Wind, Burping, Flatulence and Bloating Information Leaflet
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

2.04.26 Fecal Analysis in the Diagnosis of Intestinal Dysbiosis and Irritable Bowel Syndrome
MEDICAL POLICY – 2.04.26 Fecal Analysis in the Diagnosis of Intestinal Dysbiosis and Irritable Bowel Syndrome BCBSA Ref. Policy: 2.04.26 Effective Date: July 1, 2021 RELATED MEDICAL POLICIES: Last Revised: June 8, 2021 None Replaces: N/A Select a hyperlink below to be directed to that section. POLICY CRITERIA | DOCUMENTATION REQUIREMENTS | CODING RELATED INFORMATION | EVIDENCE REVIEW | REFERENCES | HISTORY ∞ Clicking this icon returns you to the hyperlinks menu above. Introduction Intestinal dysbiosis is a condition that occurs when the microorganisms in the digestive tract are out of balance. This condition is believed to cause diseases of the digestive tract, including poor nutrient absorption, overgrowth of certain bacteria, and irritable bowel syndrome (IBS). Symptoms of these digestive problems are similar and may include: abdominal pain, excess gas, bloating, and changes in bowel movements (constipation or diarrhea, or both). One method of diagnosing digestive disorders is by testing a fecal sample. Using fecal analysis to diagnose intestinal dysbiosis, IBS, malabsorption, or small intestinal overgrowth of bacteria is unproven (investigational). More studies are needed to see if this testing improves health outcomes. Note: The Introduction section is for your general knowledge and is not to be taken as policy coverage criteria. The rest of the policy uses specific words and concepts familiar to medical professionals. It is intended for providers. A provider can be a person, such as a doctor, nurse, psychologist, or dentist. A provider also can be a place where medical care is given, like a hospital, clinic, or lab. This policy informs them about when a service may be covered. -

THE SKY IS the LIMIT for WIND POWER Wind Energy Is One of the Best Sources of Alternative Energy
Mechanical Contractors July— Sept 2018 THE SKY IS THE LIMIT FOR WIND POWER Wind energy is one of the best sources of alternative energy. Wind refers to the movement of air from high pressure areas to low pressure areas. Wind is caused by uneven heating of the earth’s surface by the sun. Hot air rises up and cool air flows in to take its place. Winds will always exist as long as solar energy exists and peo- ple will be able to harness the energy forever. Windmills have been in use since 2000 B.C. and were first developed in Persia and China. Ancient mariners sailed to distant lands by making use of winds. Farmers used wind power to pump water and for grinding grains. Today the most popular use of wind energy is converting it to electrical energy to meet the critical energy needs of the planet. It is a renewable source of energy and does not produce any pollutants or emissions during opera- tion that could harm the environment. Wind power is one of the cleanest and safest method of generating renewable electricity. Wind farms can be created to trap wind energy by placing multiple wind turbines in the same location for the purpose of generating large amounts of electric power. Wind energy is mostly harnessed by wind turbines which are as high as 20 story buildings and usually have three blades which are 60 meters long. They resemble giant airplane propellers mounted on a stick. The blades are spun by the wind which transfers motion to a shaft connected to a generator which produces electricity. -

Pancreatic Cancer
A Patient’s Guide to Pancreatic Cancer COMPREHENSIVE CANCER CENTER Staff of the Comprehensive Cancer Center’s Multidisciplinary Pancreatic Cancer Program provided information for this handbook GI Oncology Program, Patient Education Program, Gastrointestinal Surgery Department, Medical Oncology, Radiation Oncology and Surgical Oncology Digestive System Anatomy Esophagus Liver Stomach Gallbladder Duodenum Colon Pancreas (behind the stomach) Anatomy of the Pancreas Celiac Plexus Pancreatic Duct Common Bile Duct Sphincter of Oddi Head Body Tail Pancreas ii A Patient’s Guide to Pancreatic Cancer ©2012 University of Michigan Comprehensive Cancer Center Table of Contents I. Overview of pancreatic cancer A. Where is the pancreas located?. 1 B. What does the pancreas do? . 2 C. What is cancer and how does it affect the pancreas? .....................2 D. How common is pancreatic cancer and who is at risk?. .3 E. Is pancreatic cancer hereditary? .....................................3 F. What are the symptoms of pancreatic cancer? ..........................4 G. How is pancreatic cancer diagnosed?. 7 H. What are the types of cancer found in the pancreas? .....................9 II. Treatment A. Treatment of Pancreatic Cancer. 11 1. What are the treatment options?. 11 2. How does a patient decide on treatment? ..........................12 3. What factors affect prognosis and recovery?. .12 D. Surgery. 13 1. When is surgery a treatment?. 13 2. What other procedures are done?. .16 E. Radiation therapy . 19 1. What is radiation therapy? ......................................19 2. When is radiation therapy given?. 19 3. What happens at my first appointment? . 20 F. Chemotherapy ..................................................21 1. What is chemotherapy? ........................................21 2. How does chemotherapy work? ..................................21 3. When is chemotherapy given? ...................................21 G. -

