Lymphatic Filariasis Epidemiology in Samoa in 2018: Geographic Clustering and Higher Antigen Prevalence in Older Age Groups
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
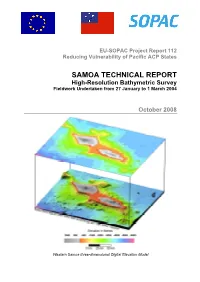
High-Resolution Bathymetric Survey of Samoa
EU-SOPAC Project Report 112 Reducing Vulnerability of Pacific ACP States SAMOA TECHNICAL REPORT High-Resolution Bathymetric Survey Fieldwork Undertaken from 27 January to 1 March 2004 October 2008 Western Samoa three-dimensional Digital Elevation Model Prepared by: Jens Krüger and Salesh Kumar SOPAC Secretariat May 2008 PACIFIC ISLANDS APPLIED GEOSCIENCE COMMISSION c/o SOPAC Secretariat Private Mail Bag GPO, Suva FIJI ISLANDS http://www.sopac.org Phone: +679 338 1377 Fax: +679 337 0040 www.sopac.org [email protected] Important Notice This report has been produced with the financial assistance of the European Community; however, the views expressed herein must never be taken to reflect the official opinion of the European Community. Samoa: High-Resolution Bathymetry EU EDF-SOPAC Reducing Vulnerability of Pacific ACP States – iii TABLE OF CONTENTS EXECUTIVE SUMMARY ......................................................................................................... 1 1. INTRODUCTION ........................................................................................................ 2 1.1 Background ................................................................................................................ 2 1.2 Geographic Situation .................................................................................................. 2 1.3 Geological Setting ...................................................................................................... 3 1.4 Previous Bathymetry Compilations............................................................................ -

Samoa Socio-Economic Atlas 2011
SAMOA SOCIO-ECONOMIC ATLAS 2011 Copyright (c) Samoa Bureau of Statistics (SBS) 2011 CONTACTS Telephone: (685) 62000/21373 Samoa Socio Economic ATLAS 2011 Facsimile: (685) 24675 Email: [email protected] by Website: www.sbs.gov.ws Postal Address: Samoa Bureau of Statistics The Census-Surveys and Demography Division of Samoa Bureau of Statistics (SBS) PO BOX 1151 Apia Samoa National University of Samoa Library CIP entry Samoa socio economic ATLAS 2011 / by The Census-Surveys and Demography Division of Samoa Bureau of Statistics (SBS). -- Apia, Samoa : Samoa Bureau of Statistics, Government of Samoa, 2011. 76 p. : ill. ; 29 cm. Disclaimer: This publication is a product of the Division of Census-Surveys & Demography, ISBN 978 982 9003 66 9 Samoa Bureau of Statistics. The findings, interpretations, and conclusions 1. Census districts – Samoa – maps. 2. Election districts – Samoa – expressed in this volume do not necessarily reflect the views of any funding or census. 3. Election districts – Samoa – statistics. 4. Samoa – census. technical agencies involved in the census. The boundaries and other information I. Census-Surveys and Demography Division of SBS. shown on the maps are only imaginary census boundaries but do not imply any legal status of traditional village and district boundaries. Sam 912.9614 Sam DDC 22. Published by The Samoa Bureau of Statistics, Govt. of Samoa, Apia, Samoa, 2015. Overview Map SAMOA 1 Table of Contents Map 3.4: Tertiary level qualification (Post-secondary certificate, diploma, Overview Map ................................................................................................... 1 degree/higher) by district, 2011 ................................................................... 26 Introduction ...................................................................................................... 3 Map 3.5: Population 15 years and over with knowledge in traditional tattooing by district, 2011 ........................................................................... -

