance with the mediation rules of the World Intellectual Property Organization. Suggested citation. World Health Organization Model List of Essential Medicines, 21st List, 2019. Geneva: World Health Organization; 2019. Licence: CC BY-NC-SA 3.0 IGO. Cataloguing-in-Publication (CIP) data. CIP data are available at http://apps.who.int/iris. -

Section 2.6.4 Pharmacokinetics Written Summary EMTRICITABINE
SECTION 2.6 NONCLINICAL SUMMARY Section 2.6.4 Pharmacokinetics Written Summary EMTRICITABINE/ RILPIVIRINE/ TENOFOVIR DISOPROXIL FUMARATE FIXED-DOSE COMBINATION 17 August 2010 CONFIDENTIAL AND PROPRIETARY INFORMATION Emtricitabine/Rilpivirine/Tenofovir Disoproxil Fumarate Section 2.6.4 Pharmacokinetics Written Summary Final TABLE OF CONTENTS SECTION 2.6 NONCLINICAL SUMMARY........................................................................................................1 TABLE OF CONTENTS .......................................................................................................................................2 GLOSSARY OF ABBREVIATIONS AND DEFINITION OF TERMS ..............................................................5 2.6. NONCLINICAL SUMMARY.......................................................................................................................8 2.6.4. PHARMACOKINETICS WRITTEN SUMMARY .........................................................................8 2.6.4.1. Brief Summary................................................................................................................8 2.6.4.2. Methods of Analysis .....................................................................................................14 2.6.4.2.1. Emtricitabine............................................................................................14 2.6.4.2.2. Rilpivirine ................................................................................................14 2.6.4.2.3. Tenofovir Disoproxil Fumarate -
IV NAD Website3 Cost
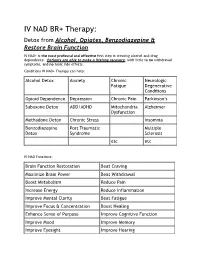
IV NAD BR+ Therapy: Detox from Alcohol, Opiates, Benzodiazepine & Restore Brain Function IV NAD+ is the most profound and effective first step in treating alcohol and drug dependence. Patients are able to make a lifelong recovery, with little to no withdrawal symptoms, and no toxic side effects. Conditions IV NAD+ Therapy can help: Alcohol Detox Anxiety Chronic Neurologic Fatigue Degenerative Conditions Opioid Dependence Depression Chronic Pain Parkinson’s Suboxone Detox ADD/ADHD Mitochondria Alzheimer Dysfunction Methadone Detox Chronic Stress Insomnia Benzodiazepine Post Traumatic Multiple Detox Syndrome Sclerosis etc etc IV NAD Functions: Brain Function Restoration Beat Craving Maximize Brain Power Beat Withdrawal Boost Metabolism Reduce Pain Increase Energy Reduce Inflammation Improve Mental Clarity Beat Fatigue Improve Focus & Concentration Boost Healing Enhance Sense of Purpose Improve Cognitive Function Improve Mood Improve Memory Improve Eyesight Improve Hearing Dr. Hong Davis. MD is only medical doctor in Texas who is Brain Restoration Plus certified (BR+ Certified). BR+ is a certification that only a few Doctors nationwide obtain which teaches the doctors the proper implementation of NAD protocols. By obtaining this certificate, it guarantees maximum results and efficiency. What is IV NAD+ Therapy: Intravenous drip of Nicotinamide Adenine Dinucleotide (NAD+) is a treatment helps the brain quickly be restored to its nature, healthy stats. It is a natural, restorative, and protective therapy to give people a better chance to live a sober and pain free life. It is a nutritionally based treatment for Addictions, Post Traumatic Stress, Chronic Stress/Fatigue, Depression, Anxiety, ADHD, and Neurodegenerative Diseases like multiple sclerosis, Parkinson’s, and Alzheimer’s. -

