Energy Requirements of Breathing
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
The Structure and Function of Breathing
CHAPTERCONTENTS The structure-function continuum 1 Multiple Influences: biomechanical, biochemical and psychological 1 The structure and Homeostasis and heterostasis 2 OBJECTIVE AND METHODS 4 function of breathing NORMAL BREATHING 5 Respiratory benefits 5 Leon Chaitow The upper airway 5 Dinah Bradley Thenose 5 The oropharynx 13 The larynx 13 Pathological states affecting the airways 13 Normal posture and other structural THE STRUCTURE-FUNCTION considerations 14 Further structural considerations 15 CONTINUUM Kapandji's model 16 Nowhere in the body is the axiom of structure Structural features of breathing 16 governing function more apparent than in its Lung volumes and capacities 19 relation to respiration. This is also a region in Fascla and resplrstory function 20 which prolonged modifications of function - Thoracic spine and ribs 21 Discs 22 such as the inappropriate breathing pattern dis- Structural features of the ribs 22 played during hyperventilation - inevitably intercostal musculature 23 induce structural changes, for example involving Structural features of the sternum 23 Posterior thorax 23 accessory breathing muscles as well as the tho- Palpation landmarks 23 racic articulations. Ultimately, the self-perpetuat- NEURAL REGULATION OF BREATHING 24 ing cycle of functional change creating structural Chemical control of breathing 25 modification leading to reinforced dysfunctional Voluntary control of breathing 25 tendencies can become complete, from The autonomic nervous system 26 whichever direction dysfunction arrives, for Sympathetic division 27 Parasympathetic division 27 example: structural adaptations can prevent NANC system 28 normal breathing function, and abnormal breath- THE MUSCLES OF RESPIRATION 30 ing function ensures continued structural adap- Additional soft tissue influences and tational stresses leading to decompensation. -

Appendix B: Muscles of the Speech Production Mechanism
Appendix B: Muscles of the Speech Production Mechanism I. MUSCLES OF RESPIRATION A. MUSCLES OF INHALATION (muscles that enlarge the thoracic cavity) 1. Diaphragm Attachments: The diaphragm originates in a number of places: the lower tip of the sternum; the first 3 or 4 lumbar vertebrae and the lower borders and inner surfaces of the cartilages of ribs 7 - 12. All fibers insert into a central tendon (aponeurosis of the diaphragm). Function: Contraction of the diaphragm draws the central tendon down and forward, which enlarges the thoracic cavity vertically. It can also elevate to some extent the lower ribs. The diaphragm separates the thoracic and the abdominal cavities. 2. External Intercostals Attachments: The external intercostals run from the lip on the lower border of each rib inferiorly and medially to the upper border of the rib immediately below. Function: These muscles may have several functions. They serve to strengthen the thoracic wall so that it doesn't bulge between the ribs. They provide a checking action to counteract relaxation pressure. Because of the direction of attachment of their fibers, the external intercostals can raise the thoracic cage for inhalation. 3. Pectoralis Major Attachments: This muscle attaches on the anterior surface of the medial half of the clavicle, the sternum and costal cartilages 1-6 or 7. All fibers come together and insert at the greater tubercle of the humerus. Function: Pectoralis major is primarily an abductor of the arm. It can, however, serve as a supplemental (or compensatory) muscle of inhalation, raising the rib cage and sternum. (In other words, breathing by raising and lowering the arms!) It is mentioned here chiefly because it is encountered in the dissection. -