Symptoms What Is IBS?
IBS Irritable Bowel Syndrome What is IBS? Symptoms IBS is a functional gut disorder, meaning the normal way the intestine moves, the sensitiv- ity of nerves in the intestine, or the way the brain controls the intestinal functions, is • People with IBS normally experience recurring episodes of diarrhea (IBS-D), constipation (IBS-C) impaired. The exact cause of IBS is still not or a mixture of both (IBS-M), alongside intense understood, but the research suggests a cramping that can last for hours. combination of factors can lead to IBS: family history of IBS, stress, previous gut infections • Symptoms can also include bloating, gas, abdom- and an imbalance in gut bacteria are a few inal distension, intermittent indigestion, nausea, potential causes. and feeling full or uncomfortable after eating. • Some people may have symptoms in their The diagnostic criteria for IBS is defined as throat/upper stomach area, including burping, recurrent abdominal pain or discomfort for at reflux-type symptoms, chest pain and feeling a least 3 days per month for the last 3 months, lump in the throat or stomach. These symptoms with at least two of the following: may indicate functional dyspepsia, which is a functional gut disorder of the upper digestive tract related to IBS. • Improvement of symptoms with Talk to your doctor about differentiating between defecation the two based on your symptoms. • Symptom onset associated with a change in the frequency of stool Did you know? • Symptom onset associated with a IBS is the most common functional digestive change in the form/appearance of stool disorder, affecting between 13-20% of Canadians. -

Irritable Bowel Syndrome (IBS) Primary Care Pathway
Irritable Bowel Syndrome (IBS) Primary Care Pathway Quick links: Pathway primer Expanded details Advice options Patient pathway 1. Suspected IBS Recurrent abdominal pain at least one day per week (on average) in the last 3 months, with two or more of the following: • Related to defecation (either increasing or improving pain) • Associated with a change in frequency of stool • Associated with a change in form (appearance) of stool Typical Features of IBS • Intestinal: bloating, flatulence, nausea, burping, early satiety, dyspepsia • Extra intestinal: dysuria, frequent/urgent urination, widespread musculoskeletal pain, dysmenorrhea, dyspareunia, fatigue, anxiety, depression Positive 2. Initial workup for celiac • Medical history, physical exam, assess secondary causes of symptoms • Serological screening to exclude celiac • CBC, Ferritin 6. Refer for consultation and/or endoscopy 3. Alarm features Yes • Family history of IBD or colorectal cancer (first degree) • GI bleeding/anemia • Nocturnal symptoms • Onset after age 50 • Unintended weight loss (>5% over 6-12 months) No Presumed Diagnosis of IBS 4. Potential approaches to IBS treament (all subtypes) • Dietary modifications: assess common food triggers, psyllium supplementation (soluble fibre), ensure adequate fluids • Physical activity: 20+ minutes of exercise almost daily; aiming for 150 min/week • Psychological treatment: patient counselling and reassurance, Cognitive Behavioural Therapy, hypnotherapy, screen and treat any underlying sleep or mood disorder where relevant • Pharmacologic therapy: antispasmodics (hyoscine butylbromide, dicyclomine hydrochloride, pinaverium bromide), enteric coated peppermint oil 5. Specific approaches based on IBS subtypes IBS-D IBS-M/U IBS-C (diarrhea predominant) (mixed/undefined) (constipation predominant) Further testing for patients • Loperamide • Pay particular attention to • Adequate fibre and water with high clinical suspicion of • Tricyclic antidepressants lifestyle & dietary principles intake IBD. -

