New Zealand Data Sheet 1 Vivaxim Solution for Injection 2 Qualitative and Quantitative Composition 3 Pharmaceutical Form 4 Clini
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Rapport 2008
rapport 2008 Reseptregisteret 2004-2007 The Norwegian Prescription Database 2004-2007 Marit Rønning Christian Lie Berg Kari Furu Irene Litleskare Solveig Sakshaug Hanne Strøm Rapport 2008 Nasjonalt folkehelseinstitutt/ The Norwegian Institute of Public Health Tittel/Title: Reseptregisteret 2004-2007 The Norwegian Prescription Database 2004-2007 Redaktør/Editor: Marit Rønning Forfattere/Authors: Christian Lie Berg Kari Furu Irene Litleskare Marit Rønning Solveig Sakshaug Hanne Strøm Publisert av/Published by: Nasjonalt folkehelseinstitutt Postboks 4404 Nydalen NO-0403 Norway Tel: + 47 21 07 70 00 E-mail: [email protected] www.fhi.no Design: Per Kristian Svendsen Layout: Grete Søimer Acknowledgement: Julie D.W. Johansen (English version) Forsideillustrasjon/Front page illustration: Colourbox.com Trykk/Print: Nordberg Trykk AS Opplag/ Number printed: 1200 Bestilling/Order: [email protected] Fax: +47-21 07 81 05 Tel: +47-21 07 82 00 ISSN: 0332-6535 ISBN: 978-82-8082-252-9 trykt utgave/printed version ISBN: 978-82-8082-253-6 elektronisk utgave/electronic version 2 Rapport 2008 • Folkehelseinstituttet Forord Bruken av legemidler i befolkningen er økende. En viktig målsetting for norsk legemiddelpolitikk er rasjonell legemiddelbruk. En forutsetning for arbeidet med å optimalisere legemiddelbruken i befolkningen er kunnskap om hvilke legemidler som brukes, hvem som bruker legemidlene og hvordan de brukes. For å få bedre kunnskap på dette området, vedtok Stortinget i desember 2002 å etablere et nasjonalt reseptbasert legemiddelregister (Reseptregisteret). Oppgaven med å etablere registeret ble gitt til Folkehelseinstituttet som fra 1. januar 2004 har mottatt månedlige opplysninger fra alle apotek om utlevering av legemidler til pasienter, leger og institusjoner. Denne rapporten er første utgave i en planlagt årlig statistikk fra Reseptregisteret. -
Typhoid Vaccine W H a T Y O U N E E D T O K N O W
TYPHOID VACCINE W H A T Y O U N E E D T O K N O W Many Vaccine Information Statements are available in Spanish and other languages. See www.immunize.org/vis. What is typhoid? •Travelers to parts of the world where typhoid is 1 common. (NOTE: typhoid vaccine is not 100% Typhoid (typhoid fever) is a serious disease. It is effective and is not a substitute for being caused by bacteria called Salmonella Typhi. careful about what you eat or drink.) Typhoid causes a high fever, weakness, stomach •People in close contact with a typhoid carrier. pains, headache, loss of appetite, and sometimes a •Laboratory workers who work with Salmonella rash. If it is not treated, it can kill up to 30% of Typhi bacteria. people who get it. Some people who get typhoid become “carriers,” Inactivated Typhoid Vaccine (Shot) who can spread the •Should not be given to children younger than 2 disease to years of age. others. •One dose provides protection. It should be given Generally, at least 2 weeks before travel to allow the vaccine people get time to work. typhoid from contaminated •A booster dose is needed every 2 years for people food or water. Typhoid is not common in the U.S., who remain at risk. and most U.S. citizens who get the disease get it Live Typhoid Vaccine (Oral) while traveling. Typhoid strikes about 21 million people a year around the world and kills about •Should not be given to children younger than 6 200,000. years of age. -
New Zealand Data Sheet 1 Avaxim Suspension for Injection 2 Qualitative and Quantitative Composition 3 Pharmaceutical Form 4 Clin