A Review of the Breathing Mechanism for Singing
A Review of the Breathing Mechanism for Singing: Part I: Anatomy Dr. Sean McCarther Breathing is important for singing. In fact, many argue that a properly coordinated breathing mechanism is one of, if not the most important components of a vocal technique. As my former teacher, Dr. Robert Harrison, is fond of saying, “No air, no sound.” It is our responsibility as teachers of singing to help students learn to coordinate the muscles and organs of the breathing mechanism in such a way as to produce the most efficient and vibrant sound. Part I of this series will focus on the anatomy of the breathing mechanism. It will review the major organs, muscles, and bones and discuss how they interact with each other for both passive and active breathing. Part II will examine the singer’s breath in greater detail and discuss various ways the system can be used for singing, including a description of appoggio. The Lungs and Lower Airway The lungs are made of a porous, spongy material that is somewhat elastic in nature (its elasticity is an important part of exhalation, but more on that later). The lungs attach to the ribs via the pleural sacs, two thin pieces of membrane that cause the lungs to adhere to the ribs. Because of this connection, any change in the volume of the rib cage causes a similar change in the volume of the lungs. As the volume of the lungs increase, a vacuum is created, causing air to rush in and fill the lungs. This is called inhalation. -
Unit-3 Mechanism of Respiration
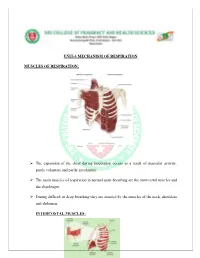
UNIT-3 MECHANISM OF RESPIRATION MUSCLES OF RESPIRATION: The expansion of the chest during inspiration occurs as a result of muscular activity, partly voluntary and partly involuntary. The main muscles of respiration in normal quiet breathing are the intercostal muscles and the diaphragm. During difficult or deep breathing they are assisted by the muscles of the neck, shoulders and abdomen. INTERCOSTAL MUSCLES: There are 11 pairs of intercostal muscles that occupy the spaces between the 12 pairs of ribs. They are arranged in two layers, the external and internal intercostal muscles. The external intercostal muscle fibres - These extend in a downwards and forwards direction from the lower border of the rib above to the upper border of the rib below. The internal intercostal muscle fibres - These extend in a downwards and backwards direction from the lower border of the rib above to the upper border of the rib below, crossing the external intercostal muscle fibres at right angles The first rib is fixed. Therefore, when the intercostal muscles contract they pull all the other ribs towards the first rib. Because of the shape of the ribs they move outwards when pulled upwards. In this way the thoracic cavity is enlarged anterioposteriorly and laterally. The intercostal muscles are stimulated to contract by the intercostal nerves. DIAPHRAGM: The diaphragm is a dome-shaped structure separating the thoracic and abdominal cavities. It forms the floor of the thoracic cavity and the roof of the abdominal cavity Consists of a central tendon from which muscle fibers radiate to be attached to the lower ribs and sternum and to the vertebral column by two crura. -

Muscles of the Spinal Column
Muscles of the Spinal Column Chapter 12 Cervical Muscles Splenius Splenius (capitis and cervicis) • Origin: • Cervicis – spinous process of T3-T6 • Capitis - lower half of ligmentum nuchea & spinous process of C7 and T1-3. • Insertion: • Cervicis - transverse process of C1-C3. • Capitis – mastoid process and occipital bone • Actions: • Whole • Neck Extension • Half • Neck Rotation to the same side. • Lateral flexion of the neck Splenius (cervicis & capitis) Splenius Sternocleidomastoid Sternocleidomastoid • O: Top of the sternum and medial third of the clavical • I: Mastoid process • Action: • Whole • Neck Flexion • Half • Lateral Flexion of the neck • Neck Rotation to the opposite side. Sternocleidomastoid Sternocleidomastoid Scalenus (or scalenes) • O: First two ribs • I: Transverse processes of cervical vertebrae. • Actions: • Whole – Neck Flexion • Half - Lateral Flexion of the neck Scalenus Other Cervical Muscles - FYI • Levator scapulae • Upper fibers of the trapezius • Upper fibers of the rhomboids Lumbar Muscles Erector Spinae Erector spinae muscles • O: Fascia of lower back, posterior L, T and lower C vertebrea, and angles of ribs. • Inesrtions • Spinalis branch - spinous process of T and C and occipital bone • Longissimus branch - transverse process of T and C, mastoid process. • Iliocostalis branch - angles of the ribs and cervical transverse processes • Actions: • Whole – Extension of the spine • Half - Lateral flexion of the spine Erector spinae muscles Erector spinae muscles Iliocostalis branch Longissimus branch Spinalis branch Spinalis branch Longissimus branch Iliocostalis branch Quadratus lumborum • O: Posterior lip of iliac crest • I: Lower border of 12th rib and transverse process of L1-4 • Actions: • Half - Lumbar lateral flexion Quadratus lumborum The Abdominal Muscles 2. 4. 3. 1. -