An Osteopathic Approach to Reduction of Readmissions for Neonatal Jaundice
Osteopathic Family Physician (2013) 5, 17–23 REVIEW ARTICLE An osteopathic approach to reduction of readmissions for neonatal jaundice Rachel Click, DO,a Julie Dahl-Smith, DO,a Lindsay Fowler, DO,a Jacqueline DuBose, MD,a Margi Deneau-Saxton, RN, CCCE, CIMI, CLC, CPD,b Jennifer Herbert, MDc From aGeorgia Health Sciences University, Medical College of Georgia, Department of Family Medicine, GA; bGeorgia Health System, OB Labor and Delivery, GA; and cUniversity Primary Care, Evans, GA. KEYWORDS: Jaundice is a potentially life-threatening condition that continues to affect at-risk newborns, accounting Breastfeeding; for continued hospital readmissions. As family physicians, we should be cognizant of neonates who may Jaundice; be at risk for jaundice, including those with pathologic jaundice as well as newborns of breastfeeding Prevention; mothers, and ensure sufficient intervention is taken to help prevent further elevations in bilirubin levels. Hyperbilirubinemia; Interventions are likely to include evaluation for sepsis, education regarding feeding frequencies for both Neonatal massage breast- and bottle-fed neonates, reviewing maternal and hematologic risk factors for neonatal jaundice, and considering inborn errors of metabolism. An additional measure family physicians may consider is that of neonatal massage for those with elevated bilirubin levels. Neonatal massage, though not widely used, has been proven to promote excess bilirubin excretion, thus decreasing length of hospital stay; all the while, providing an intervention that allows parents to take an active role. r 2013 Elsevier Inc. All rights reserved. Introduction morbidity rate with bilirubin 4 20 mg/dL. “It has been estimated that the risk of kernicterus in infants with total Jaundice is a product of excess bilirubin (a product of serum bilirubin (TSB) greater than 30 mg/dL is about 1 in broken down red blood cells), which manifests as a 7 infants”.1 Less serious complications of hyperbilirubine- yellowing of the skin and eyes. -

INFORMED CARING JAUNDICE Neonatal Jaundice BILIARY
1 INFORMED CARING Situations with Adults and Children with Gallbladder, Liver and Pancreatic Disorders 2 JAUNDICE ä Does NOT mean hepatitis ä Increased breakdown of RBCs ä Altered bilirubin breakdown ä Impeded flow through liver or bile duct ä First seen in sclera, then skin 3 Neonatal Jaundice ä Not liver failure ä RBC breakdown ä Phototherapy 4 BILIARY ATRESIA ä Jaundice 2-3 weeks after birth ä Easy bruising ä Stools putty like ä Tea colored urine ä Abdominal/organ distension 5 4 F’s of Gallbladder ä Fair ä Fat X size of person X amount in diet ä Fertile X BCP X Multiparity ä Forty 6 Cholelithiasis ä Calculi within the duct or gallbladder ä Severe colicky, cramp-like pain X radiates to shoulder blade X Murphy's sign ä Cholecystitis: inflammation X Can be caused by trauma, fasting, TPN or abdominal surgery 7 Diagnostic Studies ä Ultrasound of abdomen 1 X not for the obese ä HIDA scan X nuclear medicine ä Cholangiograms X endoscopic X transvenous X intraoperative 8 Post-op Care ä High abdominal incision X respiratory compromise ä T-tube X patients need to know how to empty it X may clamp it prior to removal X caution not dislodged with movements ä NO Morphine X spasms of sphincter of Oddi 9 Post-op Nutrition ä Limited fat in diet X can have rapid transit times ä Potential fat soluble vitamin deficit X A, D, E and K ä Weight loss diet 10 LIVER FAILURE ä Cirrhosis ä Drug toxicity X acetaminophen, anesthetics, HCTZ, chemotherapy ä Infection ä Cancer ä ETOH is single most linked cause 11 LIVER FAILURE S/S ä Don’t show up until 80-90% failed -