NEW ZEALAND DATA SHEET 1 AVAXIM SUSPENSION FOR INJECTION Hepatitis A virus (inactivated, adsorbed) 2 QUALITATIVE AND QUANTITATIVE COMPOSITION Avaxim is a sterile suspension for injection containing formaldehyde-inactivated hepatitis A virus (GBM strain) adsorbed onto aluminium hydroxide. Each 0.5mL dose contains: Active ingredient: Hepatitis A virus* ………………………………………………160 antigen units** * GBM strain cultured on MRC-5 human diploid cells. MRC-5 is a cell line that was derived from human embryonic lung tissue in the 1960s. ** In the absence of an international standardised reference, the antigen content is expressed using an in-house reference. The manufacture of this product includes exposure to bovine derived materials. No evidence exists that any case of vCJD (considered to be the human form of bovine spongiform encephalopathy) has resulted from the administration of any vaccine product. Contains phenylalanine and residual neomycin. For the full list of excipients, see Section 6.1 List of excipients. 3 PHARMACEUTICAL FORM Suspension for injection Avaxim is a cloudy, whitish suspension. 4 CLINICAL PARTICULARS 4.1 THERAPEUTIC INDICATIONS Avaxim is indicated for active immunisation against hepatitis A infection in adults and children 2 years and over. Vaccination against viral hepatitis A is recommended for individuals who are or will be at increased risk of infection: • travellers to areas of moderate or high endemicity for hepatitis A Property of the Sanofi group - strictly confidential ava-ccdsv10-dsv5-24may21 Page 1 • visitors to rural and remote indigenous communities • child day-care and pre-school personnel • the intellectually disabled and their carers • health care providers • sewerage workers • men who have sex with men • injecting drug users • patients with chronic liver disease • haemophiliacs who may receive pooled plasma concentrates 4.2 DOSE AND METHOD OF ADMINISTRATION The dose is 0.5 mL for each injection. -

Vaccine Adjuvants Derived from Marine Organisms
biomolecules Review Vaccine Adjuvants Derived from Marine Organisms Nina Sanina Department of Biochemistry, Microbiology and Biotechnology, School of Natural Sciences, Far Eastern, Federal University, Sukhanov Str., 8, Vladivostok 690091, Russia; [email protected]; Tel.: +7-423-265-2429 Received: 10 July 2019; Accepted: 1 August 2019; Published: 3 August 2019 Abstract: Vaccine adjuvants help to enhance the immunogenicity of weak antigens. The adjuvant effect of certain substances was noted long ago (the 40s of the last century), and since then a large number of adjuvants belonging to different groups of chemicals have been studied. This review presents research data on the nonspecific action of substances originated from marine organisms, their derivatives and complexes, united by the name ‘adjuvants’. There are covered the mechanisms of their action, safety, as well as the practical use of adjuvants derived from marine hydrobionts in medical immunology and veterinary medicine to create modern vaccines that should be non-toxic and efficient. The present review is intended to briefly describe some important achievements in the use of marine resources to solve this important problem. Keywords: squalene; cucumariosides; chitosan; fucoidans; carrageenans; laminarin; alginate 1. Introduction The oil-in-water-based complete Freund’s adjuvant developed by Jules Freund and Katherine McDermott in 40s of last century is the first vaccine adjuvant. The basis of immune stimulation and provide immunologists with a way to stimulate the production of antibodies and cellular immune responses to weak antigens. This elaboration allowed to establish the basis of immune stimulation and provide immunologists with an instrument to stimulate the production of antibody and cellular immune responses to weak antigens. -

2021 Medicare Vaccine Coverage Part B Vs Part D
CDPHP® Medicare Advantage Vaccine Coverage Guide Part B (Medical) vs. Part D (Pharmacy) Medicare Part B (Medical): Medicare Part D (Pharmacy): Vaccinations or inoculations Vaccinations or inoculations are included when the administration is (except influenza, pneumococcal, reasonable and necessary for the prevention of illness. and hepatitis B for members at risk) are excluded unless they are directly related to the treatment of an injury or direct exposure to a disease or condition. • Influenza Vaccine (Flu) • BCG Vaccine • Pneumococcal Vaccine • Diphtheria/Tetanus/Acellular Pertussis Vaccine (ADACEL, (Pneumovax, Prevnar 13) BOOSTRIX, DAPTACEL, INFANRIX) • Hepatitis B Vaccine • Diphtheria/Tetanus/Acellular Pertussis/Inactivated Poliovirus (Recombivax, Engerix-B) Vaccine (KINRIX, QUADRACEL) for members at moderate • Diphtheria/Tetanus Vaccine (DT, Td, TDVAX, TENIVAC) to high risk • Diphtheria/Tetanus/Acellular Pertussis/Inactivated Poliovirus Vac • Other vaccines when directly cine/ Haemophilus Influenzae Type B Conjugate Vaccine (PENTACEL) related to the treatment of an • Diphtheria/Tetanus/Acellular Pertussis/Inactivated Poliovirus injury or direct exposure to a Vaccine/Hepatitis B Vaccine (PEDIARIX) disease or condition, such as: • Haemophilus Influenzae Type B Conjugate Vaccine (ActHIB, PedvaxHIB, • Antivenom Sera Hiberix) • Diphtheria/Tetanus Vaccine • Hepatitis A Vaccine, Inactivated (VAQTA) (DT, Td, TDVAX, TENIVAC) • Hepatitis B Vaccine, Recombinant (ENGERIX-B, RECOMBIVAX HB) • Rabies Virus Vaccine for members at low risk (RabAvert, -

