President's Message
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Imaging Services Locations
IMAGING SERVICES LOCATIONS Lake Orion 6 7 Rochester Macomb Pontiac 12 TROY 8 West 1 11 Bloomeld 9 109 Sterling Heights 115 17 FARMINGTON ROYAL HILLS 18 13 Warren St. Clair 19 OAK Shores Novi 4 Southeld 14 18 3 Redford 1 Township 15 Livonia GROSSE 16 Detroit POINTE 2 DEARBORN 1 23 Canton WAYNE 20 22 21 25 24 TAYLOR Belleville 26 27 TRENTON28 Most services can 29 be scheduled by 30 calling Beaumont’s Flat Rock Appointment Center at 800-328-8542. Monroe Imaging Services locations 5 1 Beaumont Imaging Center, Canton 8 Beaumont Health & Wellness Center, 2050 N. Haggerty Road Rochester Hills7 Suite 180 1555 E. South Blvd. Canton, MI 48187 Rochester Hills, MI 48307 734-446-9701 Phone 248-267-5600 Phone 734-446-9704 Fax 248-267-5665 Fax 5 2 Beaumont Medical Center, Canton 9 Beaumont Hospital, Troy 7300 N. Canton Center Road 44201 Dequindre Road Canton, MI 48187 Troy, MI 48085 734-454-8001 Phone 248-964-5000 Phone 734-454-8064 Fax 248-964-6477 Fax Beaumont Cancer & Breast Care Center, Beaumont Breast Imaging, Troy7 3 10 2 Farmington Hills 44201 Dequindre Road 27900 Grand River Ave. Troy, MI 48085 Farmington Hills, MI 48336 248-964-5452 Phone PET/CT Scheduling: 248-556-4089 248-964-3691 Fax 947-521-8374 Phone 7 248-473-4822 Fax 11 Beaumont Medical Park, Sterling Heights 44250 Dequindre Road 4 Beaumont Hospital, Farmington Hills Sterling Heights, MI 48314 28050 Grand River Ave. PET scheduling: 248-898-5785 Suite 101 248-964-7030 Phone Farmington Hills, MI 48336 248-964-7071 Fax 947-521-8120 Phone 7 248-473-4995 Fax 12 Beaumont Medical Center, Macomb 15959 Hall Road 5 Beaumont Medical Center, Macomb, MI 48044 West Bloomfield4 586-416-8410 Phone Suite 103: Women’s Breast Care Center 586-416-8411 Fax 248-855-7830 Phone 4 248-855-7850 Fax 13 Beaumont Medical Center, Warren 8545 Common Road Suite 110: Radiology Warren, MI 48093 248-855-7443 Phone 586-393-3050 Phone 248-855-7470 Fax 586-393-3051 Fax Beaumont Medical Center, Lake Orion 7 6 14 Beaumont Medical Center, 1455 S. -

Page 1 of 3 Creating Care Connected Communities 695 Kenmoor Ave SE, Suite B Grand Rapids, Ml 49546 (844) 454-2443 | [email protected] |
Creating Care Connected Communities 695 Kenmoor Ave SE, Suite B Grand Rapids, Ml 49546 (844) 454-2443 | [email protected] | www.gl-hc.org Organization Name City County Alpena Regional Medical Center Alpena Alpena County Ascension Health - Borgess - Lee Memorial Hospital Dowagiac Cass County Ascension Health - Borgess - Pipp Hospital Plainwell Allegan County Ascension Health - Borgess Medical Center Kalamazoo Kalamazoo County Ascension Health - Genesys Regional Medical Center Grand Blanc Genesee County Ascension Health - Providence Hospital Southfield Oakland County Ascension Health - Providence Park Hospital Novi Oakland County Ascension Health - St John Detroit Riverview Hospital Detroit Wayne County Ascension Health - St John Hospital Warren Macomb County Ascension Health - St John River District Hospital East China St. Clair County Ascension Health - St Joseph Health System Tawas City Iosco County Ascension Health - St Mary's of Michigan - Saginaw Saginaw Saginaw County Ascension Health - St Mary's of Michigan - Standish Standish Arenac County Ascension Health - St. John Macomb - Oakland Hospital - Madison Heights Madison Heights Oakland County Ascension Health - St. John Macomb - Oakland Hospital - Warren Campus Warren Macomb County Beaumont Health System - Beaumont Hospital - Farmington Hills (formerly Botsford Hospital) Farmington Hills Oakland County Beaumont Health System - Grosse Pointe Campus Grosse Pointe Lapeer County Beaumont Health System - Beaumont Hospital - Dearborn (formerly Oakwood Hospital - Dearborn) Dearborn Wayne County -

