BTS Clinical Statement on Pulmonary Sarcoidosis
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
SIGN158 British Guideline on the Management of Asthma
SIGN158 British guideline on the management of asthma A national clinical guideline First published 2003 Revised edition published July 2019 Key to evidence statements and recommendations Levels of evidence 1++ High-quality meta-analyses, systematic reviews of RCTs, or RCTs with a very low risk of bias 1+ Well-conducted meta-analyses, systematic reviews, or RCTs with a low risk of bias 1– Meta-analyses, systematic reviews, or RCTs with a high risk of bias 2++ High-quality systematic reviews of case-control or cohort studies High-quality case-control or cohort studies with a very low risk of confounding or bias and a high probability that the relationship is causal 2+ Well-conducted case-control or cohort studies with a low risk of confounding or bias and a moderate probability that the relationship is causal 2– Case-control or cohort studies with a high risk of confounding or bias and a significant risk that the relationship is not causal 3 Non-analytic studies, eg case reports, case series 4 Expert opinion Grades of recommendation Note: The grade of recommendation relates to the strength of the supporting evidence on which the evidence is based. It does not reflect the clinical importance of the recommendation. A At least one meta-analysis, systematic review, or RCT rated as 1++, and directly applicable to the target population; or A body of evidence consisting principally of studies rated as 1+, directly applicable to the target population, and demonstrating overall consistency of results B A body of evidence including studies rated -

A Professional Development Framework for Paediatric Respiratory Nursing
A professional development framework for paediatric respiratory nursing ISSN 2040-2023: British Thoracic Society Reports Vol 12, Issue 2, May 2021 1 ACKNOWLEDGEMENTS: We are grateful to colleagues at the National Paediatric Respiratory and Allergy Nurses Group (NPRANG) for their support with the development of this document. In particular: Ann McMurray Asthma Nurse Specialist, Royal Hospital for Children and Young People, Edinburgh. NPRANG Chair Bethan Almeida Clinical Nurse Specialist for Paediatric Asthma and Allergy, Imperial College Healthcare NHS Trust Tricia McGinnity Paediatric Cystic Fibrosis Nurse Specialist, Southampton Children's Hospital Emma Bushell Paediatric Respiratory Nurse Specialist – Asthma, Frimley Health NHS Foundation Trust This document has been adapted from the following publication: British Thoracic Society, A professional development framework for respiratory nursing (1). The authors of this original document are: Samantha Prigmore, Co-chair Consultant respiratory nurse, St Georges University Hospitals NHS Foundation Trust Helen Morris, Co-chair ILD nurse specialist, Wythenshawe Hospital Alison Armstrong Nurse consultant (assisted ventilation), Royal Victoria Infirmary Susan Hope Respiratory nurse specialist, Royal Stoke University Hospital Karen Heslop-Marshall Nurse consultant, Royal Victoria Infirmary Jacqui Pollington Respiratory nurse consultant, Rotherham NHS Foundation Trust CONTENTS: Introduction Method of production How to use this document Competency table (Band 5, 6, 7 and 8) Supporting evidence Acknowledgements Declarations of Interest References Content from this document may be reproduced with permission from BTS as long as you conform to the following conditions: • The text must not be altered in any way. • The correct acknowledgement must be included. 2 Introduction Paediatric respiratory nurses are an important component of the multi-professional team for a wide variety of respiratory conditions, providing holistic care for patients in a variety of settings. -
17Th & 18Th June 2021 Speakers' Details and Presentation Summaries
th th SUMMER MEETING ONLINE – 17 & 18 June 2021 Speakers’ Details and Presentation Summaries The following details are in programme order. Use the PDF search button to quickly find a session or speaker. OPEN SESSION – NATIONAL ASTHMA AND COPD AUDIT PROGRAMME Thursday 17th June: 08:00-09:00 Dr James Calvert qualified in Medicine from Oxford Session aims and overview University in 1992. He studied Public Health as a 1) To summarise the main findings of the 2020/21 Fulbright Scholar at Harvard University before NACAP reports. completing his PhD in Asthma Epidemiology in South 2) To outline the QI support opportunities offered by Africa and London. NACAP to clinical and audit teams. He was a Consultant Respiratory Specialist in Bristol from 2006-2021. He is now a Respiratory Consultant Professor Roberts will present a summary of key and Medical Director of Aneurin Bevan University reported findings from across the audits from the last Health Board in Wales. 12 months, highlighting areas for further James has worked with colleagues in the South West improvement. He will speak about the impact of and at NHS England to improve access to integrated COVID-19 on standards of care and on audit services for respiratory patients. He has Chaired the participation, along with plans to improve automated British Thoracic Society (BTS) Professional and extraction of NACAP data. Organisational Standards Committee and has been Dr Calvert will talk about the QI programme to be the BTS National Audit Lead. He has a longstanding launched this year. interest in quality improvement in health care and has A discussion will follow around ideas for improving worked with the BTS, NHS Improving Value, the Royal NACAP support to clinical and audit teams. -

