2018 Community Health Assessment Report
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Upper Mississippi River Conservation Opportunity Area Wildlife Action Plan
Version 3 Summer 2012 UPPER MISSISSIPPI RIVER CONSERVATION OPPORTUNITY AREA WILDLIFE ACTION PLAN Daniel Moorehouse Mississippi River Pool 19 A cooperative, inter-agency partnership for the implementation of the Illinois Wildlife Action Plan in the Upper Mississippi River Conservation Opportunity Area Prepared by: Angella Moorehouse Illinois Nature Preserves Commission Elliot Brinkman Prairie Rivers Network We gratefully acknowledge the Grand Victoria Foundation's financial support for the preparation of this plan. Table of Contents List of Figures .............................................................................................................................. ii Acronym List .............................................................................................................................. iii I. Introduction to Conservation Opportunity Areas ....................................................................1 II. Upper Mississippi River COA ..................................................................................................3 COAs Embedded within Upper Mississippi River COA ..............................................................5 III. Plan Organization .................................................................................................................7 IV. Vision Statement ..................................................................................................................8 V. Climate Change .......................................................................................................................9 -

Project Description
Chicago to Quad Cities Passenger Rail Project Grade Crossing Design Illinois DOT - Various Locations Project Description The project provides Program Management along with planning and preliminary engineering services for the Illinois Department of Transportation to implement passenger rail service on the Chicago to Iowa City corridor within the State of Illinois project limits. The Chicago-Iowa City Passenger Rail Service Development Program of Iowa and Illinois will establish passenger rail service between Chicago, the Quad Cities, Illinois and Iowa City, Iowa, 219.5 miles. The service will be hosted by BNSF Railway (BNSF) and Iowa Interstate Railroad (IAIS), and be operated by Amtrak. New stations will be established at Geneseo and Moline, Illinois (serving the Quad Cities); and Iowa City, Iowa. The service will be part of the Midwest Regional Rail Imitative (MWRRI) designated by the Secretary of Transportation as a high-speed rail corridor in 1992. The initial Chicago-Iowa City passenger-train service will consist of two roundtrip trains daily, operating at a maximum speed of 79 mph. Ridership is estimated by Amtrak at 246,800 passengers in the Program’s opening year, and 447,000 passengers per year by 2045. The alignment of the route is suited to high-speed passenger-train operation, and had previously hosted passenger trains exceeded 100-mph. Station access to major traffic sources such as the University of Iowa, and travel patterns are all favorable to high initial ridership. The States envision future increases in maximum speed to 110 mph, increases in frequency of trains, and extension of the service to Omaha, Nebraska. -

Health Care Strategic Planning
HEALTH Introducing CARE STRATEGIC . PLANNING ACCORD LIMITED HEALTH CARE STRATEGIC PLANNING 1 ACCORD LIMITED HEALTH CARE STRATEGIC PLANNING TABLE OF CONTENTS Introduction to ACCORD LIMITED ......................................................... 3 StrategicSTRATEGIC Planning PLANNING ................................ .................................................................................................................... 4 ACCORD’s’s Approach APPROACH ................................ ................................................................................................................... 6 WhatWHAT Differentiates DIFFERENTIATES ACCORD ................................ACCORD ............................................................................... 13 A PromisePROMISE to TOour ClientsOUR CLIENTS ................................ .............................................................................................. 14 ACCORD’s’s Other OTHER Services SERVICES ................................ ................................................................................................. 15 ACCORD’s’s Health HEALTH Care CARE Clients CLIENTS ................................ ........................................................................... 16 ACCORD’s’s Consulting CONSULTING Team ................................TEAM ...................................................................................... 2220 2 ACCORD LIMITED HEALTH CARE STRATEGIC PLANNING GENERAL INFORMATION ACCORD LIMITED (ACCORD) is -

The Rock Island Arsenal and Rock Island in the World Wars
Western Illinois Historical Review © 2020 Volume XI, Spring 2020 ISSN 2153-1714 ‘Rock Island Needs Machinists’: The Rock Island Arsenal and Rock Island in the World Wars By Jordan Monson Western Illinois University “Availability of workers… was vital to the successful operation of Rock Island Arsenal in the World War, just as it must be in any future military crisis in which the country may become involved.”1 Industries and businesses have a huge impact on the development of a community. No business can be successful without labor provided by communities, and communities rarely grow without the availability of jobs provided by businesses. In this same way, the Rock Island Arsenal has had a huge impact on the surrounding communities of Rock Island, Moline, Davenport, and Bettendorf, collectively known as the Quad Cities. Indeed, in an article published in 2018, Aarik Woods points out that the Rock Island Arsenal is far and away the largest employer in the region, and the economic impact of the Arsenal on the Quad Cities was more than one billion dollars.2 With that large of an economic impact, it is safe to say that the success of the Arsenal and the success of the Quad Cities are tied at the hip. However, the Rock Island Arsenal often goes through extreme variation in production and employment numbers, with “The Arsenal’s employment and production traditionally being cyclical in nature… increasing during national emergencies and declining during peacetime.”3 These mobilization and demobilization patterns of the Arsenal were most pronounced during the period between the first and second world wars. -

