The Role of Succinate and ROS in Reperfusion Injury – a Critical Appraisal
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Progressive Increase in Mtdna 3243A>G Heteroplasmy Causes Abrupt
Progressive increase in mtDNA 3243A>G PNAS PLUS heteroplasmy causes abrupt transcriptional reprogramming Martin Picarda, Jiangwen Zhangb, Saege Hancockc, Olga Derbenevaa, Ryan Golhard, Pawel Golike, Sean O’Hearnf, Shawn Levyg, Prasanth Potluria, Maria Lvovaa, Antonio Davilaa, Chun Shi Lina, Juan Carlos Perinh, Eric F. Rappaporth, Hakon Hakonarsonc, Ian A. Trouncei, Vincent Procaccioj, and Douglas C. Wallacea,1 aCenter for Mitochondrial and Epigenomic Medicine, Children’s Hospital of Philadelphia and the Department of Pathology and Laboratory Medicine, University of Pennsylvania, Philadelphia, PA 19104; bSchool of Biological Sciences, The University of Hong Kong, Hong Kong, People’s Republic of China; cTrovagene, San Diego, CA 92130; dCenter for Applied Genomics, Division of Genetics, Department of Pediatrics, and hNucleic Acid/Protein Research Core Facility, Children’s Hospital of Philadelphia, Philadelphia, PA 19104; eInstitute of Genetics and Biotechnology, Warsaw University, 00-927, Warsaw, Poland; fMorton Mower Central Research Laboratory, Sinai Hospital of Baltimore, Baltimore, MD 21215; gGenomics Sevices Laboratory, HudsonAlpha Institute for Biotechnology, Huntsville, AL 35806; iCentre for Eye Research Australia, Royal Victorian Eye and Ear Hospital, East Melbourne, VIC 3002, Australia; and jDepartment of Biochemistry and Genetics, National Center for Neurodegenerative and Mitochondrial Diseases, Centre Hospitalier Universitaire d’Angers, 49933 Angers, France Contributed by Douglas C. Wallace, August 1, 2014 (sent for review May -
Pharmacological Inhibition of Tumor Anabolism and Host Catabolism As A
www.nature.com/scientificreports OPEN Pharmacological inhibition of tumor anabolism and host catabolism as a cancer therapy Alejandro Schcolnik‑Cabrera1,2, Alma Chavez‑Blanco1, Guadalupe Dominguez‑Gomez1, Mandy Juarez1, Ariana Vargas‑Castillo3, Rafael Isaac Ponce‑Toledo4, Donna Lai5, Sheng Hua5, Armando R. Tovar3, Nimbe Torres3, Delia Perez‑Montiel6, Jose Diaz‑Chavez1 & Alfonso Duenas‑Gonzalez1,7* The malignant energetic demands are satisfed through glycolysis, glutaminolysis and de novo synthesis of fatty acids, while the host curses with a state of catabolism and systemic infammation. The concurrent inhibition of both, tumor anabolism and host catabolism, and their efect upon tumor growth and whole animal metabolism, have not been evaluated. We aimed to evaluate in colon cancer cells a combination of six agents directed to block the tumor anabolism (orlistat + lonidamine + DON) and the host catabolism (growth hormone + insulin + indomethacin). Treatment reduced cellular viability, clonogenic capacity and cell cycle progression. These efects were associated with decreased glycolysis and oxidative phosphorylation, leading to a quiescent energetic phenotype, and with an aberrant transcriptomic landscape showing dysregulation in multiple metabolic pathways. The in vivo evaluation revealed a signifcant tumor volume inhibition, without damage to normal tissues. The six‑drug combination preserved lean tissue and decreased fat loss, while the energy expenditure got decreased. Finally, a reduction in gene expression associated with thermogenesis was observed. Our fndings demonstrate that the simultaneous use of this six‑drug combination has anticancer efects by inducing a quiescent energetic phenotype of cultured cancer cells. Besides, the treatment is well‑ tolerated in mice and reduces whole animal energetic expenditure and fat loss. -

Robert Shine, Peter Dwyer, Lyndsay Olson, Jennifer Truong, Matthew Goddeeris, Effie Tozzo, Eric Bell Mitobridge, Inc