Beaumont Health Financial Assistance Policy Summary Locations for Assistance Thank You for Choosing Beaumont for Your Healthcare Needs
Beaumont Health Financial Assistance Policy Summary Locations for Assistance Thank you for choosing Beaumont for your healthcare needs. Our goal is to provide all patients with high quality health care services regardless of their Beaumont Hospital – Dearborn financial circumstances. Beaumont Health offers financial assistance to Attention: Benefit Advisors uninsured and underinsured patients for emergency and other medically 18101 Oakwood Blvd. necessary in accordance with our Financial Assistance Policy. Dearborn, Michigan 48124 Telephone: (248) 577-9205 Who is Eligible Beaumont Hospital – Farmington Financial assistance is offered to patients who are uninsured or underinsured and Hills who satisfy requirements stated in our Policy. Eligibility for financial assistance is Attention: Benefit Advisors based on multiple factors, including insurance coverage and other sources of 28050 Grand River Farmington Hills, Michigan 48336 payment (such as for personal injury claims), income (the Federal Poverty Telephone: (248) 577-9205 Guidelines are used to determine the amount of financial assistance offered), family size and assets. Beaumont Hospital – Grosse Pointe Attention: Benefit Advisors Financial Assistance Offered 468 Cadieux Road Depending on the patient’s ability to pay, as determined in accordance with our Grosse Pointe, MI 48230 Telephone: (248) 577-9205 Policy, free care or partial financial assistance may be provided. Financial assistance is limited to medical care provided at a Beaumont Health hospital by Beaumont Hospital – Royal -

Beaumont Hospital - Royal Oak Earns Nine U.S
Beaumont Hospital - Royal Oak earns nine U.S. News & World... https://www.oakland.edu/?id=33056&sid=340 Webmail | MySAIL | Moodle Search OUWB Go About Admissions Students Curriculum Faculty Library Technology Giving Beaumont Health OUWB Connects Art and Medicine for Beaumont Hospital - Royal Oak earns nine U.S. News & World Report ‘Best Hospitals’ a Special Community Program national rankings AOA Honor Medical Society Inducts OUWB Students Dr. Jay Hollander Earns National Top-ranked in Michigan for six medical specialties Award for Excellence in Medical Beaumont Hospital - Royal Oak earned national recognition by U.S. News & World Report in nine medical Education specialties in the “Best Hospital” rankings released today. The Royal Oak hospital ranked No. 2 in Michigan and in OUWB Women in Medicine Profiles Metro Detroit in its 21st consecutive year of national recognition by U.S News. Inaugural Appreciation Event Recognizes Strong Community Less than 3 percent of the nearly 5,000 hospitals analyzed for Best Hospitals 2015-16 earned a national ranking in Partnerships even one specialty. This is the 26th year U.S. News & World Report has ranked hospitals. White Coat Ceremony 2015 Remembered Beaumont Hospital - Royal Oak is nationally ranked in the following nine medical specialties for 2015-16: OUWB Congratulates Capstone Competitive Scholarship Award Cardiology & Heart Surgery - #22 Recipients Top-ranked in Michigan Students Showcase their Internship Diabetes & Endocrinology - #17 Research at Orientation Week Top-ranked in Michigan Kidney -

Field Education