Quad Cities River Adventure
Great Rivers Country quad cities river Rock Island Moline adventure Coal Valley From the local experts Illinois City at Visit Quad Cities In the Quad Cities, you are the captain of your boat. Over three fun-filled days, you’ll experience the world-renowned Mississippi River and area waterways, discovering the history of this family of communities. Find out why the river bends to run directly east to west here; what plants and 3 days animals are native to the QC; and how this area grew up along the river. Take a break from exploring to enjoy QC favorites that are sure to satisfy. 80mi (Approx) Great Rivers Country Lagomarciano’s Celebration Belle Quad Cities Botanical Center Channel Cat Water Taxi Many attractions have reopened with limited capacity or different operating hours. Inquire with attractions ahead of time for up-to-date travel policies and health and safety information. Day 1 Moline & Rock Island Day 3 Coal Valley, Rock Island & Illinois City Get a great introduction to the Mississippi River with a ride on the Celebration Belle riverboat. The Now it’s time to direct your own boat. Lake riverboat’s captain narrates the cruise and shares George at the Loud Thunder Forest Preserve has some of the rich history of the area. You’ll view a variety of boats to rent. Try jon boats (small Blackhawk State Historical Site the largest roller dam in the world at Lock and two-person pontoon boats), kayaks, canoes, and Dam #15. Get a treat at Lagomarcino’s, a century- regular pontoon boats. -

Chicago Quad Cities
Welcome! www.connectthemidwest.com Chicago Quad Cities Project Description Purpose » Re-establish the passenger rail service between Chicago and the Quad Cities as part of the Midwest Regional Rail Initiative (MRRI) » Increase regional mobility, reduce roadway congestion, meet future travel demands, and provide an affordable alternative mode of transportation Funding » Federal award of $177 million in High-Speed and Intercity Passenger Rail (HSIPR) funds » State matching funds of $45 million Activities » Continuation of National Environmental Policy Act (NEPA) studies » Preliminary engineering for a corridor expansion program www.connectthemidwest.com Chicago Quad Cities Project Infrastructure Improvements New Stations » Moline » Geneseo Layover Facility » Rock Island Existing Rail Yard Improvements » Eola » Silvis Second Main Line Track » Between Rock Island and Silvis Yard Purchase of New Rail Equipment » Selected Manufacturer-Nippon Sharyo USA Group, Rochelle, IL Communication and Signal Enhancements www.connectthemidwest.com Chicago Quad Cities Project Benefits Economic Outcomes for the State of Illinois » Direct and indirect job creation » Generation of business revenue » Travel cost savings » Increased tourism opportunities Transportation Connectivity and Access » Creates connections to the Chicago and Quad Cities business hubs » Increases regional mobility » Addresses future travel demands » Provides comfortable, safe, affordable, and convenient travel option Reduction of Impacts to the Environment » Fuel efficient transportation -

Community Health Improvement Plan 2019-2021
Community Health Improvement Plan 2019-2021 Patricia Shouse, President, Trinity Health Foundation, and Vice President Patient and Community Advocacy Daniel Joiner, Director, Community Engagement Sherri Behr DeVrieze, Community Health Program Coordinator TABLE OF CONTENTS Part 1: Introduction Introduction 3-13 Part 2: Community Health Improvement Plan Community Health Improvement Plan Overview 14 Diabetes, Nutrition, Physical Activity & Weight 15-19 Heart Disease & Stroke 20-23 Mental/Behavioral Health & Substance Abuse 24-29 Cancer 30-32 Access to Healthcare Services 33-38 2 | P a g e Part 1: Introduction Introduction How We Got There The Community Health Needs Assessment (CHNA) was conducted by UnityPoint Health – Trinity and its partners in order to identify the greatest health needs in the community and to create and operationalize a strategy to best meet these needs. Trinity’s strategy development is known as the Community Health Improvement Plan (CHIP). Trinity has been involved in the assessment of its community’s health priorities for the past 18 years through its efforts in the establishment of a CHNA for the Quad Cities area beginning in 2002. In 2010, the Patient Protection and Affordable Care Act was enacted by Congress with the goal of improving access to healthcare services for Americans. As part of the Affordable Care Act, non-profit hospitals are required to submit a Community Health Needs Assessment and Improvement Plan every three years. In addition to our commitment to serving the needs of the community, Trinity’s CHIP also fulfills these regulatory requirements. In late 2014, UnityPoint Health - Trinity partnered with the Quad City Health Initiative and other community partners to begin the process of collecting data and planning the operationalization of the Community Health Improvement Plan for 2019-2021. -

