MSHSAA Brain Injury Report
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
THE KEY VOL 113 NO 3 FALL 1996.Pdf
Com Com Surfing the ' et 61st Bien · al Conventi , theKAPPACONNECTION Kappa Kappa Gamma is pleased to offer The Kappa Connection as a service to its membership. As Kappas, we have the opportunity to bond with one another in sisterhood. Our individual talents, skills, and interests are tremendously valuable, especially when shared with others, and The Kappa Connection connects sisters for the benefit of each. The Kappa Connection is a database of personal information about participating alumnae and collegians, designed to connect women of all ages. Some examples: • Undergraduates can access professional women to discuss their career experiences. • Women relocating or pursuing a new interest can search for similar Kappas in their geographical area. • Kappas can locate other Kappas with certain skills and interests. • Graduating Kappas can make connections with alumnae. • Kappas of any age may find a mentor or new friend. Accessing this information is easy! Just call Headquarters at 614/228-6515 and a staff member can help you obtain a list that meets your needs! If you are interested in finding the alumnae association nearest you, please contact Headquarters for more information at 614/228-6515. The following list corresponds to the survey on the back cover of the magazine. OCCUPATION CLUSTERS AGRI Agriculture & Environment: Conservation, HOME Home Economics: Homemaker, Child rearing, Forestry, Horticulture, Landscaping, Recycling, Wildlife Family Planning ARCH Architecture, Engineering & Design: Drafting, HOSP Hospitality: Catering, Chef, -

The Maneater Daily: Marches and Wiretappin
Subscribe Past Issues Translate RSS The Maneater Daily View this email in your browser Monday, January 30, 2017 The weekend’s warm weather continues into the week. Today’s high will be 55 degrees, and the low will be 35. It’ll be partly cloudy throughout the day. University of Missouri professor Melissa Stormont lays flowers on the steps of the Islamic Center of Central Missouri. | Lane Burdette/Photographer Local citizens hold solidarity march in Columbia in response to Trump's "Muslim ban" President Donald Trump signed an executive order Friday that limits the immigration from seven majority Muslim countries. The rally started in Peace Park to stand with local Muslims. A representative of the Islamic Center of Central Missouri led about 200 people from the park to the mosque at the corner of Fifth and Locust streets, where they were greeted with cookies, snacks and juice. The marchers left their signs and flowers on the front steps of the mosque and then returned to Peace Park. CPD faces allegations of illegally recording client-attorney calls The complaint was filed against the Columbia Police Department by attorney Stephen Wyse on Jan. 23. Wyse filed the complaint after he read about a drunk driving case in the Columbia Daily Tribune, in which cops violated attorney-client privilege by covertly observing and recording the conversation. Federal law makes it illegal to intentionally intercept, disclose or use any wire, oral or electronic communication through the use of a “device,” and law enforcement officers may only wiretap a conversation in which one of the parties involved in the conversation has consented to the recording. -