Poster Title Here Mitochondrial Deficiency in Primary Muscle Cells from Mdx Mice Robert Shine, Peter Dwyer, Lyndsay Olson, Jennifer Truong, Matthew Goddeeris, Effie Tozzo, Eric Bell Mitobridge, Inc. Cambridge, MA 02138 Abstract Results Results Duchenne muscular dystrophy (DMD) is a recessive, fatal X-linked disease that is characterized M ito c h o n d ria l c o n trib u te d A T P is re d u c e d Mdx myoblasts have decreased expression by progressive skeletal muscle wasting due to a loss of function in dystrophin, a protein that is of OXPHOS complexes part of a complex that bridges the cytoskeleton and extracellular matrix. The mdx mouse, an in m d x m y o b la s ts a n d m y o tu b e s T animal model for DMD, has a point mutation in the dystrophin gene that results in a loss of 1 .5 2.0 W l function. This study uses primary muscle satellite cell derived myoblasts and myotubes to W T a WT m determine differences in mitochondrial biology between the mdx mice and wild type (WT) control s M D X o 1.5 a r MDX mice. Compared to cells isolated from WT mice, mdx cells have reductions in mitochondrial 1 .0 **** f B bioenergetics. Moreover, mdx cells have reduced levels of mitochondria which may partially *** e T g 1.0 explain the reduction in bioenergetics. Interestingly, the mitochondrial phenotype is apparent **** ** n * * W a * * * before dystrophin protein is increased during myogenesis. * * * 0 .5 h 0.5 * d l C o d l F 0.0 o 1 3 2 6 1 a 1 a b B 0 .0 F t v Materials and Analysis a 5 P X D C H H y 5 l l F X T N R O D a M in a M in D C s s P n n U A c c O S C C a 0 a 0 S y y T B 0 B 0 D WT and mdx myoblast isolation and culture: Quadricep and gastrocnemius muscles from a C 1 m 1 m Q A o o N single mouse were pooled and subjected to a mechanical/collagenase digestion. -

Understanding the Central Role of Citrate in the Metabolism of Cancer Cells and Tumors: an Update
International Journal of Molecular Sciences Review Understanding the Central Role of Citrate in the Metabolism of Cancer Cells and Tumors: An Update Philippe Icard 1,2,3,*, Antoine Coquerel 1,4, Zherui Wu 5 , Joseph Gligorov 6, David Fuks 7, Ludovic Fournel 3,8, Hubert Lincet 9,10 and Luca Simula 11 1 Medical School, Université Caen Normandie, CHU de Caen, 14000 Caen, France; [email protected] 2 UNICAEN, INSERM U1086 Interdisciplinary Research Unit for Cancer Prevention and Treatment, Normandie Université, 14000 Caen, France 3 Service de Chirurgie Thoracique, Hôpital Cochin, Hôpitaux Universitaires Paris Centre, APHP, Paris-Descartes University, 75014 Paris, France; [email protected] 4 INSERM U1075, COMETE Mobilités: Attention, Orientation, Chronobiologie, Université Caen, 14000 Caen, France 5 School of Medicine, Shenzhen University, Shenzhen 518000, China; [email protected] 6 Oncology Department, Tenon Hospital, Pierre et Marie Curie University, 75020 Paris, France; [email protected] 7 Service de Chirurgie Digestive et Hépato-Biliaire, Hôpital Cochin, Hôpitaux Universitaires Paris Centre, APHP, Paris-Descartes University, 75014 Paris, France; [email protected] 8 Descartes Faculty of Medicine, University of Paris, Paris Center, 75006 Paris, France 9 INSERM U1052, CNRS UMR5286, Cancer Research Center of Lyon (CRCL), 69008 Lyon, France; [email protected] 10 ISPB, Faculté de Pharmacie, Université Lyon 1, 69373 Lyon, France 11 Department of Infection, Immunity and Inflammation, Institut Cochin, INSERM U1016, CNRS UMR8104, Citation: Icard, P.; Coquerel, A.; Wu, University of Paris, 75014 Paris, France; [email protected] Z.; Gligorov, J.; Fuks, D.; Fournel, L.; * Correspondence: [email protected] Lincet, H.; Simula, L. -

PIM2-Mediated Phosphorylation of Hexokinase 2 Is Critical for Tumor Growth and Paclitaxel Resistance in Breast Cancer