2005 Most Wired Survey and Benchmarking Study
2012 Most Wired Survey Winners by State Alabama Cullman Regional Medical Center: Innovator Award winner Evergreen Medical Center: Most Wired–Small and Rural St. Vincent’s Hospital–Birmingham: Most Wired University of Alabama at Birmingham (UAB) Hospital: Most Wired Washington County Hospital, Chatom: Most Wired–Small and Rural Arizona Banner Health, Phoenix: Most Wired Tucson Medical Center: Most Wired Arkansas Stone County Medical Center, Mountain View: Most Wired–Small and Rural California Eisenhower Medical Center, Rancho Mirage: Most Wired Kaiser Permanente, Oakland: Most Improved Naval Hospital Lemoore: Most Wired–Small and Rural Rady Children's Hospital–San Diego: Most Wired San Francisco VA Medical Center: Most Wired Sharp HealthCare, San Diego: Most Wired Stanford Hospital and Clinics: Most Wired University of California Davis Health System, Sacramento: Most Wired University of California, San Diego Health System: Most Wired VA Palo Alto Health Care System: Most Wired VA Sierra Pacific Network, Mare Island: Most Wired Colorado Denver Health and Hospital Authority: Most Wired Poudre Valley Health System, Fort Collins: Most Wired Connecticut Hartford Hospital: Most Wired Middlesex Health System, Middletown: Most Wired MidState Medical Center, Meriden: Most Wired Saint Francis Care, Hartford: Most Wired William W. Backus Hospital, Norwich: Most Wired Yale New Haven Health System: Most Wired Delaware Alfred I. duPont Hospital for Children, Wilmington: Most Wired District of Columbia Washington, D.C. VA Medical Center: Most Wired Florida -
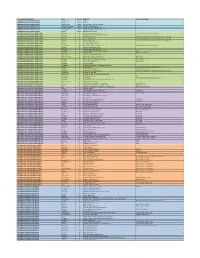
Participants List Through January 2020
REGIONAL GROUP NAME CITY STATE CENTER HEALTH SYSTEM(s) CANADIAN VASCULAR QUALITY INITIATIVE Montreal, QC Canada CHUM CANADIAN VASCULAR QUALITY INITIATIVE Gatineau Canada CISSSO CANADIAN VASCULAR QUALITY INITIATIVE Edmonton, AB Canada Covenant Health - Grey Nuns Hospital CANADIAN VASCULAR QUALITY INITIATIVE Kentville, Nova Scotia Canada Nova Scotia Health Authority CANADIAN VASCULAR QUALITY INITIATIVE Toronto, Ontario Canada Sunnybrook Health Sciences Centre CANADIAN VASCULAR QUALITY INITIATIVE Thunder Bay Canada Thunder Bay ReGional Health Sciences Centre CANADIAN VASCULAR QUALITY INITIATIVE Toronto Canada Toronto General Hospital CAROLINAS VASCULAR QUALITY GROUP (CVQG) BurlinGton NC Alamance ReGional Medical Center Cone Health System; Carolinas Healthcare CAROLINAS VASCULAR QUALITY GROUP (CVQG) Anderson SC AnMed Health Medical Center (AnMed Health) CAROLINAS VASCULAR QUALITY GROUP (CVQG) Concord NC Atrium Health Carrabus The Charlotte-MecklenburG Hospital Authority d/b/a Atrium Health CAROLINAS VASCULAR QUALITY GROUP (CVQG) Charlotte NC Atrium Health Pineville The Charlotte-MecklenburG Hospital Authority d/b/a Atrium Health CAROLINAS VASCULAR QUALITY GROUP (CVQG) Monroe NC Atrium Health Union The Charlotte-MecklenburG Hospital Authority d/b/a Atrium Health CAROLINAS VASCULAR QUALITY GROUP (CVQG) louidiana SC Beaufort Memorial Hospital CAROLINAS VASCULAR QUALITY GROUP (CVQG) Hickory NC Catawba Valley Medical Center CAROLINAS VASCULAR QUALITY GROUP (CVQG) Greensboro NC Cone Health Heart & Vascular Center Cone Health System; Carolinas Healthcare -