For Those Who Make, Cover and Influence the News 2127 Innerbelt Business Center Drive St
Office For those who make, cover and influence the news 2127 Innerbelt Business Center Drive St. Louis, MO 63114 July 13, 2017 PHONE: (314) 449-8029 FAX: (314) 317-0031 Media Contact: [email protected] Glenda Partlow, Executive Director www.stlpressclub.org St. Louis Press Club, 314-449-8029 Mail P.O. Box 410522 FOR IMMEDIATE RELEASE: Creve Coeur, MO 63141 Board of Directors PRESS CLUB RECOGNIZES 16 STUDENTS AT SCHOLARSHIP LUNCHEON OFFICERS William Greenblatt PRESIDENT St. Louis, MO – The St. Louis Press Club with the St. Louis Journalism Foundation Tom Eschen* IMMEDIATE PAST-PRESIDENT held its annual scholarship luncheon on Tuesday, July 11 at the International Photography Cynthia Kagan Frohlichstein Janet Scott VICE PRESIDENT --PROGRAMMING Hall of Fame and Museum. The event was catered by Urban Canvas. Trish Muyco-Tobin VICE PRESIDENT -- MEMBERSHIP Kameel Stanley and Tim Lloyd, St. Louis Public Radio reporters and podcasters, Margaret S. Gillerman VICE PRESIDENT-- PUBLICITY Glynelle Wells were the featured speakers at the event, introduced by Outreach Specialist Linda Lockhart. Tom Eschen* VICE PRESIDEN T -- FUNDRAISING They spoke about the nature of podcasting and how pivotal moments are central to the Alice Handelman* VIE PRESIDENT -- NOMINATING Claudia Burris survival of media. VICE PRESIDENT – SCHOLARSHIPS Benjamin Lipman TREASURER Kent Martin SECRETARY BOARD MEMBERS Claire Applewhite Joan Lee Berkman Joe Bonwich Jessica Z. Brown Charlene Bry Amanda Galloway Richard Gavatin Denise Hollinshed Ellen Futterman Linda Lockhart Pamela -

@Mizzoubaseball
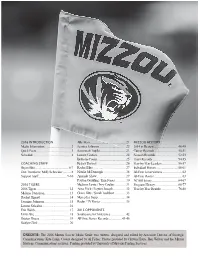
@MIZZOUBASEBALL 1 @MIZZOUBASEBALL TABLE OF CONTENTS MEDIA INFORMATION Quick Facts _________________________ 2 Mizzou Communications Staff ____________ 3 Roster - Numerical ____________________ 4 Roster - Alphabetical __________________ 5 University/Athletics Leadership __________6-8 MEET THE TIGERS Connor Brumfield / Cameron Dulle _________ 9 Paul Gomez / Jordan Gubelman __________ 10 Zach Hanna / Spencer Juergens _________ 11 Tyler LaPlante / Trevor Mallett ___________ 12 Tony Ortiz / Jacob Cantleberry ___________ 13 Chris Cornelius / Austin James __________ 14 Art Joven / Jake Matheny ______________ 15 Kameron Misner / TJ Sikkema ___________ 16 Lukas Veinbergs / Peter Zimmerman ______ 17 Luke Anderson / Konnor Ash ____________ 18 Ian Bedell / Thomas Broyles ____________ 19 Trey Dillard / Chad McDaniel ____________ 20 Alex Peterson / Clayton Peterson _________ 21 Cameron Pferrer / Mark Vierling _________ 22 Seth Halvorsen / Josh Holt Jr. ____________ 23 Nick Lommen / Luke Mann _____________ 23 Tre Morris / Ty Olejnik _________________ 24 Trae Robertson / Tommy Springer ________ 24 Cameron Swanger / Nick Swanson _______ 25 COACHES & STAFF Steve Bieser _____________________ 26-27 Lance Rhodes / Fred Corral _____________ 28 Jake Epstein / Jae Fadde ______________ 29 Austin Tribby / Brett Peel ______________ 30 Support Staff _______________________ 31 2018 SEASON IN REVIEW Season Stats _______________________ 32 SEC Only Stats ______________________ 33 Results Summary ____________________ 34 Miscellaneous Stats __________________ 35 PROGRAM -