Oncogene (2018) 37:5997–6009 https://doi.org/10.1038/s41388-018-0386-x ARTICLE PIM2-mediated phosphorylation of hexokinase 2 is critical for tumor growth and paclitaxel resistance in breast cancer 1 1 1 1 1 2 2 3 Tingting Yang ● Chune Ren ● Pengyun Qiao ● Xue Han ● Li Wang ● Shijun Lv ● Yonghong Sun ● Zhijun Liu ● 3 1 Yu Du ● Zhenhai Yu Received: 3 December 2017 / Revised: 30 May 2018 / Accepted: 31 May 2018 / Published online: 9 July 2018 © The Author(s) 2018. This article is published with open access Abstract Hexokinase-II (HK2) is a key enzyme involved in glycolysis, which is required for breast cancer progression. However, the underlying post-translational mechanisms of HK2 activity are poorly understood. Here, we showed that Proviral Insertion in Murine Lymphomas 2 (PIM2) directly bound to HK2 and phosphorylated HK2 on Thr473. Biochemical analyses demonstrated that phosphorylated HK2 Thr473 promoted its protein stability through the chaperone-mediated autophagy (CMA) pathway, and the levels of PIM2 and pThr473-HK2 proteins were positively correlated with each other in human breast cancer. Furthermore, phosphorylation of HK2 on Thr473 increased HK2 enzyme activity and glycolysis, and 1234567890();,: 1234567890();,: enhanced glucose starvation-induced autophagy. As a result, phosphorylated HK2 Thr473 promoted breast cancer cell growth in vitro and in vivo. Interestingly, PIM2 kinase inhibitor SMI-4a could abrogate the effects of phosphorylated HK2 Thr473 on paclitaxel resistance in vitro and in vivo. Taken together, our findings indicated that PIM2 was a novel regulator of HK2, and suggested a new strategy to treat breast cancer. Introduction ATP molecules. -

Ketoconazole and Posaconazole Selectively Target HK2-Expressing Glioblastoma Cells
Published OnlineFirst October 15, 2018; DOI: 10.1158/1078-0432.CCR-18-1854 Translational Cancer Mechanisms and Therapy Clinical Cancer Research Ketoconazole and Posaconazole Selectively Target HK2-expressing Glioblastoma Cells Sameer Agnihotri1, Sheila Mansouri2, Kelly Burrell2, Mira Li2, Mamatjan Yasin, MD2, Jeff Liu2,3, Romina Nejad2, Sushil Kumar2, Shahrzad Jalali2, Sanjay K. Singh2, Alenoush Vartanian2,4, Eric Xueyu Chen5, Shirin Karimi2, Olivia Singh2, Severa Bunda2, Alireza Mansouri7, Kenneth D. Aldape2,6, and Gelareh Zadeh2,7 Abstract Purpose: Hexokinase II (HK2) protein expression is eleva- in vivo. Treatment of mice bearing GBM with ketoconazole ted in glioblastoma (GBM), and we have shown that HK2 and posaconazole increased their survival, reduced tumor could serve as an effective therapeutic target for GBM. Here, we cell proliferation, and decreased tumor metabolism. In interrogated compounds that target HK2 effectively and addition, treatment with azoles resulted in increased pro- restrict tumor growth in cell lines, patient-derived glioma stem portion of apoptotic cells. cells (GSCs), and mouse models of GBM. Conclusions: Overall, we provide evidence that azoles exert Experimental Design: We performed a screen using a set of their effect by targeting genes and pathways regulated by HK2. 15 drugs that were predicted to inhibit the HK2-associated These findings shed light on the action of azoles in GBM. gene signature. We next determined the EC50 of the com- Combined with existing literature and preclinical results, these pounds by treating glioma cell lines and GSCs. Selected data support the value of repurposing azoles in GBM clinical compounds showing significant impact in vitro were used to trials. -

Microrna‑451A Prevents Cutaneous Squamous Cell Carcinoma Progression Via the 3‑Phosphoinositide‑Dependent Protein Kinase‑1‑Mediated PI3K/AKT Signaling Pathway