FIELD EDUCATION CANADIAN MENTAL HEALTH ASSOCIATION CAO HOME The following agencies are representative of those who have worked with CAPUCHIN SOUP KITCHEN members of the Faculty in field instruction during recent academic years: CARE AND TRANSFORMATION CENTER ABC SOLUTIONS INC. CARE HOUSE MACOMB COUNTY CHILD ADVOCACY CENTER ABR ADULT DAY SERVICES LLC CARE HOUSE OF OAKLAND COUNTY ACCESS CARE MATTERS ADULT WELL-BEING SERVICES CARE OF SOUTHEASTERN MICHIGAN ADVANCED TECHNOLOGY ACADEMY CAREFIRST COMMUNITY HEALTH SERVICES ADVANTAGE HEALTH CENTERS CATHOLIC CHARITIES OF SOUTHEAST MICHIGAN AFFIRMATIONS CATHOLIC SERVICES OF MACOMB ALGONAC COMMUNITY SCHOOLS CATHOLIC FAMILY SERVICES ALL ABOUT BABY MIHP CENTER FOR COMMUNITY ENGAGEMENT IN HEALTH ALTERNATIVES FOR GIRLS CENTER FOR SOCIAL WORK RESEARCH ALZHEIMER'S ASSOCIATION CENTURY LIVING AMERICAN RED CROSS CESAR CHAVEZ ACADEMY ANCHOR BAY SCHOOL DISTRICT CHADSEY CONDON COMMUNITY ORGANIZATION ANGELA HOSPICE CHALDEAN AMERICAN LADIES OF CHARITY ANN ARBOR CENTER FOR INDEPENDENT LIVING CHERRY HEALTH ARAB-AMERICAN AND CHALDEAN COUNCIL CHILDREN'S CENTER AREA AGENCY ON AGING 1C CHILDREN'S HOSPITAL OF MICHIGAN ARTS ACADEMY IN THE WOODS HIGH SCHOOL CHILDREN'S LEUKEMIA FOUNDATION OF MICHIGAN ASSOCIATED MANAGEMENT COMPANY CHIPPEWA VALLEY SCHOOLS AVONDALE SCHOOL DISTRICT SPECIAL EDUCATION CHITTER CHATTER PC BABY COURT CHRIST CHILD HOUSE BEAUMONT HEALTH SYSTEMS CITY CONNECT DETROIT BEGINNING STEP CITY OF GARDEN CITY BEHAVIORAL CENTER OF AMERICA - STONE CREST CTR. CLARKSTON COMMUNITY SCHOOLS BELLE ISLE CONSERVANCY CLARKSTON SPECIALTY HEALTHCARE CENTER BERKLEY SCHOOL DISTRICT COMMON GROUND - THE SANCTUARY BETHANY CHRISTIAN SERVICES COMMUNITY AND HOME SUPPORTS, INC. BETHANY VILLA SENIOR APARTMENTS COMMUNITY CARE SERVICES BIG BROTHERS BIG SISTERS WASHTENAW COMMUNITY HEALTH AND SOCIAL SERVICES (CHASS) CENTER BIRMINGHAM PUBLIC SCHOOLS COMMUNITY HOUSING NETWORK, INC. -
Active Psych Program List 10.01.14
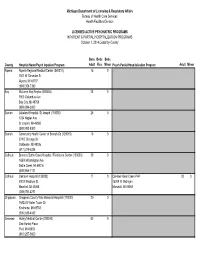
Michigan Department of Licensing & Regulatory Affairs Bureau of Health Care Services Health Facilities Division LICENSED ACTIVE PSYCHIATRIC PROGRAMS INPATIENT & PARTIAL HOSPITALIZATION PROGRAMS October 1, 2014 Listed by County Beds Beds Beds County Hospital Name/Psych Inpatient Program Adult Flex Minor Psych Partial Hospitalization Program Adult Minor Alpena Alpena Regional Medical Center (040010) 15 0 040010 1501 W Chisholm St Alpena, MI 49707 (989) 356-7390 Bay McLaren Bay Region (090050) 28 0 090050 1900 Columbus Ave Bay City, MI 48708 (989) 894-3000 Berrien Lakeland Hospital- St Joseph (110050) 26 0 110050 1234 Napier Ave St Jospeh, MI 49085 (269) 983-8300 Branch Community Health Center of Branch Co (120010) 16 0 120010 274 E Chicago St Coldwater, MI 49036 (517) 279-5326 Calhoun Bronson Battle Creek Hospital / Fieldstone Center (130030) 39 0 130030 165 N Washington Ave Battle Creek, MI 49016 (269) 964-7121 Calhoun Oaklawn Hospital (130080) 17 0 Oaklawn Bear Creek PHP 20 0 130080 200 N Madison St 15209 W Michigan Marshall, MI 49068 Marshall, MI 49068 (269) 781-4271 Chippewa Chippewa County War Memorial Hospital (170020) 20 0 170020 16523 S Water Tower Dr Kincheloe, MI 49788 (906) 635-4460 Genesee Hurley Medical Center (250040) 60 0 250040 One Hurley Plaza Flint, MI 48503 (810) 257-9000 Genesee McLaren Flint (250050) 36 0 McLaren Flint PHP 40 30 250050 401 S Ballenger Hwy 4448 Oak Bridge Dr Flint, MI 48532 Flint, MI 48532 (810) 342-2000 (810) 342-5333 Grand Munson Medical Center (280010) 14 0 Munson Medical Center PHP 15 0 Traverse -

Detroit, Michigan, Health Manufacturers (Ford, General Motors, and Chrysler (Now Care Market