Enzymatic Baeyer-Villiger Type Oxidations of Ketones Catalyzed By
BrooRGANrccHEMTSTRY 17, 4l-_52(1989) EnzymaticBaeyer-Villiger Type Oxidations of Ketones Catalyzedby CyclohexanoneOxygenase OssroraNR AnnrL, Cenol C. RyEnsoN,CsRrsropHER Wnr-sH. eNo GEoncE,M. WHrrEsrogsl Department of Chemistry, Haruard Uniuersity, Camhridge, Massac'husetts02138, und Department of Chemistry, Massachusetts Institute of Technologt,, Cumbridge, Mussachusett.s02138 Rec'eiuedFehruury 9, 1988;accepted August 31, 1988 Cyclohexanone oxygenase (EC l l4.l3.-) produced by Acinetobat'ter NCIB 9871 is a flavin-containingNADPH-dependent monooxygenasethat utilizes dioxygen to convert cy- clic ketones into lactones. A variety of ketones were examined in order to determine the substratespecificity. regioselectivity,and enantioselectivityof cyclohexanoneoxygenase. Lactones were synthesizedusing immobilized enzymes.The nicotinamidecotactor required by cyclohexanoneoxygenase was regeneratedin .rilrrr.r,ith glucose 6-phosphate and glucose- 6-phosphatedehydrogenase from Laucono.\to('mesenleroitle.s. i9g9Acactemic press. rnc. INTRODUCTION Microorganisms are capable of effecting a wide range of oxidative transforma- tions of organic compounds (1). Among these transformations, the biological equivalentof the Baeyer-Villigerreactionl (2)-the insertionof an oxygen atom into organic ketones with the production of lactones-has been implicated in microbialdegradations of alkanes.steroids. and cyclic ketones(3-15 ). The ob- jective of this work was to explore the utility of one enzyme-cyclohexanone monooxygenase(EC 1.14.13.-)-capableof catalyzingthis tranformationfor utility in organic synthesis. The microorganismsthat are capableof removing side chains from steroids are alsogenerally able to carry out an additionalBaeyer-Villiger oxidation on the C-17 ketones to give lactones. The microbial double Baeyer-Villiger oxidation of pro- gesteroneby Penicillium c'hrysogenum,for example, gives testololactonein 70Va yield (9). The microbiological Baeyer-Villiger reactionsof steroidsare not limited to C-17 side chains and D-rings. -

Bulk Drug Substances Nominated for Use in Compounding Under Section 503B of the Federal Food, Drug, and Cosmetic Act
Updated June 07, 2021 Bulk Drug Substances Nominated for Use in Compounding Under Section 503B of the Federal Food, Drug, and Cosmetic Act Three categories of bulk drug substances: • Category 1: Bulk Drug Substances Under Evaluation • Category 2: Bulk Drug Substances that Raise Significant Safety Risks • Category 3: Bulk Drug Substances Nominated Without Adequate Support Updates to Categories of Substances Nominated for the 503B Bulk Drug Substances List1 • Add the following entry to category 2 due to serious safety concerns of mutagenicity, cytotoxicity, and possible carcinogenicity when quinacrine hydrochloride is used for intrauterine administration for non- surgical female sterilization: 2,3 o Quinacrine Hydrochloride for intrauterine administration • Revision to category 1 for clarity: o Modify the entry for “Quinacrine Hydrochloride” to “Quinacrine Hydrochloride (except for intrauterine administration).” • Revision to category 1 to correct a substance name error: o Correct the error in the substance name “DHEA (dehydroepiandosterone)” to “DHEA (dehydroepiandrosterone).” 1 For the purposes of the substance names in the categories, hydrated forms of the substance are included in the scope of the substance name. 2 Quinacrine HCl was previously reviewed in 2016 as part of FDA’s consideration of this bulk drug substance for inclusion on the 503A Bulks List. As part of this review, the Division of Bone, Reproductive and Urologic Products (DBRUP), now the Division of Urology, Obstetrics and Gynecology (DUOG), evaluated the nomination of quinacrine for intrauterine administration for non-surgical female sterilization and recommended that quinacrine should not be included on the 503A Bulks List for this use. This recommendation was based on the lack of information on efficacy comparable to other available methods of female sterilization and serious safety concerns of mutagenicity, cytotoxicity and possible carcinogenicity in use of quinacrine for this indication and route of administration. -