EXPERIMENTAL AND THERAPEUTIC MEDICINE 21: 116, 2021 MicroRNA‑451a prevents cutaneous squamous cell carcinoma progression via the 3‑phosphoinositide‑dependent protein kinase‑1‑mediated PI3K/AKT signaling pathway JIXING FU*, JIANHUA ZHAO*, HUAMIN ZHANG, XIAOLI FAN, WENJUN GENG and SHAOHUA QIAO Department of Dermatology, Liaocheng Second People's Hospital, Shandong First Medical University Affiliated Liaocheng Second Hospital, Linqing, Shandong 252601, .R.P China Received February 12, 2020; Accepted August 11, 2020 DOI: 10.3892/etm.2020.9548 Abstract. The role of microRNAs (miRNAs/miRs) in pathway, which may offer potential therapeutic targets for the governing the progression of cutaneous squamous cell carci‑ treatment of cSCC. noma (cSCC) has been the focus of recent studies. However, the functional role of miR‑451a in cSCC growth remains Introduction poorly understood. Therefore, the present study aimed to determine the expression levels of miR‑451a in cSCC cell Skin cancer or cutaneous carcinoma is a major worldwide lines and the involvement of miR‑451a in cSCC progression. public health burden which is highly prevalent and demon‑ The results revealed that the expression levels of miR‑451a strates an ever‑increasing incidence with ~108,420 new cases were downregulated in cSCC tissues and cell lines, and that and 11,480 death in the United States in 2020 (1,2). The this subsequently upregulated 3‑phosphoinositide‑dependent majority of diagnosed skin cancer cases are non‑melanoma‑ protein kinase‑1 (PDPK1) expression levels. PDPK1 was tous, consisting of basal cell carcinoma and cutaneous cell validated as a direct target of miR‑451a in cSCC using carcinoma (cSCC), which originate from keratinized epithelial bioinformatics software Starbase, dual‑luciferase reporter cells (3). -
Hk2) in the Breast Cancer Cell Line T47.D1
[CANCERRESEARCH57,2651—2656.July1, 19971 Expression of Human Prostate-specific Glandular Kallikrein Protein (hK2) in the Breast Cancer Cell Line T47.D1 Ming-Li Hsieh, M. Cristine Charlesworth, Marcia Goodmanson, Shaobo Zhang, Thomas Seay, George G. Klee, Donald J. Tindall, and Charles Y. F. Young@ Departments of Urology (M-L H., S. Z, T. S., D. J. T., C. Y. F. Y.], Biochemistry and Molecular Biology [M. C. C., D. J. T., C. Y. F. Y.j, and Laboratory Medicine IM. G.. G. G. K.], Mayo Graduate Schools, Mayo Clinic/Foundation, Rochester, Minnesota 55905 ABSTRACT whether PSA plays a physiological role in these tissues in women remains to be elucidated. Human glandular kallikrein (hK2) protein, like prostate-specific anti The hK2 is another member of the human kallikrein gene family gen (PSA), is produced mainly In prostatic epithellum. It may be useful as (16). The hK2 gene was first discovered in 1987 (17). However, its a new diagnostic indicator for prostate cancer. Recently, a number of hK2-speciflc monoclonal antibodies have been developed that enable us to complete cDNA was not isolated until 1992 (18). Studies of hK2 detect hK2 protein In human prostate tissue, seminal fluid, and scm. mRNA indicate that hK2 is specific for prostatic tissue and is regu Whether hK2 can be expressed, like PSA, in nonprostatic cells is not lated by androgens via the androgen receptor (18—20).To define the known. In this study, we have characterized the presence of hK2 in an biological role and potential clinical utility of hK2 protein for prostate androgen-responsive breast cancer cell line T47-D at both the protein and cancer, recombinant hK2 proteins and hK2 peptides have been syn mRNA levels with an immunoassay, Western blot analysis, Northern blot thesized and used to generate monospecific antibodies (mAbs; Ref. -

Mitochondrial Heteroplasmy Shifting As a Potential Biomarker of Cancer Progression