Elif Fatma Sen BW.Indd
Use and Safety of Respiratory Medicines in Children E. F. Şen EEliflif FFatmaatma SSenen BBW.inddW.indd 1 003-01-113-01-11 115:175:17 The work presented in this thesis was conducted at the Department of Medical Informatics of the Erasmus University Medical Center, Rotterdam. The research reported in thesis was funded by the European Community’s 6th Framework Programme. Project number LSHB-CT-2005-005216: TEDDY: Task force in Europe for Drug Development for the Young. The contributions of the participating primary care physicians in the IPCI, Pedianet and IMS-DA project are greatly acknowledged. Financial support for printing this thesis was kindly provided by the department of Medical Informatics – Integrated Primary Care Information (IPCI) project of the Erasmus University Medi- cal Center; and by the J.E. Jurriaanse Stichting in Rotterdam. Cover: Optima Grafi sche Communicatie Printed by: Optima Grafi sche Communicatie Elif Fatma Şen Use and Safety of Respiratory medicines in Children ISBN: 978-94-6169-003-6 © E.F. Şen, Rotterdam, the Netherlands, 2011. All rights reserved. No part of this thesis may be reproduced, stored in a retrieval system, or transmitted in any form or by any means, without prior written permission of the holder of the copyright. EEliflif FFatmaatma SSenen BBW.inddW.indd 2 003-01-113-01-11 115:175:17 Use and Safety of Respiratory Medicines in Children Het gebruik en de bijwerkingen van respiratoire medicijnen in kinderen Proefschrift Ter verkrijging van de graad van doctor aan de Erasmus Universiteit Rotterdam op gezag van de rector magnifi cus Prof.dr. -

Safety and Efficacy of Antiviral Therapy for Prevention of Cytomegalovirus Reactivation in Immunocompetent Critically Ill Patien
1 2 3 PROJECT TITLE 4 Anti-viral Prophylaxis for Prevention of Cytomegalovirus (CMV) Reactivation in Immunocompetent 5 Patients in Critical Care 6 7 STUDY ACRONYM 8 Cytomegalovirus Control in Critical Care - CCCC 9 10 APPLICANTS 11 Dr Nicholas Cowley 12 Specialty Registrar Anaesthesia and Intensive Care Medicine, Intensive Care Research Fellow 13 Queen Elizabeth Hospital Birmingham 14 15 Professor Paul Moss 16 Professor of Haematology 17 Queen Elizabeth Hospital Birmingham 18 19 Professor Julian Bion 20 Professor of Intensive Care Medicine 21 Queen Elizabeth Hospital Birmingham 22 23 Trial Virologist Trial Statistician 24 Dr H Osman Dr P G Nightingale 25 Queen Elizabeth Hospital Birmingham University of Birmingham CCCC CMV Protocol V1.7, 18th September 2013 1 Downloaded From: https://jamanetwork.com/ on 09/23/2021 26 CONTENTS 27 Substantial Amendment Sept 18th 2013 4 28 1 SUMMARY OF TRIAL DESIGN .......................................................................................................... 5 29 2 QEHB ICU Duration of Patient Stay ................................................................................................. 6 30 3 SCHEMA - QEHB PATIENT NUMBERS AVAILABLE FOR RECRUITMENT ........................................... 6 31 4 INTRODUCTION ............................................................................................................................... 7 32 4.1 CMV latent infection is widespread ........................................................................................ 7 33 4.2 CMV Reactivation -

Routine Immunizations