STATE of OKLAHOMA OCCUPATIONAL THERAPY PRACTICE ACT Title 59 O.S., Sections 888.1 - 888.16
Amended: November 1, 2019 STATE OF OKLAHOMA OCCUPATIONAL THERAPY PRACTICE ACT Title 59 O.S., Sections 888.1 - 888.16 INDEX 888.1. Short Title 888.2 Purpose 888.3. Definitions 888.4. License required - Application of Act 888.5. Practices, services and activities not prohibited 888.6. Application for license - information required 888.7. Application for license - form - examination and reexamination 888.8. Waiver of examination, education or experience requirement 888.9. Denial, refusal, suspension, revocation, censure, probation and reinstatement of license 888.10. Renewal of license - continuing education 888.11. Fees 888.12. Oklahoma Occupational Therapy Advisory Committee - creation - membership - term - vacancies - removal - liability 888.13. Oklahoma Occupational Therapy Advisory Committee - officers - meetings - rules - records - expenses 888.14. Powers and duties of Committee 888.15. Titles and abbreviations - misrepresentation - penalties -1- 888.1. Short title This act shall be known and cited as the "Occupational Therapy Practice Act". 888.2. Purpose In order to safeguard the public health, safety and welfare, to protect the public from being misled by incompetent and un-authorized persons, to assure the highest degree of professional conduct on the part of occupational therapists and occupational therapy assistants, and to assure the availability of occupational therapy services of high quality to persons in need of such services, it is the purpose of this act to provide for the regulation of persons offering occupational therapy -

Disparities in Respiratory Health
American Thoracic Society Documents An Official American Thoracic Society/European Respiratory Society Policy Statement: Disparities in Respiratory Health 6 Dean E. Schraufnagel, Francesco Blasi, Monica Kraft, Mina Gaga, Patricia Finn, Klaus Rabe This official statement of the American Thoracic Society (ATS) and the European Respiratory Society (ERS) was approved by the ATS Board of Directors, XXXXXXXXX, and by the ERS XXXXXXXX, XXXXXXXXXX [[COMP: Insert internal ToC]] 1 Abstract Background: Health disparities, defined as a significant difference in health between populations, are more common for diseases of the respiratory system than for those of other organ systems because of the environmental influence on breathing and the variation of the environment among different segments of the population. The lowest social groups are up to 14 times more likely to have respiratory diseases than are the highest. Tobacco smoke, air pollution, environmental exposures, and occupational hazards affect the lungs more than other organs and occur disproportionately in ethnic minorities and those with lower socioeconomic status. Lack of access to quality health care contributes to disparities. Methods: The executive committees of the American Thoracic Society (ATS) and European Respiratory Society (ERS) established a writing committee to develop a policy on health disparities. The document was reviewed, edited, and approved by their full executive committees and boards of directors of the societies. Results: This document expresses a policy to address health disparities by promoting scientific inquiry and training, disseminating medical information and best practices, and monitoring and advocating for public respiratory health. ERS and ATS have strong international commitments and work with leaders from governments, academia, and other organizations to address and reduce avoidable health inequalities. -