Symptomatic Approach to Gas, Belching and Bloating 21
20 Osteopathic Family Physician (2019) 20 - 25 Osteopathic Family Physician | Volume 11, No. 2 | March/April, 2019 Gennaro, Larsen Symptomatic Approach to Gas, Belching and Bloating 21 Review ARTICLE to escape. This mechanism prevents the stomach from becoming IRRITABLE BOWEL SYNDROME (IBS) Symptomatic Approach to Gas, Belching and Bloating damaged by excessive dilation.2 IBS is abdominal pain or discomfort associated with altered with OMT Treatment Options Many patients with GERD report increased belching. Transient bowel habits. It is the most commonly diagnosed GI disorder lower esophageal sphincter (LES) relaxation is the major and accounts for about 30% of all GI referrals.7 Criteria for IBS is recurrent abdominal pain at least one day per week in the Carly Gennaro, DO1; Helaine Larsen, DO1 mechanism for both belching and GERD. Recent studies have shown that the number of belches is related to the number of last three months associated with at least two of the following: times someone swallows air. These studies have concluded that 1) association with defecation, 2) change in stool frequency, 1 Good Samaritan Hospital Medical Center, West Islip, NY patients with GERD swallow more air in response to heartburn and 3) change in stool form. Diagnosis should be made using these therefore belch more frequently.3 There is no specific treatment clinical criteria and limited testing. Common symptoms are for belching in GERD patients, so for now, physicians continue to abdominal pain, bloating, alternating diarrhea and constipation, treat GERD with proton pump inhibitors (PPIs) and histamine-2 and pain relief after defecation. Pain can be present anywhere receptor antagonists with the goal of suppressing heartburn and in the abdomen, but the lower abdomen is the most common KEYWORDS: ABSTRACT: Intestinal gas production is a normal physiologic progress. -
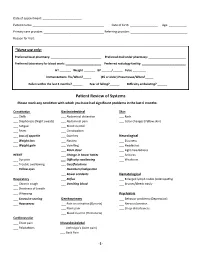
Patient Review of Systems Please Mark Any Condition with Which You Have Had Significant Problems in the Last 6 Months
Date of appointment: ________________________ Patient name: ____________________________________________ Date of birth: _________________ Age: ___________ Primary care provider: _____________________________________ Referring provider: ___________________________________ Reason for Visit: _____________________________________________________________________________________________ *Nurse use only: Preferred local pharmacy: _______________________________ Preferred mail order pharmacy: _______________________ Preferred laboratory for blood work: ______________________ Preferred radiology facility: ___________________________ HT _______ Weight _______ BP ______/______ Pulse ________ Immunizations: Flu/When?_____ (65 or older) Pneumovax/When?_____ Fallen within the last 3 months? ______ Fear of falling?______ Difficulty ambulating? ______ Patient Review of Systems Please mark any condition with which you have had significant problems in the last 6 months: Constitution Gastrointestinal Skin ___ Chills ___ Abdominal distention ___ Rash ___ Diaphoresis (Night sweats) ___ Abdominal pain ___ Color changes (Yellow skin) ___ Fatigue ___ Blood in stool ___ Fever ___ Constipation ___ Loss of appetite ___ Diarrhea Neurological ___ Weight loss ___ Nausea ___ Dizziness ___ Weight gain ___ Vomiting ___ Headaches ___ Black stool ___ Light-headedness HEENT ___ Change in bowel habits ___ Seizures ___ Eye pain ___ Difficulty swallowing ___ Weakness ___ Trouble swallowing ___ Gas/flatulence ___ Yellow eyes ___ Heartburn/indigestion ___ Bowel accidents Hematological -

2019 FMX Gastrointestinal Handouts
2019 FMX Gastrointestinal Handouts Colorectal Cancer Update: Butt Seriously (CME064‐065) Diverticulitis Update (CME066‐067) Gallbladder Disease (CME068‐069) Gastroesophageal Reflux Disease: Evidence‐Based Approach (CME070‐071) Colorectal Cancer Update: Butt Seriously Jason Domagalski, MD, FAAFP ACTIVITY DISCLAIMER The material presented here is being made available by the American Academy of Family Physicians for educational purposes only. Please note that medical information is constantly changing; the information contained in this activity was accurate at the time of publication. This material is not intended to represent the only, nor necessarily best, methods or procedures appropriate for the medical situations discussed. Rather, it is intended to present an approach, view, statement, or opinion of the faculty, which may be helpful to others who face similar situations. The AAFP disclaims any and all liability for injury or other damages resulting to any individual using this material and for all claims that might arise out of the use of the techniques demonstrated therein by such individuals, whether these claims shall be asserted by a physician or any other person. Physicians may care to check specific details such as drug doses and contraindications, etc., in standard sources prior to clinical application. This material might contain recommendations/guidelines developed by other organizations. Please note that although these guidelines might be included, this does not necessarily imply the endorsement by the AAFP. 1 DISCLOSURE It is the policy of the AAFP that all individuals in a position to control content disclose any relationships with commercial interests upon nomination/invitation of participation. Disclosure documents are reviewed for potential conflict of interest (COI), and if identified, conflicts are resolved prior to confirmation of participation. -