Aaron Daniel Gray, MD Associate Professor E-Mail
Aaron Daniel Gray, M.D. Associate Professor E-mail: [email protected] Department of Orthopaedics Twitter: @MizzouSportsDoc Department of Family Medicine University of Missouri Department of Orthopaedics 1100 Virginia Ave. Columbia, MO 65212 Employment 2011 - present Family Physician & Sports Medicine Physician Assistant Professor Department of Family Medicine Department of Orthopaedics / Division of Sports Medicine University of Missouri School of Medicine Education & Training 2010-2011 Fellow, Primary Care Sports Medicine Department of Family Medicine / Division of Sports Medicine University of California – Los Angeles 2007-2010 Resident Physician (Chief Resident 2009-2010) Department of Family and Community Medicine University of Missouri, Columbia, MO 2003-2007 University of Tennessee - Health Science Center College of Medicine, Memphis, TN M.D. 1999-2003 Tennessee Technological University, Cookeville, TN B.S., Summa cum laude, 4.0 GPA, Chemistry Honors 2012 “Teacher of the Year.” Family Medicine Residency Program, Department of Family Medicine, University of Missouri. Team Physician Experience United States Soccer Federation 2014 Team Physician – Boys U-15 National Team Training Camp Abu Dhabi, United Arab Emirates Team Physician – U-23 United States Men’s National Team Brasilia, Brazil University of Missouri 2012-Present Team Physician – Baseball (2012-2015), Volleyball (2014) Physician – Athletic Department Pre-participation Physicals Training Room Physician – All Athletic Teams Integrated Healthcare Team – Medical Director (2015 -

University of Missouri Campus
ACADEMIC UNITS 1931 when the Chinese government gave them to the School of Journalism. Today, as the story goes, if students break the silence of the archway while Accountancy, School of, 303 Cornell 882-4463 University of Missouri passing through, they will fail their next exam. Agriculture, Food and Natural Resources, College of, 2-64 Agriculture, 882- 8301 6. Thomas Jefferson Statue and Tombstone: Founded in 1839, Mizzou is Campus Map Arts and Science, College of, 317 Lowry, 882-4421 the first public land-grant institution west of the Mississippi River, an outcome Business, Trulaske College of, 111 Cornell , 882-7073 of Thomas Jefferson’s dedication to expanding the United States and his Education, College of, 109 Hill, 882-0560 commitment to public education. Jefferson also is the father of the University Engineering, College of, W1025 Laferre, 882-4375 of Virginia, MU’s sister school and the model for Francis Quadrangle. Jef- Graduate School, 210 Jesse, 882-6311 ferson’s gravemarker was donated to MU by his grandchildren. In 2001, a Welcome Health Professions, School of, 504 Lewis 882-8011 statue of Thomas Jefferson, created by Colorado sculptor George Lundeen, to the University was dedicated as a gift from the trustees of the Jefferson Club. Human Environmental Sciences, College of, 117 Gwynn, 882-6424 of Missouri. As a Journalism, School of, 120 Neff, 882-4821 7. The Residence on Francis Quadrangle: Built in 1867, this house is the Columbia area 763 Law, School of, 203 Hulston, 882-6487 oldest building on campus and has been home to 18 university presidents land-grant institution Informational Science and Learning Technology, School of, 303 Townsend, and chancellors. -
2016 Front.Indd
2016 INTRODUCTION Allie Hess ............................................21 MIZZOU HISTORY Media Information .................................2 Jessica Johnson .................................22 2014 in Review ..............................48-49 Quick Facts ...........................................3 Savannah Trujillo ................................23 Career Records .............................50-51 Schedule ............................................... 4 Lauren Gaston ....................................24 Season Records ............................52-53 Bethany Coons ...................................25 Team Records ...............................54-55 COACHING STAFF Kelsey Dossey ....................................26 Year-by-Year Leaders ....................56-57 Bryan Blitz .........................................6-7 Rachel Hise ........................................27 Individual Honors ...........................58-61 Don Trentham / Molly Schneider ..........8 Natalie McDonough ............................38 All-Time Letterwinners ........................62 Support Staff ....................................9-10 Amanda Shaw ....................................29 All-Time Roster ...................................63 Payton Goulding / Erin Jones .............30 NCAA History .................................64-67 2016 TIGERS Madison Lewis / Izzy Coulter ..............31 Program History .............................68-77 2016 Tigers .........................................12 Anna Frick / Peyton Joseph ................32 Year-by-Year -