International Journal of Molecular Sciences Review Mitochondrial Heteroplasmy Shifting as a Potential Biomarker of Cancer Progression Carlos Jhovani Pérez-Amado 1,2 , Amellalli Bazan-Cordoba 1,2, Alfredo Hidalgo-Miranda 1 and Silvia Jiménez-Morales 1,* 1 Laboratorio de Genómica del Cáncer, Instituto Nacional de Medicina Genómica, Mexico City 14610, Mexico; [email protected] (C.J.P.-A.); [email protected] (A.B.-C.); [email protected] (A.H.-M.) 2 Programa de Maestría y Doctorado, Posgrado en Ciencias Bioquímicas, Universidad Nacional Autónoma de México, Mexico City 04510, Mexico * Correspondence: [email protected] Abstract: Cancer is a serious health problem with a high mortality rate worldwide. Given the rele- vance of mitochondria in numerous physiological and pathological mechanisms, such as adenosine triphosphate (ATP) synthesis, apoptosis, metabolism, cancer progression and drug resistance, mito- chondrial genome (mtDNA) analysis has become of great interest in the study of human diseases, including cancer. To date, a high number of variants and mutations have been identified in different types of tumors, which coexist with normal alleles, a phenomenon named heteroplasmy. This mecha- nism is considered an intermediate state between the fixation or elimination of the acquired mutations. It is suggested that mutations, which confer adaptive advantages to tumor growth and invasion, are enriched in malignant cells. Notably, many recent studies have reported a heteroplasmy-shifting phenomenon as a potential shaper in tumor progression and treatment response, and we suggest that each cancer type also has a unique mitochondrial heteroplasmy-shifting profile. So far, a plethora Citation: Pérez-Amado, C.J.; Bazan-Cordoba, A.; Hidalgo-Miranda, of data evidencing correlations among heteroplasmy and cancer-related phenotypes are available, A.; Jiménez-Morales, S. -
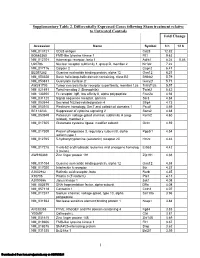
Supplementary Table 2
Supplementary Table 2. Differentially Expressed Genes following Sham treatment relative to Untreated Controls Fold Change Accession Name Symbol 3 h 12 h NM_013121 CD28 antigen Cd28 12.82 BG665360 FMS-like tyrosine kinase 1 Flt1 9.63 NM_012701 Adrenergic receptor, beta 1 Adrb1 8.24 0.46 U20796 Nuclear receptor subfamily 1, group D, member 2 Nr1d2 7.22 NM_017116 Calpain 2 Capn2 6.41 BE097282 Guanine nucleotide binding protein, alpha 12 Gna12 6.21 NM_053328 Basic helix-loop-helix domain containing, class B2 Bhlhb2 5.79 NM_053831 Guanylate cyclase 2f Gucy2f 5.71 AW251703 Tumor necrosis factor receptor superfamily, member 12a Tnfrsf12a 5.57 NM_021691 Twist homolog 2 (Drosophila) Twist2 5.42 NM_133550 Fc receptor, IgE, low affinity II, alpha polypeptide Fcer2a 4.93 NM_031120 Signal sequence receptor, gamma Ssr3 4.84 NM_053544 Secreted frizzled-related protein 4 Sfrp4 4.73 NM_053910 Pleckstrin homology, Sec7 and coiled/coil domains 1 Pscd1 4.69 BE113233 Suppressor of cytokine signaling 2 Socs2 4.68 NM_053949 Potassium voltage-gated channel, subfamily H (eag- Kcnh2 4.60 related), member 2 NM_017305 Glutamate cysteine ligase, modifier subunit Gclm 4.59 NM_017309 Protein phospatase 3, regulatory subunit B, alpha Ppp3r1 4.54 isoform,type 1 NM_012765 5-hydroxytryptamine (serotonin) receptor 2C Htr2c 4.46 NM_017218 V-erb-b2 erythroblastic leukemia viral oncogene homolog Erbb3 4.42 3 (avian) AW918369 Zinc finger protein 191 Zfp191 4.38 NM_031034 Guanine nucleotide binding protein, alpha 12 Gna12 4.38 NM_017020 Interleukin 6 receptor Il6r 4.37 AJ002942 -

A Switch in Metabolism Precedes Increased Mitochondrial Biogenesis in Respiratory Chain-Deficient Mouse Hearts