Multiple Sclerosis and Respiratory Muscle Weakness
AMERICAN PHYSICAL THERAPY ASSOCIATION, SECTION ON NEUROLOGY Multiple Sclerosis and FACT SHEET Respiratory Muscle Weakness Author:s Donna Frym, PT, PhD, CHC and Toni Chiara, PT, PhD Respiratory function is important to keep your body strong Neck and chest wall muscle strength is required to expand the chest wall to allow the lungs to expand when you breathe in. When the lungs fill with air, the blood vessels in the lungs absorb oxygen necessary for your body to function well. If the muscles that expand the chest wall are weak, the lungs cannot expand fully and less oxygen gets into our blood. Abdominal muscle strength is required to achieve a forceful cough necessary to re- move mucus from the lungs when you have a respiratory infection. Also, abdominal muscle strength is needed for loudness and endurance of speech projection. People with multiple sclerosis (MS) rarely complain of respiratory dysfunction, although upon testing respiratory dysfunction is commonly found even in people who have minimal disability. When Should Respiratory Muscle Strength be Tested? If you have MS and experience difficulty breathing, shortness of breath, or have a weak cough on a regular basis, testing of respiratory muscle strength is indicated. How is Respiratory Muscle Strength Tested? Respiratory therapists and physical therapists test respiratory muscle strength and en- durance. Testing is done using a device called a manometer which measures air pres- sure as you breathe into or out of a large tube placed in your mouth. 1111 North Farifax Street Alexandria, VA 22314-1488 Phone: 800-999-2782, Ext 3237 Fax: 703-706-8578 Email: [email protected] www.neuropt.org Image from (http://www.powerbreathe.com/blog/inspiratory-muscle-training-for-strength) Last accessed on 3/24/15 AMERICAN PHYSICAL THERAPY ASSOCIATION, SECTION ON NEUROLOGY Multiple Sclerosis Strength measures: and Respiratory Maximal Inspiratory Pressure (MIP) is a measure of the maximal pressure Muscle Weakness generated in a testing device when breathing in (inspiration). -

Muscles of Respiration I-Clicker Muscles of Inspiration
Muscles of Respiration SHS 300 i-clicker • Anatomy movies –A) integrate into lectures with questions –B) integrate into lectures with bonus questions –C) just show the damn movie so I can sleep Muscles of Inspiration •Diaphragm •Rib cage Elevators –External intercostals and internal intercostal (chondral portion) –Sternocleidomastoid –Levatores costarum or costal elevators –Scalenus group: Anterior, medius and posterior –Pectoralis major and minor –Subclavius –Serratus anterior and serratus posterior superior –Latissimus dorsi 1 Diaphragm ‘Fence in between’ •Thick sheet of muscle that forms floor of thorax –Separates abdomen and thorax •Dome or inverted bowl shape and slightly lower on left •In the center is the central tendon •Lateral muscles attach all around lower rib cage and circumference •Major inhalation muscle Hoit & Hixon, 2005 Diaphragm •Contraction pulls tendon downwards and forwards •Enlarges thorax vertically and circumerentially (elevates lower six ribs) •Increases pressure on abdominal contents •Innervation: Phrenic nerve arising from cervical plexus Diaphragm Origins and Insertions •Origins: • Sternal part: Xiphoid process: posterior surface. •Costal part: Ribs 6 to 12 and their costal cartilages. •Insertion: Central tendon. Hoit & Hixon, 2005 2 Diaphragm Origins and Insertions Lumbar part: 1) Medial and lateral arcuate ligaments; 2) Vertebrae L1 - L3: bodies (via left and right crura). The left crus is a tendinous attachment of the diaphragm and is located on its posterior aspect. It passes to the left side of the aorta and blends with the anterior longitudinal ligament over the vertebrae and discs of L1 to L2. The right crus is a tendinous attachment of the diaphragm located on its posterior aspect. It passes to the right side of the aorta and blends with the anterior longitudinal ligament over the vertebrae and discs of L1 to L3. -