Drug and Biologic Coverage Policy Effective Date ............................................... 7/1/2021 Next Review Date ......................................... 4/1/2022 Coverage Policy Number .................................. 9001 Routine Immunizations Table of Contents Related Coverage Resources Coverage Policy ................................................... 1 Preventive Care Services General Background ............................................ 2 Covid-19 Vaccine Coding/Billing Information .................................... 3 References .......................................................... 7 INSTRUCTIONS FOR USE The following Coverage Policy applies to health benefit plans administered by Cigna Companies. Certain Cigna Companies and/or lines of business only provide utilization review services to clients and do not make coverage determinations. References to standard benefit plan language and coverage determinations do not apply to those clients. Coverage Policies are intended to provide guidance in interpreting certain standard benefit plans administered by Cigna Companies. Please note, the terms of a customer’s particular benefit plan document [Group Service Agreement, Evidence of Coverage, Certificate of Coverage, Summary Plan Description (SPD) or similar plan document] may differ significantly from the standard benefit plans upon which these Coverage Policies are based. For example, a customer’s benefit plan document may contain a specific exclusion related to a topic addressed in a Coverage Policy. In the event -
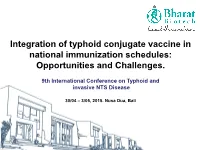
Integration of Typhoid Conjugate Vaccine in National Immunization Schedules: Opportunities and Challenges
Integration of typhoid conjugate vaccine in national immunization schedules: Opportunities and Challenges. Integration of typhoid9th conjugateInternational vaccine Conferencein national immunization on Typhoid schedules: and Opportunities and invasiveChallenges. NTS Disease 30/04 – 3/05, 2015. Nusa Dua, Bali Objective Review the existing clinical data on Vi conjugate vaccines, based on literature and our experience with Typbar-TCV to ascertain data sufficiency to assist global policy formualtion. Presentation Outline • Need for typhoid vaccine – Disease burden • Typhoid conjugate vaccines – Key considerations • Available data from typhoid conjugate vaccines (TCV) • Programmatic considerations • Integration of TCV into childhood immunization programs Typhoid epidemiology Disease Burden This disease is endemic in most developing countries. Cases/100,00 persons Highly Endemic >100 Endemic 10-100 Sporadic <10 21 million cases worldwide, mortality estimates of 216,000 to 600,000. http://www.who.int/immunization/topics/en/ http://www3.chu-rouen.fr/Internet/services/sante_voyages/pathologies/typhoide/ Age stratified disease burden 0.4 0.3 0.2 0.1 0 Proportion of Cases of Proportion Age groups Crump JA, et al. Bull World Health Organ 2004;82:346-353 Typhoid fever incidence – Asia and Africa • High incidence of typhoid fever in the region. • High incidence in urban slums; rates similar • Substantial regional variation in incidence. to those from Asia. • “Modified” Passive srvlnce. • Lower burden in rural children from Ghana (and Lwak, Kenya), compared to urban Ochiai RL, et al. Bull World Health Organ 2008;86:260-268. Breiman, RF et. al, PLoS One. 2012; 7(1): e29119. areas; regional differences Marks, F et. al, Emerg Infect Dis. 2010; 16(11): 1796–1797. -

Caspofungin II-02
ANNEX I ANNEX I SUMMARY OF PRODUCT CHARACTERISTICS 1 1. NAME OF THE MEDICINAL PRODUCT Caspofungin MSD 50 mg Powder for concentrate for solution for infusion 2. QUALITATIVE AND QUANTITATIVE COMPOSITION Each vial contains 50 mg Caspofungin equivalent to 55.5 mg caspofungin acetate. For excipients, see 6.1. 3. PHARMACEUTICAL FORM Powder for concentrate for solution for infusion. The vial contains a white to off-white compact, lyophilised powder. 4. CLINICAL PARTICULARS 4.1 Therapeutic indications · Treatment of invasive candidiasis in non-neutropaenic adult patients. · Treatment of invasive aspergillosis in adult patients who are refractory to or intolerant of amphotericin B, lipid formulations of amphotericin B and/or itraconazole. Refractoriness is defined as progression of infection or failure to improve after a minimum of 7 days of prior therapeutic doses of effective antifungal therapy. 