'IMPRESS Project' And
“To improve the sustainable and costs-effective utilization of indigenous renewable energy resources for energy production in Samoa” The Ministry of Natural Resources and Environment through a collaboration between the ‘IMPRESS Project’ and the ‘2 Million Tree Planting Campaign’ under the Forestry Division; will be conducting a Tree Planting Event on Friday 14th June 2019. It is part of a three (4) days tree planting campaign starting from 12th June (refer to program attached). A tree has various components that are valuable to our communities and the environment. Apart from the ecological services in which it provides, a tree is also considered a source of Renewable Energy as it can produce Electricity. But how? The IMPRESS Project is constructing the very first ever Biomass Gasification Plant at Afolau. It is a technology of its kind which converts stored potential energy contained in trees to electric energy; making Biomass Energy the fifth (5th) source of Renewable Energy available in Samoa. This Gasification plant will assist our electricity sector in meeting its current target goal and Nationally Determinded Contributions (NDC) of “100% Renewable Energy target for Electricity generation by 2025.” By harvesting only invasive species that are available at certain plots of Afolau. The purpose of the Tree Planting event on 14th June is to showcase the various importance of trees and to offset harvest operations which will take place in Afolau. The Tree Planting event will take place at Faleolo Reserve (refer to diagrams attached). Registrations of all participants will start at 9am (refer to program attached). An estimate of 75 students altogether from five (5) Schools will be participating in this event. -

2016 CENSUS Brief No.1
P O BOX 1151 TELEPHONE: (685)62000/21373 LEVEL 1 & 2 FMFM II, Matagialalua FAX No: (685)24675 GOVERNMENT BUILDING Email: [email protected] APIA Website: www.sbs.gov.ws SAMOA 2016 CENSUS Brief No.1 Revised version Population Snapshot and Household Highlights 30th October 2017 1 | P a g e Foreword This publication is the first of a series of Census 2016 Brief reports to be published from the dataset version 1, of the Population and Housing Census, 2016. It provides a snapshot of the information collected from the Population Questionnaire and some highlights of the Housing Questionnaire. It also provides the final count of the population of Samoa in November 7th 2016 by statistical regions, political districts and villages. Over the past censuses, the Samoa Bureau of Statistics has compiled a standard analytical report that users and mainly students find it complex and too technical for their purposes. We have changed our approach in the 2016 census by compiling smaller reports (Census Brief reports) to be released on a quarterly basis with emphasis on different areas of Samoa’s development as well as demands from users. In doing that, we look forward to working more collaboratively with our stakeholders and technical partners in compiling relevant, focused and more user friendly statistical brief reports for planning, policy-making and program interventions. At the same time, the Bureau is giving the public the opportunity to select their own data of interest from the census database for printing rather than the Bureau printing numerous tabulations which mostly remain unused. -

Samoa 2015 Education Stats
2015 Introduction The Statistical Digest provides a range of statistics and performance measures related to education in Samoa. The information included in the digest is the latest information available as of June 2014. Historical data has also been included to reflect changes over time. The Digest is divided into two parts: Part 1 – Data from School Census Information System and Early Childhood Education (ECE) Monitoring Visits Part 2 – Data from sources other than the School Census Information System Part 1 Data from School Census Information System The Annual School Census data collection, held on the first week of March, is a major source of statistical information. The census data is stored in the Ministry’s school census information system called Manumea. The school census information system includes a series of reports, which are automatically produced. These reports are contained in Part 1 of the Statistical Digest. Data for Early Childhood Education (ECE) is collected from monitoring visits conducted by the Ministry. This information is stored separately. Part 2 Data from sources other than the School Census Information System The Ministry of Education, Sports and Culture’s performance measure framework includes a range of indicators provided by the Assessment and Examination Unit. Data has been collected from a range of sources such as examination results and personnel information. This information is contained in Part 2 of the Statistical Digest. Statistical Digest produced by: Policy, Planning and Research Division Ministry of Education Sports & Culture Samoa Phone: (+685) 64601 Fax: (+685) 64664 Email:[email protected] July 2015 BRIEF OVERVIEW OF SAMOA’S EDUCATION SYSTEM Primary and Secondary education in Samoa is provided through three stakeholders, namely the Government in partnership with village based school committees, mission schools and private schools. -

