Inducible Knockout of Clec16a in Mice Results in Sensory Neurodegeneration Heather S
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Genome-Scale Single-Cell Mechanical Phenotyping Reveals Disease-Related Genes Involved in Mitotic Rounding
ARTICLE DOI: 10.1038/s41467-017-01147-6 OPEN Genome-scale single-cell mechanical phenotyping reveals disease-related genes involved in mitotic rounding Yusuke Toyoda 1,2, Cedric J. Cattin3, Martin P. Stewart 3,4,5, Ina Poser1, Mirko Theis6, Teymuras V. Kurzchalia1, Frank Buchholz1,6, Anthony A. Hyman1 & Daniel J. Müller 3 To divide, most animal cells drastically change shape and round up against extracellular confinement. Mitotic cells facilitate this process by generating intracellular pressure, which the contractile actomyosin cortex directs into shape. Here, we introduce a genome-scale microcantilever- and RNAi-based approach to phenotype the contribution of > 1000 genes to the rounding of single mitotic cells against confinement. Our screen analyzes the rounding force, pressure and volume of mitotic cells and localizes selected proteins. We identify 49 genes relevant for mitotic rounding, a large portion of which have not previously been linked to mitosis or cell mechanics. Among these, depleting the endoplasmic reticulum-localized protein FAM134A impairs mitotic progression by affecting metaphase plate alignment and pressure generation by delocalizing cortical myosin II. Furthermore, silencing the DJ-1 gene uncovers a link between mitochondria-associated Parkinson’s disease and mitotic pressure. We conclude that mechanical phenotyping is a powerful approach to study the mechanisms governing cell shape. 1 Max Planck Institute of Molecular Cell Biology and Genetics, Pfotenhauerstrasse 108, 01307 Dresden, Germany. 2 Division of Cell Biology, Life Science Institute, Kurume University, Hyakunen-Kohen 1-1, Kurume, Fukuoka 839-0864, Japan. 3 Department of Biosystems Science and Engineering (D-BSSE), Eidgenössische Technische Hochschule (ETH) Zurich, Mattenstrasse 26, 4058 Basel, Switzerland. -

Clec16a, Nrdp1, and USP8 Form a Ubiquitin-Dependent
Page 1 of 46 Diabetes Clec16a, Nrdp1, and USP8 form a ubiquitin-dependent tripartite complex that regulates beta cell mitophagy Gemma Pearson1; Biaoxin Chai1; Tracy Vozheiko1; Xueying Liu1; Malathi Kandarpa2; 3 1,4* Robert C. Piper ; and Scott A. Soleimanpour 1Division of Metabolism, Endocrinology & Diabetes, Department of Internal Medicine, University of Michigan Medical School, Ann Arbor, MI 48105, USA. 2Division of Hematology and Oncology, Department of Internal Medicine, University of Michigan Medical School, Ann Arbor, MI 48105, USA. 3Department of Molecular Physiology and Biophysics, University of Iowa Carver College of Medicine, Iowa City, IA 52242, USA 4Veterans Affairs Ann Arbor Health Care System, Ann Arbor, MI 48105, USA. *Corresponding Author Scott A. Soleimanpour, M.D., 1000 Wall Street, 5317 Brehm Tower, Ann Arbor, MI 48105. Phone: (734) 763-0528 Fax: (734) 232-8162 E-mail: [email protected] Running Title: β-cell mitophagy requires ubiquitin signaling Word Count: 4448 Figures: 7 Diabetes Publish Ahead of Print, published online November 27, 2017 Diabetes Page 2 of 46 ABSTRACT Mitophagy is a cellular quality control pathway, which is essential to eliminate unhealthy mitochondria. While mitophagy is critical to pancreatic β-cell function, the post-translational signals governing β-cell mitochondrial turnover are unknown. Here we report that ubiquitination is essential for the assembly of a mitophagy regulatory complex, comprised of the E3 ligase Nrdp1, the deubiquitinase enzyme USP8, and Clec16a, a mediator of β-cell mitophagy with unclear function. We discover that the diabetes gene Clec16a encodes an E3 ligase, which promotes non-degradative ubiquitin conjugates to direct its mitophagy effectors and stabilize the Clec16a-Nrdp1-USP8 complex. -
Genome-Wide DNA Methylation Dynamics During Epigenetic
Gómez‑Redondo et al. Clin Epigenet (2021) 13:27 https://doi.org/10.1186/s13148‑021‑01003‑x RESEARCH Open Access Genome‑wide DNA methylation dynamics during epigenetic reprogramming in the porcine germline Isabel Gómez‑Redondo1*† , Benjamín Planells1†, Sebastián Cánovas2,3, Elena Ivanova4, Gavin Kelsey4,5 and Alfonso Gutiérrez‑Adán1 Abstract Background: Prior work in mice has shown that some retrotransposed elements remain substantially methylated during DNA methylation reprogramming of germ cells. In the pig, however, information about this process is scarce. The present study was designed to examine the methylation profles of porcine germ cells during the time course of epigenetic reprogramming. Results: Sows were artifcially inseminated, and their fetuses were collected 28, 32, 36, 39, and 42 days later. At each time point, genital ridges were dissected from the mesonephros and germ cells were isolated through magnetic‑ activated cell sorting using an anti‑SSEA‑1 antibody, and recovered germ cells were subjected to whole‑genome bisulphite sequencing. Methylation levels were quantifed using SeqMonk software by performing an unbiased analysis, and persistently methylated regions (PMRs) in each sex were determined to extract those regions showing 50% or more methylation. Most genomic elements underwent a dramatic loss of methylation from day 28 to day 36, when the lowest levels were shown. By day 42, there was evidence for the initiation of genomic re‑methylation. We identifed a total of 1456 and 1122 PMRs in male and female germ cells, respectively, and large numbers of transpos‑ able elements (SINEs, LINEs, and LTRs) were found to be located within these PMRs. Twenty‑one percent of the introns located in these PMRs were found to be the frst introns of a gene, suggesting their regulatory role in the expression of these genes. -