Missourialumnus.Pdf (12.66Mb)
/} ISSOURI VOL. XXXIX -· No. 3 UNIVERSITY ol MISSOURI NOVEMBER, 1950 HOMECOMING-November 20-23 IT WAS MORE THAN JUST CHANCE THAT THERE WAS A M& VOICI.S on the sound~tmck fnded down and T died. While the people on the 'Cr«n moved their lips in ai!cncc, a m:m•s deep voice cut in nnd nskcd, .. h there a doctort in he the<'ttrd rr there is. will he plentc come to the manager'a offitc risht ll wtty~ " A tnll young mo\n arose in tl1e $Cmi -dArknc:s..~ of the thentrc nnd bqvm cdgins- his way townrd the :ai11le. Batt l:'is.her watched him go UJ'I the aisle with lo11g, swift atridcs. His wife leaned coward him and whis pued, '"Wasn't that youngAifrM Buna~~·· Da" noddtd. ''Probably his fine movie in months.•• The voices eame back to the SC'ttn and the audience: ruttled for a moment and then scni«l back to listen. lt wu a~ movie, but now O;m's mind w.as w~tndering f:u from t he screen. He was thinking of Alfred Barnes-and wondcrina, as no doubt others in the nudience were-what emergency hnd called him to the bnck of the theatre. A hcllrt nttnck . .. 1t fnincina sp-ell ... :tn nccidenc . .. these thing.!! hAppen. 1t w11s fortunA.te th:tt young Bnrnes WAI there , . And yet it was something more than "fortune" that h.Ad Jet the boy re:~li"tt hi• ambitions tO be a phyaidan in the first place. Bart smiled t·o himJCJ( u he rcnlled how seriously the lad had tpoken of his ••career in medicine. -

Together for '21 Fest: a Missouri Bicentennial Birthday Bash
TOGETHER FOR ’21 FEST: A MISSOURI BICENTENNIAL BIRTHDAY BASH August 6-8, 2021 Together for ’21 Fest is an event of the Missouri Bicentennial Commission, organized by The State Historical Society of Missouri and The University of Missouri. Statehood Day events are sponsored by Shelter Insurance and Union Pacific Railroad. Preliminary Schedule of Events Friday, August 6 8:00 a.m. – 4:00 p.m. Quilt exhibition – Cook Hall, Center for Missouri Studies Since the pioneer days of the American Midwest, quilts have been a cornerstone of Missouri culture, fashion, and tradition. The quilt exhibition will feature quilts made across the state in honor of the bicentennial year. The following quilts will be on display: • Missouri Bicentennial Quilt by SHSMO/Missouri Star Quilt Co. • Missouri 4-H Bicentennial Quilt by Missouri 4-H • Phelps County Bicentennial Quilt by Phelps County Quilting Group • Texas County Bicentennial Quilt by Houston Community Betterment • Ray County Bicentennial Quilt by Ray County Committee My Missouri 2021 exhibition – Hulston Lobby, Center for Missouri Studies 2 Between May 2018 and November 2019, Missouri 2021 invited professional and amateur photographers to capture unique and meaningful aspects of Missouri. The exhibition, oriented around the four seasons, features selected images from this project and reflects the geographic and cultural landscape of the state. Bicentennial Time Capsule – Hulston Lobby, Center for Missouri Studies Come add your “note to future Missourians” to the Bicentennial Time Capsule! Bicentennial poster exhibition – Mezzanine, Center for Missouri Studies In 2020, Missouri students helped the Missouri Bicentennial Commission commemorate the state’s 200th anniversary by submitting design concepts for a Missouri Bicentennial poster. -