MH-ICP-MS Analysis of the Freshwater and Saltwater Environmental Resources of Upolu Island, Samoa
Supplementary Materials (SM) MH-ICP-MS Analysis of the Freshwater and Saltwater Environmental Resources of Upolu Island, Samoa Sasan Rabieh 1,*, Odmaa Bayaraa 2, Emarosa Romeo 3, Patila Amosa 4, Khemet Calnek 1, Youssef Idaghdour 2, Michael A. Ochsenkühn 5, Shady A. Amin 5, Gary Goldstein 6 and Timothy G. Bromage 1,7,* 1 Department of Molecular Pathobiology, New York University College of Dentistry, 345 East 24th Street, New York, NY 10010, USA; [email protected] (K.C.) 2 Environmental Genomics Lab, Biology Program, Division of Science and Mathematics, New York University Abu Dhabi, Saadiyat Island, PO Box 129188, Abu Dhabi, United Arab Emirates; [email protected] (O.B.); [email protected] (Y.I.) 3 Hydrology Division, Ministry of Natural Resources and Environment, Level 3, Tui Atua Tupua Tamasese Efi Building (TATTE), Sogi., P.O. Private Bag, Apia, Samoa; [email protected] (E.R.) 4 Faculty of Science, National University of Samoa, PO Box 1622, Apia, Samoa; [email protected] (P.A.) 5 Marine Microbial Ecology Lab, Biology Program, New York University Abu Dhabi, Saadiyat Island, PO Box 129188, Abu Dhabi, United Arab Emirates; [email protected] (M.A.O.); [email protected] (S.A.A.) 6 College of Dentistry, New York University, 345 East 24th Street, New York, NY 10010, USA; [email protected] (G.G.) 7 Department of Biomaterials, New York University College of Dentistry, 345 East 24th Street, New York, NY 10010, USA * Correspondence: [email protected] (S.R.); [email protected] (T.G.B.); Tel.: +1-212-998-9638 (S.R.); +1- 212-998-9597 (T.G.B.) Academic Editors: Zikri Arslan and Michael Bolshov Received: 16 August 2020; Accepted: 19 October 2020; Published: date Table S1. -

Samatau Reserve Reassessment
Project Title: Strengthen the Management and Monitoring of Samoa’s Community- Based Marine Management and MPAs Network Grantee Name: Government of Samoa Ministry of Agriculture and Fisheries Award Number: NA11NOS4820010 Award Period: 10/01/2011 - 06/30/2013 FINAL REPORT 0 Contents Progress Report………………………………………………………………………………….……page 2 Appendix 1: 2 Samoa’s General Meeting Nov. 2011……………………………………page 9 Appendix 2: Two Samoa’s Strategic Plan – unsigned……………………………..….page 15 Appendix 3a: Communities Exchange Agenda………………………………..…………page 28 Appendix 3b: Cabinet Report (Samoan)……………………………………………………page 31 Appendix 4: Community-based Fisheries Management Program Poster…….page 34 Appendix 4: Live Coral Poster……………………………………………………………….….page 34 Appendix 5: Pictures of Floats and Signboards……………………………………….….page 35 Appendix 6: Ecological Assessments conducted at data less sites………….……page 38 1 A. Background 1. The project was identified as an important boost to the onward movement of the 2 Samoas Environmental Initiative. The Ministry of Agriculture and Fisheries (MAF) and the Ministry of Environment and Natural Resources (MNRE) who are the main counterparts in the Samoan Government developed this proposal as an initial implementation on some of the needed activities in which Samoa needs to be effective in the collaboration with American Samoa. 2. The project proposal targeted the NOAAs Coral Reef Conservation Grant Program Fiscal Year 2011 Federal Funding Opportunity–International Coral Reef Conservation Cooperative Agreements with relative Objective -