A switch in metabolism precedes increased mitochondrial biogenesis in respiratory chain-deficient mouse hearts Anna Hansson*, Nicole Hance*, Eric Dufour*, Anja Rantanen*, Kjell Hultenby†, David A. Clayton‡, Rolf Wibom§, and Nils-Go¨ ran Larsson*¶ Departments of *Medical Nutrition and Biosciences and §Laboratory Medicine and †Clinical Research Center, Karolinska Institutet, Novum, Karolinska University Hospital, S-141 86 Stockholm, Sweden; and ‡Howard Hughes Medical Institute, 4000 Jones Bridge Road, Chevy Chase, MD 20815-6789 Communicated by Rolf Luft, Karolinska Institutet, Stockholm, Sweden, December 30, 2003 (received for review November 15, 2003) We performed global gene expression analyses in mouse hearts plified by increased levels of transcripts encoding the glycolytic with progressive respiratory chain deficiency and found a meta- enzyme GAPDH in respiratory chain-deficient heart muscle bolic switch at an early disease stage. The tissue-specific mitochon- (14) and normal GAPDH transcript levels in respiratory chain- drial transcription factor A (Tfam) knockout mice of this study deficient cerebral cortex (9). Our studies have also demonstrated displayed a progressive heart phenotype with depletion of mtDNA that the mitochondrial mass increases in respiratory chain- and an accompanying severe decline of respiratory chain enzyme deficient embryos and differentiated mouse tissues, suggesting activities along with a decreased mitochondrial ATP production that increased mitochondrial biogenesis represents a cellular rate. These characteristics were observed after 2 weeks of age and compensatory mechanism. Measurement of the MAPR has became gradually more severe until the terminal stage occurred at demonstrated that an increase of mitochondrial mass increases 10–12 weeks of age. Global gene expression analyses with mi- overall ATP production to near normal levels in mitochondrial croarrays showed that a metabolic switch occurred early in the myopathy mice (11). -

Cancer As a Metabolic Disease
Merrimack College Merrimack ScholarWorks Honors Senior Capstone Projects Honors Program Spring 2017 Cancer as a Metabolic Disease Javaria Haseeb Merrimack College, [email protected] Follow this and additional works at: https://scholarworks.merrimack.edu/honors_capstones Part of the Cancer Biology Commons, Cells Commons, and the Nutritional and Metabolic Diseases Commons Recommended Citation Haseeb, Javaria, "Cancer as a Metabolic Disease" (2017). Honors Senior Capstone Projects. 27. https://scholarworks.merrimack.edu/honors_capstones/27 This Capstone - Open Access is brought to you for free and open access by the Honors Program at Merrimack ScholarWorks. It has been accepted for inclusion in Honors Senior Capstone Projects by an authorized administrator of Merrimack ScholarWorks. For more information, please contact [email protected]. 1 Cancer as a Metabolic Disease Javaria Haseeb Department of Biochemistry, Merrimack College, North Andover MA 01845, USA Abstract Despite decades of intensive scientific and medical efforts to develop efficient and effective treatments for cancer, it remains one of the prime causes of death today. For example, in 2016, there will be an estimated 1,685,210 new cases of cancer and 595,690 deaths due to cancer in the United States alone (National Cancer Institute). Worldwide in 2012, there were an estimated 14 million new cases of cancer and 8.2 million deaths due to cancer. In order to come up with better methods of detection and more successful modes of treatment, it is crucial that scientists understand the depth of not only what causes cancer but also what sustains it. This literature review examines cancer as a metabolic disease. More specifically, it summarizes carbohydrate metabolism and compares and contrasts the roles of the glucose transporter, the metabolic enzymes hexokinase, pyruvate kinase, citrate synthase, succinate dehydrogenase, cytochrome c oxidase, ATP synthase, and the tumor suppressor protein p53 in normal versus cancer cells.