WFOT ANNOUNCEMENTS & DELEGATE UPDATE May 2014
WFOT ANNOUNCEMENTS & DELEGATE UPDATE May 2014 WFOT BULLETIN – MAY 2014 This edition addresses Assistive Technology and Information Technology. Take a trip around the world with OT authors from Austria, Australia, Bangladesh, Canada, Denmark, Finland, Germany, Hong Kong, Latvia, Netherlands, Romania, Sweden, Singapore, United Kingdom, USA AOTA CONFERENCE – BALTIMORE, MD – April 2014 – PLETHORA OF INTERNATIONAL EVENTS: More than 60 international and cross cultural sessions addressed topics like: service learning, fieldwork, occupational justice, human rights, refugees, cultural fluidity, disaster response, assistive technologies, OT Education in under resourced areas, and special populations such as women with obstetric fistulas. 16th WORLD CONGRESS OF OT - YOKOHAMA, JAPAN - June 18-21, 2014 “SHARING TRADITIONS, CREATING FUTURES” REGISTER: http://www.wfot.org/wfot2014/eng/index.html STUDENTS: WOW - registration is only $100 for the four day conference! FELLOW TRAVELERS: http://otconnections.aota.org/more_groups/wfot_congress_2014_japan_preparations_and_reflections/default.aspx HELPING: Donate: http://www.wfot.org/wfot2014/eng/contents/donation.html SPONSORSHIP & EXHIBITING: http://www.wfot.org/wfot2014/eng/contents/sponsor.html PROMOTING: WFOT resources & media pack: http://www.wfot.org/ResourceCentre.aspx WORLD HEALTH ORGANIZATION (WHO) INVITES OCCUPATIONAL THERAPISTS TO JOIN THE GLOBAL CLINICAL PRACTICE NETWORK FOR ICD-11 MENTAL AND BEHAVIOURAL DISORDERS Dear Colleague: The World Health Organization’s Department of Mental Health and Substance -
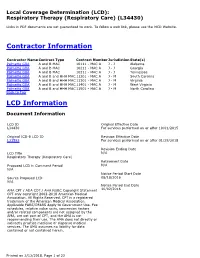
Local Coverage Determination for Respiratory Therapy
Local Coverage Determination (LCD): Respiratory Therapy (Respiratory Care) (L34430) Links in PDF documents are not guaranteed to work. To follow a web link, please use the MCD Website. Contractor Information Contractor Name Contract Type Contract Number Jurisdiction State(s) Palmetto GBA A and B MAC 10111 - MAC A J - J Alabama Palmetto GBA A and B MAC 10211 - MAC A J - J Georgia Palmetto GBA A and B MAC 10311 - MAC A J - J Tennessee Palmetto GBA A and B and HHH MAC 11201 - MAC A J - M South Carolina Palmetto GBA A and B and HHH MAC 11301 - MAC A J - M Virginia Palmetto GBA A and B and HHH MAC 11401 - MAC A J - M West Virginia Palmetto GBA A and B and HHH MAC 11501 - MAC A J - M North Carolina Back to Top LCD Information Document Information LCD ID Original Effective Date L34430 For services performed on or after 10/01/2015 Original ICD-9 LCD ID Revision Effective Date L31593 For services performed on or after 01/29/2018 Revision Ending Date LCD Title N/A Respiratory Therapy (Respiratory Care) Retirement Date Proposed LCD in Comment Period N/A N/A Notice Period Start Date Source Proposed LCD 08/18/2016 N/A Notice Period End Date AMA CPT / ADA CDT / AHA NUBC Copyright Statement 10/02/2016 CPT only copyright 2002-2018 American Medical Association. All Rights Reserved. CPT is a registered trademark of the American Medical Association. Applicable FARS/DFARS Apply to Government Use. Fee schedules, relative value units, conversion factors and/or related components are not assigned by the AMA, are not part of CPT, and the AMA is not recommending their use. -