Geological Subsidence and Sinking Islands: The
1 Symposium for W. Dickinson – SAA 2015 “Geological subsidence and sinking Islands: the case of Manono (Samoa)” Christophe Sand1, Jacques Bolé1, David Baret1, André-John Ouetcho1, Fiona Petchey2, Alan Hogg2 Tautala Asaua3 Abstract W. Dickinson, as part of his wide study of the geological history of the Pacific islands, has proposed in a series of papers to explainlinked the unique case of the deeply submerged Lapita site of Mulifanua in Western Upolu (Samoa), as linked to the slow subsidence of Upolu Island. Recent archaeological research on the neighbouring small island of Manono, has brought new and detailed data on this geological process. A series of new dates has allowed us to define chronologically the speed of the subsidence and demonstrateas well as the massive environmental changes that the local population had to adapt to over the past 2500 years. 1. Institute of Archaeology of New Caledonia and the Pacific (IANCP) 2. Radiocarbon Dating Laboratory, University of Waikato 3. Center for Samoan Studies, National University of Samoa 2 Introduction The geological diversity of the Pacific region defies any simple categorization. The region is, divided between different tectonic plates and, cut in two on its western side by the active “belt of fire”, with iIslands ranking being derived from continental fragments to old eroding or still active volcanic summits to simple coral aAtolls, defies any simple categorization. Volcanic activity, earthquakes and possible tsunami-related events, associated to episodes of extreme weather devastation through cyclones/typhoons or prolonged droughts make Oceania a region that often defies the idyllic image built by Western imagination. -

Climate of Samoa
DaDatata CCoollecllectiotionn aanndd mmodeodellillinnggffoor ar adadaptaptationtion Nusipepa Lepale Samoa Presentation OutlinePresentation Outline Background info Geography Climate of Samoa Impacts of Climate Change (CC) in Samoa CC Adaptation in Samoa Data Observation Network (Data collection) Modeling used in Samoa Responses to Climate Change in Samoa Samoa Climate Early Warning System (CLEWS) Background InformationBackground Information Samoa, officially the Independent State of Samoa (formerly known as Western Samoa and German Samoa), is a country governing the western part of the Samoan Islands in the South Pacific Ocean. It became independent from New Zealand in 1962. The two main islands of Samoa are Upolu and one of the biggest islands in Polynesia Savai'i. The capital city Apia and Faleolo International Airport are situated on the island of Upolu. The 1960 Constitution, which formally came into force with independence from New Zealand in 1962, is based on the British pattern of parliamentary democracy, modified to take account of Samoan customs The unicameral legislature (Fono) consists of 49 members serving 5-year terms. Forty-seven are elected from territorial districts by ethnic Samoans; the other two are chosen by non-Samoans with no chiefly affiliation on separate electoral rolls GeographyGeography The country is located east of the international date line and south of the equator, about halfway between Hawai‘i and New Zealand in the Polynesian region of the Pacific Ocean. The total land area is 2934 km² -

Report on the Distribution of the Introduced Seaweeds
Report on the distribution of the introduced seaweeds (Codium arenicola and Spatoglossum macrodontum) and the distribution and density of the crown of thorn starfish (Acanthaster planci) 18 – 19 October 2014 Prepared by: Marine Conservation Section Division of Environment & Conservation Ministry of Natural Resources & Environment 1 1. INTRODUCTION A survey conducted in 2008 identified two introduced seaweed species that do not occur naturally in the marine environment of Samoa. These were the Codium arenicola which is found in Thailand and Southeast Asia and the Spatoglossum macrodontum,a brown algae recorded from French Polynesia, Hawaii and Australia. The two seaweeds were observed distributed and well established around the Apia harbour, Mulinuu and Palolo deep marine reserve. The crown of thorn starfish (COTS) are coral-eating starfish that occur throughout the Indo- Pacific region (Wilmes, 2014). They are naturally found on coral reefs where they can be observed in low numbers. An outbreak of the COTS was observed in a number of villages after the 2009 tsunami.The Fisheries Division of the Ministry of Agriculture and Fisheries and the MNRE worked with the communities to collect the starfish mainly from the areas along the southern and south-eastern coast of Upolu Island. This activity was an effort to help with the recovery of coral reefs from the impacts of the tsunami. However, there were a number of reports from various villages on both Upolu, Savaii and Manono Islands reporting large numbers of crown of thorn starfish (COT) in their marine environment and concerns that the increase in the number of COTs were impacting the health of the corals. -