Assessing Responses to Increased Provider Consolidation: Detroit Case Study Case Study Analysis: Assessing Responses to Increased The Detroit Health Care Market Provider Consolidation Sabrina Corlette, Jack Hoadley, and Olivia Hoppe November 2018 Rising health care prices have increased concerns about hospital and health system consolidation among policymakers, regulators, employers, and other purchasers of health coverage. Although merging hospitals and health systems claim they can achieve greater efficiencies through their consolidation, the economic literature almost universally finds that hospitals that merge have prices Macomb above those of surrounding hospitals.1 And increases in Oakland hospital prices have been a key factor driving the growth of Wayne commercial health insurance costs over the past decade.2 As prices have risen, employers have shifted an ever greater share of the costs to employees. Over the past ten years, the average worker contribution for family coverage has increased faster than the average employer contribution (65 percent vs. 51 percent). Indeed, employee Background, History, and Methodology 3 contributions have risen almost 300 percent since 1999. The Detroit metropolitan region, defined in this study to Further, the increased negotiating clout of a concentrated include Macomb, Oakland, and Wayne counties, is home provider sector influences payers’ ability to maximize to six hospital systems. These are: Ascension Health, value-improving practices, such as alternative payment Beaumont Health, Henry Ford Health System, McLaren models, quality improvement, and transparency efforts. Health Care Corporation, Tenet Healthcare, and Trinity Health. Three of the systems (Beaumont, Henry Ford, In a series of six market-level, qualitative case studies, and McLaren) operate solely in the state of Michigan. -

Mail Code Directory
Pink = Oakwood Site Code ( aka . Mail Code) is assigned to the physical location of your building. Ex . Research Bldg, 3811 W 13 Mile Rd is assigned Site Code 306. Blue = Beaumont Location Code is assigned to your location within the site code. Used for inside delivery of supplies Ex. Microbiology is inside 306, their Location Code is 306C02MICR Yellow = Botsford Site Codes double as Mail Codes – When addressing Inter dept envelopes (Staples # 91709), please use the 3 digit Site Code first. Only RED Site numbers receive inter-mail delivery NOTE: Site # New Name Address City Zip 001 Beaumont Hospital - Dearborn 18101 Oakwood Blvd Dearborn 48124 002 Beaumont Hospital - Wayne 33155 Annapolis Wayne 48184 005 Beaumont Hospital - Taylor 10000 Telegraph Taylor 48180 007 Beaumont Hospital - Trenton 5450 Fort St Trenton 48183 008 Beaumont Laboratory Services - Riverview 19020 Fort St Riverview 48193 009 Beaumont Learning & Innovation Center - Dearborn 18200 Oakwood Blvd Dearborn 48124 011 Beaumont Medical Building - Dearborn West 25045 Ford Rd Dearborn 48128 012 Beaumont Heart & Vascular Center - Dearborn 22060 Beech Rd Dearborn 48124 014 Beaumont Medical Center - Belleville 201 Third St Belleville 48111 015 Vacant 17000 King Road Brownstown 48183 016 Oakwood HC Center - Canton 7300 Canton Center Rd Canton 48187 021 Oakwood Healthcare Center - Mercury Drive 4900 Mercury Dr Dearborn 48126 024 Beaumont Medical Center - Southgate 15777 Northline Rd Southgate 48196 025 Beaumont Medical Center - Westland 2001 South Merriman Westland 48186 026 Oakwood -
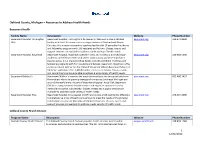
Oakland County, Michigan – Resources to Address Health Needs