Evaluating Convergence Students’ Preparation at the University of Missouri School of Journalism
IS J-SCHOOL WORTH IT? EVALUATING CONVERGENCE STUDENTS’ PREPARATION AT THE UNIVERSITY OF MISSOURI SCHOOL OF JOURNALISM SARAH TUCKER Missouri School of Journalism MAY 2014 Committee: Clyde Bentley, chair Yong Volz Tom Warhover ii ACKNOWLEDGEMENTS Many thanks to Clyde Bentley, my project committee chair, for his patience, encouragement on crafting and completing this project. Special thanks to my other committee members, Yong Volz and Tom Warhover, for their input and guidance on this project. And finally, many thanks to the Mizzou Mafia. Your offers to help a fellow Tiger were encouraging. And for those alumni who participated, thank you for your time and giving me hope when I needed it. I always found our conversations inspiring. TABLE OF CONTENTS ACKNOWLEDGEMENTS .......................................................................................................................... ii Chapter 1. INTRODUCTION ........................................................................................................................... 1 2. FIELD NOTES ................................................................................................................................. 8 3. SELF-EVALUATION .................................................................................................................. 44 4. PROFESSIONAL WORK .......................................................................................................... 48 5. SCHOLARLY ANALYSIS ....................................................................................................... -

University of Missouri Campus
ACADEMIC UNITS SCHOOL OF JOURNALISM* (35, 9) Mizzou is home to the oldest journalism school Accountancy, School of, 303 Cornell 882-4463 in the world. It was established in 1908 by Walter Williams and is always ranked among the Agriculture, Food and Natural Resources, College of, 2-64 Agriculture, 882- best programs in the country. The Donald W. Reynolds Journalism Institute’s industry leading University of Missouri 8301 resources demonstrate new technologies advancing news production, design and delivery, information and advertising. Features include a technology and research center, the Futures Arts and Science, College of, 317 Lowry, 882-4421 Laboratory and Demonstration Center, an enlarged journalism library, administrative offices, Campus Map Business, Trulaske College of, 111 Cornell , 882-7073 fellows and graduate-studies programs and seminar space. Education, College of, 109 Hill, 882-0560 JOURNALISM ARCHWAY* (169, 10) The two stone lions that stand in the archway Engineering, College of, W1025 Laferre, 882-4375 between Neff and Walter Williams halls once guarded a Confucian temple in China. Dating from the Ming Dynasty, circa 1400, the lions became a fixture on campus in 1931 when the Chinese Graduate School, 210 Jesse, 882-6311 government gave them to the School of Journalism. Today, as the story goes, if students break Health Professions, School of, 504 Lewis 882-8011 the silence of the archway while passing through, they will fail their next exam. Welcome Human Environmental Sciences, College of, 117 Gwynn, 882-6424 MUSEUM OF ART AND ARCHAEOLOGY* (93, 11) Pickard Hall houses mid- to the University Journalism, School of, 120 Neff, 882-4821 Missouri’s largest art museum. -
Gov Bd Manual-Final Indd.Indd
Governing Board Resource Guide 2008-2009 ThankThank YouYou To our Association Leadership, Since 1853, the Mizzou Alumni Association has carried the torch of alumni support for the University of Missouri. From our fi rst president, Gen. Odon Guitar, until today we have been blessed with extraordinary volunteer leadership. Thanks in large part to that leadership, the Association has been a proud and prominent resource for the University and its alumni for 155 years. This resource guide is the product of our commitment to communicate effi ciently and effectively with our volunteer leaders. We are hopeful the enclosed information is a useful tool for you as you serve on our Governing Board. It is critical that you know and share the story of how the Association proudly serves the best interests and traditions of Missouri’s fl agship university. We are proud to serve a worldwide network of 250,000 Mizzou alumni. Your volunteer leadership represents a portion of our diverse, vibrant and loyal membership base. While Mizzou has many cherished traditions, the tradition of alumni support is one that we foster by our actions and commitment to the Asso- ciation and the University. Thank you for your selfl ess service to MU and the Association. With your involvement and engage- ment, I am confi dent we will reach our vision of becoming the preeminent resource for the University of Missouri. Our staff and I look forward to working with you in 2008 - 2009. Go Mizzou! Todd A. McCubbin, M Ed ‘95 Executive Director Mizzou Alumni Association Table of Contents