The Rare Plants of Samoa JANUARY 2011
The Rare Plants of Samoa JANUARY 2011 BIODIVERSITY CONSERVATION LESSONS LEARNED TECHNICAL SERIES 2 BIODIVERSITY CONSERVATION LESSONS LEARNED TECHNICAL SERIES 2 The Rare Plants of Samoa Biodiversity Conservation Lessons Learned Technical Series is published by: Critical Ecosystem Partnership Fund (CEPF) and Conservation International Pacific Islands Program (CI-Pacific) PO Box 2035, Apia, Samoa T: + 685 21593 E: [email protected] W: www.conservation.org Conservation International Pacific Islands Program. 2011. Biodiversity Conservation Lessons Learned Technical Series 2: The Rare Plants of Samoa. Conservation International, Apia, Samoa Author: Art Whistler, Isle Botanica, Honolulu, Hawai’i Design/Production: Joanne Aitken, The Little Design Company, www.thelittledesigncompany.com Series Editors: James Atherton and Leilani Duffy, Conservation International Pacific Islands Program Conservation International is a private, non-profit organization exempt from federal income tax under section 501c(3) of the Internal Revenue Code. ISBN 978-982-9130-02-0 © 2011 Conservation International All rights reserved. OUR MISSION Building upon a strong foundation of science, partnership and field demonstration, CI empowers societies to responsibly and sustainably care for nature for the well-being of humanity This publication is available electronically from Conservation International’s website: www.conservation.org ABOUT THE BIODIVERSITY CONSERVATION LESSONS LEARNED TECHNICAL SERIES This document is part of a technical report series on conservation projects funded by the Critical Ecosystem Partnership Fund (CEPF) and the Conservation International Pacific Islands Program (CI-Pacific). The main purpose of this series is to disseminate project findings and successes to a broader audience of conservation professionals in the Pacific, along with interested members of the public and students. -

The Case of Samoa
GeoHazards Article Multiscale Quantification of Tsunami Hazard Exposure in a Pacific Small Island Developing State: The Case of Samoa Shaun Williams 1,* , Ryan Paulik 1 , Rebecca Weaving 2,3, Cyprien Bosserelle 1 , Josephina Chan Ting 4, Kieron Wall 1 , Titimanu Simi 5 and Finn Scheele 6 1 National Institute of Water and Atmospheric Research (NIWA), Christchurch 8011, New Zealand; [email protected] (R.P.); [email protected] (C.B.); [email protected] (K.W.) 2 School of Geography, Environment and Geosciences, University of Portsmouth, Portsmouth, Hampshire PO1 2UP, UK; [email protected] 3 Ascot Underwriting Ltd., London EC3M 3BY, UK 4 Disaster Management Office, Ministry of Natural Resources and Environment, Apia WS1339, Western Samoa; [email protected] 5 Project Unit, Samoa Green Climate Fund Project, Ministry of Finance, Apia WS1339, Western Samoa; [email protected] 6 GNS Science, Lower Hutt 5011, New Zealand; [email protected] * Correspondence: [email protected] Abstract: This study presents a scenario-based approach for identifying and comparing tsunami exposure across different sociopolitical scales. In Samoa, a country with a high threat to local tsunamis, we apply scenarios for the 2009 South Pacific tsunami inundation at different grid resolutions (50 and 10 m) to quantify building and road exposure at the national, district and village levels. We Citation: Williams, S.; Paulik, R.; show that while the coarser 50 m model is adequate for use in the rapid identification of exposure Weaving, R.; Bosserelle, C.; Chan at the national and district levels, it can overestimate exposure by up to three times more at the Ting, J.; Wall, K.; Simi, T.; Scheele, F.