BTS Clinical Statement on Pulmonary Arteriovenous Malformations
Downloaded from http://thorax.bmj.com/ on November 15, 2017 - Published by group.bmj.com BTS Clinical Statement British Thoracic Society Clinical Statement on Pulmonary Arteriovenous Malformations Claire L Shovlin,1,2 Robin Condliffe,3 James W Donaldson,4 David G Kiely,3,5 Stephen J Wort,6,7 on behalf of the British Thoracic Society 1NHLI Vascular Science, Imperial EXECUTIVE SUMMARY high cardiac output.16 PAVMs of any size allow College London, London, UK Pulmonary arteriovenous malformations (PAVMs) are paradoxical emboli that may cause ischaemic 2Respiratory Medicine, and structurally abnormal vascular communications that strokes,17 18 myocardial infarction,18–20 cerebral VASCERN HHT European 17 21–23 Reference Centre, Hammersmith provide a continuous right-to-left shunt between (brain) and peripheral abscesses, discitis and Hospital, Imperial College pulmonary arteries and veins. Their importance stems migraines.24–26 Less frequently, PAVMs may cause Healthcare NHS Trust, London, from the risks they pose (>1 in 4 patients will have haemoptysis, haemothorax27–29 and/or maternal UK 29 3 a paradoxical embolic stroke, abscess or myocardial death in pregnancy. Due to compensatory adap- Pulmonary Vascular Disease Unit, Royal Hallamshire Hospital, infarction while life-threatening haemorrhage affects tations, respiratory symptoms are frequently absent Sheffield, UK 1 in 100 women in pregnancy), opportunities for risk or not recognised until PAVM treatment has led 4 Dept of Respiratory Medicine, prevention, surprisingly high prevalence and under- to improvement or resolution.1 13–16 26 However, Derby Teaching Hospitals NHS appreciation, thus representing a challenging condition at least one in three patients with PAVMs will Foundation Trust, Derby, UK 5Department of Infection, for practising healthcare professionals. -

Primary Care Summary of the British Thoracic Society Guidelines for the Management of Community Acquired Pneumonia in Adults: 2009 Update
Copyright PCRS-UK - reproduction prohibited Primary Care Respiratory Journal (2010); 19(1): 21-27 GUIDELINE SUMMARY Primary care summary of the British Thoracic Society Guidelines for the management of community acquired pneumonia in adults: 2009 update Endorsed by the Royal College of General Practitioners and the Primary Care Respiratory Society UK Mark L Levya, Ivan Le Jeuneb, Mark A Woodheadc, John T Macfarlaned, *Wei Shen Limd on behalf of the British Thoracic Society Community Acquired Pneumonia in Adults Guideline Group UK a Senior Clinical Research Fellow, Allergy and Respiratory Research Group, Division of Community Health Sciences: GP section, University of Edinburgh, Scotland, UK b Departments of Acute and Respiratory Medicine, Nottingham University Hospitals NHS Trust, Nottingham, UK c Department of Respiratory Medicine, Manchester Royal Infirmary, Manchester, UK Society d Department of Respiratory Medicine, Nottingham University Hospitals NHS Trust, Nottingham, UK Received 11th January 2009; revised version received 29th January 2010; accepted 1st February 2010; online 15th February 2010 Abstract Introduction: The identification and management of adults presentingRespiratory with pneumonia is a major challenge for primary care health professionals. This paper summarises the key recommendations of the Britishprohibited Thoracic Society (BTS) Guidelines for the management of Community Acquired Pneumonia (CAP) in adults. Method: Systematic electronic database searches were conductedCare in order to identify potentially relevant studies that might inform guideline recommendations. Generic study appraisal checklists and an evidence grading from A+ to D were used to indicate the strength of the evidence upon which recommendations were made. Conclusions: This paper provides definitions, keyPrimary messages, and recommendations for handling the uncertainty surrounding the clinical diagnosis, assessing severity, management, and follow-upReproduction of patients with CAP in the community setting. -