Oakland County, Michigan – Resources to Address Health Needs Beaumont Health Facility Name Description Website Phone Number Beaumont Hospital, Farmington Beaumont Hospital, Farmington Hills opened in 1965 and is now a 330-bed beaumont.org 248-471-8000 Hills facility with Level II trauma status serving residents of Oakland and Wayne Counties. It is a major osteopathic teaching facility with 20 accredited residency and fellowship programs with 140 residents and fellows. Classes, events and support services are available to address a wide variety of health needs. Beaumont Hospital, Royal Oak Beaumont Hospital, Royal Oak opened in 1955 and is now a 1,070-bed major beaumont.org 248-898-5000 academic and referral center with Level I adult trauma and Level II pediatric trauma status. It is a major teaching facility with 40 accredited residency and fellowship programs with 434 residents and fellows. Beaumont, Royal Oak is the exclusive clinical partner for the Oakland University William Beaumont School of Medicine, with more than 1,400 Beaumont doctors on faculty. Classes, events and support services are available to address a wide variety of health needs. Beaumont Children’s Beaumont Children’s provides the most advanced care for young patients from beaumont.org 855-480-5437 the smallest infants to growing teenagers from across Southeast Michigan and around the world more. As part of Beaumont Hospital, Royal Oak, Beaumont Children’s comprehensive health services and expertise span nearly every medical and surgical subspecialty. Classes, events and support services are available to address a wide variety of health needs Beaumont Hospital, Troy Beaumont Hospital, Troy opened in 1977 and is now a 520-bed facility offering a beaumont.org 248-964-5000 comprehensive array of health care services to meet the needs of the growing communities it serves in Macomb and Oakland Counties. -
Beaumont Hospital, Wayne Implementation Strategy 2018 Update
Community Health Needs Assessment – 2016 Beaumont Hospital, Wayne Implementation Strategy 2018 Update Building healthier lives and communities. P19360g9_19360_091918 COMMUNITY HEALTH NEEDS ASSESSMENT IMPLEMENTATION STRATEGY The Patient Protection and Affordable Care Act health needs for this community (see box to right). (the PPACA) requires all tax-exempt hospitals to Significant health needs were identified as those assess the health needs of their community through where the qualitative data (interview and focus a community health needs assessment (CHNA) group feedback) and quantitative data (health once every three years. A CHNA is a written indicators) converged. Beaumont Health prioritized document developed for a hospital facility that these significant community healthcare needs defines the community served by the organization, based on the following: explains the process used to conduct the • Importance of the problem to the community assessment and identifies the salient health needs ensures the priorities chosen reflect the of the community. In addition, the CHNA must community experience. include a description of the process and criteria used in prioritizing the identified significant health • Alignment with the health system’s strengths is needs, and an evaluation of the implementation important to ensure we leverage our ability to strategies adopted as part of the most make an impact. recently conducted (2013) assessment. A CHNA • Resources criteria acknowledges that we need is considered conducted in the taxable year that to work within the capacity of our organization’s the written report of its findings, as described budget, partnerships, infrastructure, and available above, is approved by the hospital governing body grant funding. and made widely available to the public. -