Traveller's Diarrhoea (TD) Is the Commonest Health
Diarrhoea • THEME Traveller's diarrhoea BACKGROUND There has been little if any Traveller's diarrhoea (TD) is the commonest health change in the incidence of traveller's diarrhoea problem facing travellers to less developed countries over the past 20 years. of the world. It is costly to both the traveller (time lost) and the host country (eg. cancelled activities). OBJECTIVE This article aims to provide a basic understanding on why travellers are more likely to Definition experience diarrhoea during travel. Classic TD is described as three or more loose bowel DISCUSSION In a 20 minute pretravel actions with at least one of the following accompanying consultation time is precious, and providing symptoms: nausea, vomiting, abdominal cramps or information on traveller's diarrhoea often has pain, fever or blood in the stools. Lesser degrees a low priority over prescribing the necessary vaccinations and discussing antimalarials. (moderate or mild) of TD are also described. Severity is Bob Kass, Travellers do not follow the rules of eating and usually defined by the number of bowel actions per 24 drinking safely, and diarrhoea is common. 'What hour period (severe >6). According to the World Health MBBS, MRCP (UK), MScMCH, Organisation, symptoms lasting less than 14 days may to do in the event of illness' is an important DCH, FAFPHM, consideration. Presumptive treatment should be defined as 'acute diarrhoea', and those lasting more is a consultant, be offered to all travellers whose itinerary and than 14 days 'persistent diarrhoea'.1 International Public activities put them at risk. Between 30 and 50% of travellers will be affected Health Medicine, Rede-Health in a 2 week overseas stay, with approximately 12% International. -

Type 2 Diabetes SCAN Formulary Drugs
Pharmacologic Agents for Treatment of Type 2 Diabetes SCAN Formulary Drugs 2020 2021 Risk for Dosing & Drug- Drug Medication Formulary Formulary Adverse Drug Reactions Administration Interactions Tier UM Tier UM * Biguanides 500 – 850 mg Nausea/ vomiting, GI upset, metallic taste, metformin tabs 1 1 QD - TID diarrhea, flatulence, lactic acidosis (rare) metformin er Neutral 500 – 2000 mg Nausea/ vomiting, GI upset, diarrhea, flatulence, uncoated tabs 1 1 daily lactic acidosis 500 mg & 750 mg Sulfonylureas Dizziness, headache, hypoglycemia, nausea, glimepiride 1 1 1 – 8 mg daily weight gain 2.5 – 20 mg Rash, diarrhea, dizziness, headache, diarrhea, glipizide 1 1 daily Moderate hypoglycemia, nausea, weight gain Asthenia, headache, dizziness, rash, nausea, glipizide er 1 1 5 – 20 mg daily hypoglycemia, weight gain glipizide / 2.5 / 500 mg Rash, diarrhea, dizziness, headache, nausea, 1 1 Moderate metformin tabs BID flatulence, hypoglycemia, lactic acidosis Thiazolidinediones & Thiazolidinedione Combination Agents 15 – 45 mg Anemia, edema, weight gain, headache, myalgia, pioglitazone 1 1 daily bone fracture, heart failure 15 / 500 mg – pioglitazone / Rash, diarrhea, dizziness, headache, nausea, 2 2 45 / 1500mg metformin Neutral flatulence, hypoglycemia, lactic acidosis daily 15 / 500 mg – pioglitazone / Anemia, edema, weight gain, headache, myalgia, 2 [QL] 2 [QL] 45 / 2550 mg glimepiride dizziness, hypoglycemia, nausea daily R. Brower and N. Nguyen rev. 11/2012; R. Brower rev. 11/2013, 9/2014, 11/2015; D. Yoon rev 8/2016, 11/2016, 8/2017; K.