The Therapeutic Basis of Breathing Exercises
THE THERAPEUTIC BASIS OF BREATHING EXERCISES PAUL A. NELSON, M.D. Department of Physical Medicine and Rehabilitation HE value of breathing exercises has not been sufficiently stressed in the Tpast. Most physicians have not been trained to think in terms of prescrip- tion of therapeutic exercise as they have in prescription of drugs or in indica- tions for operative procedures. However, with the introduction of courses of physical medicine and rehabilitation into the curricula of many medical schools, encouraging progress is being made in giving younger physicians a basic un- derstanding of therapeutic exercise. It is hoped that with this new emphasis, greater use will be made by all physicians of such simple yet beneficial pro- cedures as breathing exercises in conditions where they are indicated. Three conditions in which breathing exercises have proved to be of definite value will be discussed. Special consideration will be given to the pathologic physiology present in each instance, particularly in so far as it affects respiration, and to the therapeutic objectives of breathing exercises. The exercises themselves will be outlined briefly in the form that has been found most practical for instruction of patients. Physiology of Normal Respiration. Since the rationale for breathing exercises is based upon physiologic principles, a brief discussion of the physiology of normal respiration is warranted. Respiration in a strictly physiologic sense is the exchange of oxygen and carbon dioxide between living cells and their environment. However, the term respiration usually refers to the movements of inspiration and expiration which provide an intermittent flow of air through the lungs sufficient for the exchange of the respiratory gases. -
Anatomy of the Thoracic Wall, Pulmonary Cavities, and Mediastinum
3 Anatomy of the Thoracic Wall, Pulmonary Cavities, and Mediastinum KENNETH P. ROBERTS, PhD AND ANTHONY J. WEINHAUS, PhD CONTENTS INTRODUCTION OVERVIEW OF THE THORAX BONES OF THE THORACIC WALL MUSCLES OF THE THORACIC WALL NERVES OF THE THORACIC WALL VESSELS OF THE THORACIC WALL THE SUPERIOR MEDIASTINUM THE MIDDLE MEDIASTINUM THE ANTERIOR MEDIASTINUM THE POSTERIOR MEDIASTINUM PLEURA AND LUNGS SURFACE ANATOMY SOURCES 1. INTRODUCTION the thorax and its associated muscles, nerves, and vessels are The thorax is the body cavity, surrounded by the bony rib covered in relationship to respiration. The surface anatomical cage, that contains the heart and lungs, the great vessels, the landmarks that designate deeper anatomical structures and sites esophagus and trachea, the thoracic duct, and the autonomic of access and auscultation are reviewed. The goal of this chapter innervation for these structures. The inferior boundary of the is to provide a complete picture of the thorax and its contents, thoracic cavity is the respiratory diaphragm, which separates with detailed anatomy of thoracic structures excluding the heart. the thoracic and abdominal cavities. Superiorly, the thorax A detailed description of cardiac anatomy is the subject of communicates with the root of the neck and the upper extrem- Chapter 4. ity. The wall of the thorax contains the muscles involved with 2. OVERVIEW OF THE THORAX respiration and those connecting the upper extremity to the axial skeleton. The wall of the thorax is responsible for protecting the Anatomically, the thorax is typically divided into compart- contents of the thoracic cavity and for generating the negative ments; there are two bilateral pulmonary cavities; each contains pressure required for respiration. -

Aerodigestive and Respiratory Changes Post Tracheostomy: a Comprehensive Review Passy-Muir Inc. 1
Aerodigestive and Respiratory Changes Post Tracheostomy: A Comprehensive Review AERO-DIGESTIVE & RESPIRATORY CHANGES POST TRACHEOSTOMY: A COMPREHENSIVE REVIEW Learning Objectives: • Review anatomy & physiology of upper airway (aero-digestive system) • Review anatomy & physiology of lower airway • Un ders tan d the physi ol ogi ic changes to the airway secondary to the tracheotomy, and relate those changes to specific disease processes • Discuss complications of the tracheostomy tube Upper Respiratory Tract • Nasal Cavity Nasal Cavity • Oral Cavity • Pharynx • Larynx Oral Cavity Pharynx Larynx Passy‐Muir Inc. 1 Aerodigestive and Respiratory Changes Post Tracheostomy: A Comprehensive Review Nasal Cavity Velum • Heats, humidifies, Nasal Cavity filters, resonates sound, and olfaction • Velum elevates during the swallow, closes the nasal cavity, and prevents nasal regurgitation Oral Cavity Oral Cavity Primary role is respiration, but is also used for swallow, digestion and speech • Lips – seal oral cavity for swallow •Tongue–oral prep, oral transit (base of tongue is Tongue the primary muscle used to propel food – it rests on hyoid bone) • Salivary Glands –secrete Hyoid Bone lubrication Pharynx – Muscular tube that is duel passageway for respiration and swallow Naso‐ – The 3 segments are: pharynx • Nasopharynx • Oropharynx Oro‐ Pharynx – gag reflex1 – 13% no gag-not predictor of 2 Laryngo‐ dysphagia pharynx • Laryngopharynx – separates digestive and respiratory tracts 1.Leder 1996a 2.Leder 1997 Passy‐Muir Inc. 2 Aerodigestive and Respiratory -