Hormonal Effects on Blood Vessels
Hypertension Research (2012) 35, 363–369 & 2012 The Japanese Society of Hypertension All rights reserved 0916-9636/12 www.nature.com/hr REVIEW SERIES Hormonal effects on blood vessels Masahiro Akishita1 and Jing Yu2 The incidence of cardiovascular disease (CVD) is lower in younger women than in men of the same age, but it increases after menopause, implicating the atheroprotective action of endogenous estrogen. Although observational studies have suggested the efficacy of estrogen therapy in postmenopausal women, placebo-controlled, randomized trials, such as the Women’s Health Initiative, have not confirmed effects of estrogen therapy on CVD. Conversely, basic, experimental research has progressed and provided mechanistic insight into estrogen’s action on blood vessels. By contrast, the vascular effects of androgens remain poorly understood and have been controversial for a long time. In recent years, an increasing body of evidence has suggested that androgens may exert protective effects against the development of atherosclerosis, at least in elderly men. Epidemiological studies have shown that the incidence of and mortality due to CVD were increased in elderly men with low testosterone levels, although the efficacy of androgen therapy remains unknown. Furthermore, recent experimental studies have demonstrated the direct action of androgens on the vasculature. In this review, we illustrate the effects of sex steroids on the cardiovascular system, focusing on the action of testosterone on the blood vessels. Hypertension Research (2012) 35, 363–369; doi:10.1038/hr.2012.4; published online 2 February 2012 Keywords: cardiovascular disease; endothelium; estrogen; testosterone; vascular smooth muscle INTRODUCTION As the effects of estrogen on the cardiovascular system have been Since the 1940s, it has been recognized that sex steroids have extensively studied and reviewed,11–14 we allocated a small portion of important roles in the cardiovascular system.1,2 Anumberofepide- our research to estrogen, highlighting recent developments. -

Possible Adverse Effects of High-Dose Nicotinamide
biomolecules Article Possible Adverse Effects of High-Dose Nicotinamide: Mechanisms and Safety Assessment Eun Seong Hwang * and Seon Beom Song Department of Life Science, University of Seoul, Dongdaemun-gu, Seoulsiripdae-ro 163, Seoul 02504, Korea; [email protected] * Correspondence: [email protected]; Tel.: +82-2-64-90-2-669 Received: 13 March 2020; Accepted: 21 April 2020; Published: 29 April 2020 Abstract: Nicotinamide (NAM) at doses far above those recommended for vitamins is suggested to be effective against a wide spectrum of diseases and conditions, including neurological dysfunctions, depression and other psychological disorders, and inflammatory diseases. Recent increases in public awareness on possible pro-longevity effects of nicotinamide adenine dinucleotide (NAD+) precursors have caused further growth of NAM consumption not only for clinical treatments, but also as a dietary supplement, raising concerns on the safety of its long-term use. However, possible adverse effects and their mechanisms are poorly understood. High-level NAM administration can exert negative effects through multiple routes. For example, NAM by itself inhibits poly(ADP-ribose) polymerases (PARPs), which protect genome integrity. Elevation of the NAD+ pool alters cellular energy metabolism. Meanwhile, high-level NAM alters cellular methyl metabolism and affects methylation of DNA and proteins, leading to changes in cellular transcriptome and proteome. Also, methyl metabolites of NAM, namely methylnicotinamide, are predicted to play roles in certain diseases and conditions. In this review, a collective literature search was performed to provide a comprehensive list of possible adverse effects of NAM and to provide understanding of their underlying mechanisms and assessment of the raised safety concerns.