PTAB Detroit
Detroit is the “Real McCoy” In July 2012, Detroit welcomed the opening of the Elijah J. McCoy United States Patent and Trademark Office, which holds the distinction of being the first satellite office located outside of the Washington D.C. area. Appropriately, the Office is named after Elijah J. McCoy, who secured more than 50 patents over his lifetime. McCoy was born in Ontario, Canada to fugitive slaves, and his family moved to Michigan when McCoy was a young child. After an apprenticeship abroad, McCoy returned back to Michigan to work as a fireman, an oiler, and a designer in a home-based machine shop. He is best known for inventing an automatic lubricator for oiling steam engines of locomotives and ships. Although others attempted to duplicate McCoy’s invention, none held up to the original. Legend has it that railroad engineers specifically seeking McCoy’s invention to avoid inferior copies of the device would ask, “Is it the real McCoy?” Why locate a patent office in Detroit, an aging city recovering from bankruptcy? Simple—the people. Descended from Native Americans, European, Asian, and Middle Eastern immigrants, and more recently transplanted southerners, their friendliness sets them apart from other areas of the country. In addition to being known for their friendliness and Midwestern values, Detroiters are also known for their grit and determination. Those who choose to stay here and those who choose to come here to live or work share an infectious excitement. Many embody the true entrepreneurial spirit of America and relish the opportunity to not just be a part of the status quo somewhere else, but to be ahead of the curve and to be a part of actually rebuilding a city to be better than it is. -

James Lynch, M.D. Interim President, Grosse Pointe and Troy
James Lynch, M.D. Interim President, Grosse Pointe and Troy James P. Lynch, M.D., is president of the Grosse Pointe and Troy acute care campuses for Beaumont Health, Michigan’s largest health care system, based on inpatient admissions and net patient revenue. He is responsible for strategy development, daily operations and financial performance of the 289-bed full- service community campus in Grosse Pointe and the 520-bed Troy campus, including its ambulatory, diagnostic and surgery centers. Prior to this role, Dr. Lynch served as chief medical officer at Beaumont, Troy, beginning in 2010. In this role, he closely collaborated with medical and hospital leadership, including the Medical Executive Committee, hospital president and elected chief of staff. He also served as chief of Colon and Rectal Surgery at Troy. Dr. Lynch has been a member of the medical staffs at Beaumont, Troy and Beaumont, Royal Oak since 1988. He is certified by the American Board of Colon and Rectal Surgery and is a fellow of the American Society of Colon and Rectal Surgeons. He is also a member of the Michigan Surgical Quality Collaborative and the National Surgical Quality Improvement Project, as well as a past president of the Michigan Society of Colon and Rectal Surgeons. He was named a “Top Doc” by Hour Detroit Magazine in 2010. Dr. Lynch received his medical degree from Wayne State University and performed his post-doctoral surgical training at Beaumont. He also has a master’s degree in business administration from Oakland University, and is an assistant professor at the Oakland University William Beaumont School of Medicine.