Structural Model of Thorax and Abdomen for Respiratory Mechanics
Mathematical )dodellin¢. Vol. 7. pp. 1083-1098. 1986 0270--0255,86 53.00 ~ .00 Printed in the U.S.A. All rights reser',ed. Copyright ~ I986 Pergamon Journals Ltd. STRUCTURAL MODEL OF THORAX AND ABDOMEN FOR RESPIRATORY MECHANICS STEPHEN H. LOR1NG* Department of Environmental Science and Physiology. Harvard School of Public Health. Boston. Massachusetts 02115, U.S.A. (Received 5 February 1985; revised 23 April 1985) Abstract--This paper describes a structural model of the human rib cage and abdomen that incorporates many geometrical and functional features important to the under- standing of respiratory mechanics. The rib cage, diaphragm, abdominal wall and lungs are characterized by nonlinear stress-strain characteristics that depend on muscle ac- tivity. The positions, volumes, forces and pressures for each set of initial conditions are found by determining mechanical equilibrium. Many such determinations allow pre- dictions for large displacements. The model predicts passive respiratory system be- havior and the action of individual respiratory muscles that are qualitatively consistent with physiological data. Respiratory mechanics includes both pulmonary mechanics and mechanics of the chest wall by which we mean the mechanics of the thorax, the abdomen and the diaphragm. The geometrical complexity of the chest wall and its associated muscles of respiration makes rigorous analysis of the mechanics of the res- piratory system difficut. This paper describes a structural model of the respiratory system with two degrees of freedom of motion that has been useful for understanding the actions of respiratory muscles. The model was initially developed to test the hy- pothesis of Goldman and Mead[l] that the diaphragm, contracting by itself, can expand the abdomen and rib cage in the same way as passive inflation of the respiratory system. -

RESPIRATORY SYSTEM EXAMINATION and EMERGENCY/CRITICAL CARE TECHNIQUES Bernie Hansen DVM MS DACVECC DACVIM (Int. Med) North Carol
RESPIRATORY SYSTEM EXAMINATION AND EMERGENCY/CRITICAL CARE TECHNIQUES Bernie Hansen DVM MS DACVECC DACVIM (Int. Med) North Carolina State University College of Veterinary Medicine Raleigh, NC NORMAL RESPIRATION Respiration requires an integrated system of control (CNS), movement of a bellows (ribs and associated muscle) to draw air into the lungs, exchange of gas within the lung, and a feedback system (chemoreceptors, stretch receptors) to close the loop. This lecture will present some basic elements of the bellows part of this system, providing a basis for evaluation of respiratory patterns in the dog. LUNGS COLLAPSE, RIBS SPRING OUT Lungs are a viscoelastic tissue suspended within the pleural cavity. If the chest is opened to the atmosphere the lungs collapse until small airway occlusion prevents further loss of gas. The collapse won’t stop until the lung volume is quite a bit smaller than the normal functional residual capacity (FRC) in the intact animal. The lung volume in a normal animal is maintained by support from the thoracic wall. Because there is an airtight seal within the pleural space and the lungs are coupled to the chest wall with a viscous fluid, the tendency of the lungs to collapse is countered by the tendency of the ribs to th th spring out. Between breaths, these opposing forces yield a pleural pressure of -5 cm H2O at the 8 -9 interspace in an average size dog. Breathing takes place around this equilibrium, with most of the energy of breathing expended to increase the thoracic volume above the equilibrium point during inspiration. BUCKET HANDLES The ribs in the dog (and cat) are arranged in such a manner that most movement, and the inspiratory effect of that movement, is related to cranial displacement of the ribs during inspiration (Fig 1).