Region Three: Peoria/Quad Cities Region Three Covers the Following
Region Three: Peoria/Quad Cities Region Three covers the following 14 counties: The counties of Fulton, Hancock, Henderson, Henry, Knox, Marshall, McDonough, Mercer, Peoria, Rock Island, Stark, Tazewell, Warren and Woodford are located in Region Three: Peoria/Quad Cities. Landfills Nine landfills in the Peoria/Quad Cities area reported more than 263.1 million gate cubic yards of capacity remaining at the beginning of 2012. Total capacity was 4.3 million gate cubic yards more than the amount that was reported the previous year. Total capacity in the region increased 1.7 percent from the previous year. These landfills in Region Three accounted for 25.1 percent of the more than one billion gate cubic yards of disposal capacity remaining statewide on Jan. 1, 2012. Fifty-four years of landfill life remaining The longest amount of landfill life is 54 years in both the Peoria/Quad Cities region and the Southern Illinois Region. Chicago Metropolitan Region had the least, with 12 years. Waste disposal amounts increased by 5.7 percent The Region’s eight landfills active in 2011 reported accepting more than 4.8 million gate cubic yards of waste for disposal. However, in Region Three, 260,257 more gate cubic yards of waste was received than during 2010, up 5.7 percent. Twenty-one percent of waste receipts came from seven other states Of the almost 46.2 million gate cubic yards of solid waste disposed in Illinois’ landfills in 2011, 13.3 percent was imported from 11 other states. For Region Three, 21.3 percent of its waste receipts originated from seven of these 12 states. -

Muscatine County Health Improvement Plan
2019-2021 Muscatine County Health Improvement Plan Improving the health of the people and communities we serve. Credits and Acknowledgements We wish to thank those involved for their invaluable collaboration and input toward the Muscatine County’s health needs assessment and improvement planning process. Muscatine County Board of Health • William Koellner, Chairperson • Neva Rettig-Baker • Brian Wright • Michael Maharry, M.D. • Karen Harper UnityPoint Health – Trinity Muscatine Board of Directors • Daniel Stein, Chairperson • Rhea Allen, M.D. • Toni Eller, O.D. • Stacie Fidlar • Troy Fridley • Prasad Nadkarni, M.D. • Scott Natvig • Suneel Parvathareddy, M.D. • Mark Peterson • Jerry Riibe, Ph.D. • Charla Schafer • Richard Seidler • Candace Terrill • Guadalupe Vazquez • Robert Weis, M.D. Community Effectiveness Stakeholder Committee • Rhea Allen, M.D., Trinity Muscatine Occupational Medicine • John Beckey, Beckey Insurance and Financial Services, Inc. • Troy Fridley, Kent Corporation • Cory Garvin, R.Ph., Pharm.D., Wester Drug • Angela Johnson, Trinity Regional Health System • Janell Kassel, O.D., Family Eye Center • Jay Logel, Community Volunteer • Scott Natvig, Community Volunteer • Mark Peterson, WTC Communications • Jerry Riibe, Muscatine Community School District • Charla Schafer, Community Foundation of the Greater Muscatine Area Muscatine County Health Improvement Plan 2019-2021 2 | Page • Daniel Stein, CBI Bank and Trust • Guadalupe Vazquez, Guadalajara and North Construction, LLC • Robert Weis, M.D., UnityPoint Clinic Internal -

Causes Local
Causes B07002 Camps for Kids with Health Challenges B08664 Alzheimer's Association, Greater Iowa, Burlington Provide a recreational camp experience that improves the B08665 Alzheimer's Association, Greater Iowa, Council Bluffs quality of life for children managing long term health B08666 Alzheimer's Association, Greater Iowa, Davenport conditions. B08667 Alzheimer's Association, Greater Iowa, Dubuque B07004 Crisis and Disaster Community Health B08668 Alzheimer's Association, Greater Iowa, Fort Dodge Provide vital health and critical resource assistance to B08669 Alzheimer's Association, Greater Iowa, Sioux City support communities around the world responding to B00339 Alzheimer's Association, Greater Iowa, West Des crises and natural disasters. Moines B07008 Drive for a Cure B00660 American Diabetes Association, Iowa, North Liberty Help advance research to find a cure for the diseases that impact the most Americans. B00661 American Diabetes Association, Iowa, Urbandale B02114 Every Kid Deserves B00889 American Lung Association in Iowa Support the best children’s health charities improving child B01045 Arthritis Foundation, Heartland Region, Iowa well being in the United States. B01401 Camp Hertko Hollow B07003 Health & Safety at School B01734 Crohn's & Colitis Foundation, Iowa Chapter Ensure that students have a safe and healthy environment B01800 Cystic Fibrosis Foundation, Iowa Chapter to learn and grow. B01981 Easterseals Iowa B07005 Health Services for Vulnerable Populations B02058 Epilepsy Foundation of North-Central Illinois, Iowa & Help provide critical health services to vulnerable Nebraska populations across the nation that are struggling to get the B02541 Huntington's Disease Society of America, Iowa Chapter care and health management tools they need. B02690 JDRF International, Eastern Iowa Chapter B07009 Hero’s Health B02691 JDRF International, Greater Iowa Chapter Protect the physical and mental health of our nation’s military, veterans and first responders.