4.2 Posology and method of administration Caspofungin MSD should be initiated by a physician experienced in the management of invasive fungal infections. After reconstitution and dilution, the solution should be administered by slow intravenous infusion over approximately 1 hour. Do not mix or co-infuse Caspofungin MSD with other medicines, as there are no data available on the compatibility of Caspofungin MSD with other intravenous substances, additives, or medicinal products. DO NOT USE DILUENTS CONTAINING GLUCOSE, as Caspofungin MSD is not stable in diluents containing glucose. For reconstitution directions see section 6.6. Both 70 mg and 50 mg vials are available. Invasive Candidiasis or Invasive Aspergillosis: A single 70-mg loading dose should be administered on Day-1, followed by 50 mg daily thereafter. -
1 SUMMARY of PRODUCT CHARACTERISTICS 1. NAME of the MEDICINAL PRODUCT ANCOTIL 500 Mg, Tablet 2. QUALITATIVE and QUANTITATIVE
Flucytosine 500 mg Tablets WHOPAR part 4 March 2018 2014 (MEDA Pharma, France) HA693 Suppliers submission of the SRA approved text SUMMARY OF PRODUCT CHARACTERISTICS 1. NAME OF THE MEDICINAL PRODUCT ANCOTIL 500 mg, tablet 2. QUALITATIVE AND QUANTITATIVE COMPOSITION Flucytosine 500 mg Per tablet. 3. PHARMACEUTICAL FORM Tablet. 4. CLINICAL PARTICULARS 4.1. Therapeutic indications Severe systemic fungal infections with susceptible pathogens, as an alternative or when switching from parenteral use, particularly: candidiasis, cryptococcosis, chromoblastomycosis and certain forms of aspergillosis. Combination with another antifungal agent: Flucytosine must be used in combination, in order to avoid as much as possible the selection of resistant mutations, especially in the treatment of candidiasis and cryptococcosis. Combination with amphotericin B is often synergistic and never antagonistic. 4.2. Posology and method of administration Oral use. Posology Dosages range from 100 to 200 mg/kg per day, depending on the nature of the infection, its site and sensitivity of the causative agent. The daily dosage must be divided into 3 or 4 oral doses. USE IN PATIENTS WITH RENAL IMPAIRMENT Doses must be administered at longer intervals, according to the following dosing regimen: CREATININE CLEARANCE SINGLE DOSE INTERVAL ≥ 40 mL/min 25 to 50 mg/kg 6 hours 20≤Cl<40 mL/min 25 to 50 mg/kg 12 hours 10≤Cl<20 mL/min 25 to 50 mg/kg 24 hours Cl < 10 mL/min Single dose of 25 mg/kg, then plasma monitoring 12 hours after the initial dose, before repeating the dose. PATIENTS ON DIALYSIS Since flucytosine is dialysable, the dose of this medicinal product must be repeated after each blood‐cleansing session. -

Weekly Epidemiological Record Relevé Épidémiologique Hebdomadaire
2017, 92, 13-20 No 2 Weekly epidemiological record Relevé épidémiologique hebdomadaire 13 JANUARY 2017, 92th YEAR / 13 JANVIER 2017, 92e ANNÉE No 2, 2017, 92, 13–20 http://www.who.int/wer Global Advisory Committee Comité consultatif mondial Contents on Vaccine Safety, pour la sécurité des vaccins, er 13 Global Advisory Committee on 30 November – 1 December 30 novembre - 1 décembre Vaccine Safety, 30 November 2016 2016 – 1 December 2016 The Global Advisory Committee on Le Comité consultatif mondial pour la sécurité Vaccine Safety (GACVS), an independent des vaccins (GACVS) est un organe consultatif Sommaire expert clinical and scientific advisory indépendant composé d’experts cliniques et 13 Comité consultatif mondial body, provides WHO with scientifically scientifiques qui fournissent à l’OMS des pour la sécurité des vaccins, rigorous advice on vaccine safety issues of conseils d’une grande rigueur scientifique sur 30 novembre - 1er décembre potential global importance.1 GACVS held des problèmes de sécurité des vaccins suscep- 2016 its 35th meeting in Geneva, Switzerland, tibles d’avoir une portée mondiale.1 Le GACVS on 30 November and 1 December 2016.2 a tenu sa 35e réunion à Genève (Suisse) les The Committee examined 2 generic issues: 30 novembre et 1er décembre 2016.2 Il a abordé updates on its operations following a 2 questions génériques, avec une mise à jour review conducted in 2014, and progress sur ses activités suite à une analyse réalisée with developing the Vaccine Safety Net. It en 2014 et un aperçu des progrès accomplis also reviewed vaccine-specific safety issues dans la mise en place du Réseau pour la sécu- concerning typhoid vaccines, yellow fever rité des vaccins.