At Work in the World
Perspectives in Medical Humanities At Work in the World Proceedings of the Fourth International Conference on the History of Occupational and Environmental Health Edited by Paul D. Blanc, MD and Brian Dolan, PhD Page Intentionally Left Blank At Work in the World Proceedings of the Fourth International Conference on the History of Occupational and Environmental Health Perspectives in Medical Humanities Perspectives in Medical Humanities publishes scholarship produced or reviewed under the auspices of the University of California Medical Humanities Consortium, a multi-campus collaborative of faculty, students and trainees in the humanities, medi- cine, and health sciences. Our series invites scholars from the humanities and health care professions to share narratives and analysis on health, healing, and the contexts of our beliefs and practices that impact biomedical inquiry. General Editor Brian Dolan, PhD, Professor of Social Medicine and Medical Humanities, University of California, San Francisco (ucsf) Recent Monograph Titles Health Citizenship: Essays in Social Medicine and Biomedical Politics By Dorothy Porter (Fall 2011) Paths to Innovation: Discovering Recombinant DNA, Oncogenes and Prions, In One Medical School, Over One Decade By Henry Bourne (Fall 2011) The Remarkables: Endocrine Abnormalities in Art By Carol Clark and Orlo Clark (Winter 2011) Clowns and Jokers Can Heal Us: Comedy and Medicine By Albert Howard Carter iii (Winter 2011) www.medicalhumanities.ucsf.edu [email protected] This series is made possible by the generous support of the Dean of the School of Medicine at ucsf, the Center for Humanities and Health Sciences at ucsf, and a Multi-Campus Research Program grant from the University of California Office of the President. -

Your Career in Occupational Therapy: Workforce Trends In
Resources for students from The American Occupational Therapy Association Your career in Occupational Therapy he demand for occupational therapy services is Workforce Trends strong. The U.S. Department of Labor’s Bureau Tof Labor Statistics (BLS) projected employment of occupational therapists to increase by 26% and of in Occupational occupational therapy assistants to increase by 30% or more between 2008 and 2018. This projection is based on the Bureau’s assumptions that demographic trends Therapy and advances in medical technology will continue to fuel demand for therapy services. Occupational therapy workforce shortages are appear- ing in selected markets and sectors. Demand for occu- pational therapy services in early intervention programs and in schools that enroll children with disabilities who are served under the federal Individuals with Disabilities Education Improvement Act of 2004 remains strong. Newly emerging areas of practice for occupational therapy practitioners related to the needs of an aging population are increasing demand for services. These in- clude low-vision rehabilitation; treatment of Alzheimer’s disease and other forms of dementia, including caregiver training; older driver safety and rehabilitation; assisted living; and home safety and home modifications to en- able “aging in place.” In a survey of education program directors, the overwhelming majority (80%+) of the 318 programs reported that more than 80% of occupational therapy and occupational therapy assistant graduates were able to secure jobs within 6 months of graduation. Many of these graduates had secured job offers prior to graduating. Current Workforce Based on 2010 survey results from state occupational therapy regulatory boards, the American Occupational Therapy Association (AOTA) estimates the current active occupational therapy workforce to be roughly 137,000 practitioners. -

The Role of Occupational Therapy with Children and Youth
Fact Sheet Occupational Therapy’s Role with Children and Youth Occupational therapy practitioners work with children, youth, and their families, caregivers, and teachers to pro- mote active participation in activities or occupations that are meaningful to them. Occupation refers to activities that support the health, well-being, and development of an individual (American Occupational Therapy Asso- ciation, 2014). For children and youth, occupations are activities that enable them to learn and develop life skills (e.g., preschool and school activities), be creative and/ or derive enjoyment (e.g., play), and thrive (e.g., self- care and relationships with others) as both a means and an end. Occupational therapy practitioners work with children of all ages and abilities through the habilitation and rehabilitation process. Recommended interventions are based on a thorough understanding of typical development, the environments in which children engage (e.g., home, school, playground) and the impact of disability, illness, and impairment on the individual child’s development, play, learn- ing, and overall occupational performance. Occupational therapy practitioners collaborate with parents/caregivers and other professionals to identify and meet the needs of children experiencing delays or challenges in development; identifying and modifying or compensating for barri- ers that interfere with, restrict, or inhibit functional performance; teaching and modeling skills and strategies to children, their families, and other adults in their environments to extend therapeutic intervention to all aspects of daily life tasks; and adapting activities, materials, and environmental conditions so children can participate under different conditions and in various settings (e.g., home, school, sports, community programs). Developmental Needs The primary occupations of infants, toddlers, and young children are playing, learning, and interacting with caregivers and, eventually, their peers.