POGLUT1, the Putative Effector Gene Driven by Rs2293370 in Primary
www.nature.com/scientificreports OPEN POGLUT1, the putative efector gene driven by rs2293370 in primary biliary cholangitis susceptibility Received: 6 June 2018 Accepted: 13 November 2018 locus chromosome 3q13.33 Published: xx xx xxxx Yuki Hitomi 1, Kazuko Ueno2,3, Yosuke Kawai1, Nao Nishida4, Kaname Kojima2,3, Minae Kawashima5, Yoshihiro Aiba6, Hitomi Nakamura6, Hiroshi Kouno7, Hirotaka Kouno7, Hajime Ohta7, Kazuhiro Sugi7, Toshiki Nikami7, Tsutomu Yamashita7, Shinji Katsushima 7, Toshiki Komeda7, Keisuke Ario7, Atsushi Naganuma7, Masaaki Shimada7, Noboru Hirashima7, Kaname Yoshizawa7, Fujio Makita7, Kiyoshi Furuta7, Masahiro Kikuchi7, Noriaki Naeshiro7, Hironao Takahashi7, Yutaka Mano7, Haruhiro Yamashita7, Kouki Matsushita7, Seiji Tsunematsu7, Iwao Yabuuchi7, Hideo Nishimura7, Yusuke Shimada7, Kazuhiko Yamauchi7, Tatsuji Komatsu7, Rie Sugimoto7, Hironori Sakai7, Eiji Mita7, Masaharu Koda7, Yoko Nakamura7, Hiroshi Kamitsukasa7, Takeaki Sato7, Makoto Nakamuta7, Naohiko Masaki 7, Hajime Takikawa8, Atsushi Tanaka 8, Hiromasa Ohira9, Mikio Zeniya10, Masanori Abe11, Shuichi Kaneko12, Masao Honda12, Kuniaki Arai12, Teruko Arinaga-Hino13, Etsuko Hashimoto14, Makiko Taniai14, Takeji Umemura 15, Satoru Joshita 15, Kazuhiko Nakao16, Tatsuki Ichikawa16, Hidetaka Shibata16, Akinobu Takaki17, Satoshi Yamagiwa18, Masataka Seike19, Shotaro Sakisaka20, Yasuaki Takeyama 20, Masaru Harada21, Michio Senju21, Osamu Yokosuka22, Tatsuo Kanda 22, Yoshiyuki Ueno 23, Hirotoshi Ebinuma24, Takashi Himoto25, Kazumoto Murata4, Shinji Shimoda26, Shinya Nagaoka6, Seigo Abiru6, Atsumasa Komori6,27, Kiyoshi Migita6,27, Masahiro Ito6,27, Hiroshi Yatsuhashi6,27, Yoshihiko Maehara28, Shinji Uemoto29, Norihiro Kokudo30, Masao Nagasaki2,3,31, Katsushi Tokunaga1 & Minoru Nakamura6,7,27,32 Primary biliary cholangitis (PBC) is a chronic and cholestatic autoimmune liver disease caused by the destruction of intrahepatic small bile ducts. Our previous genome-wide association study (GWAS) identifed six susceptibility loci for PBC. -

Full-Text.Pdf
Systematic Evaluation of Genes and Genetic Variants Associated with Type 1 Diabetes Susceptibility This information is current as Ramesh Ram, Munish Mehta, Quang T. Nguyen, Irma of September 23, 2021. Larma, Bernhard O. Boehm, Flemming Pociot, Patrick Concannon and Grant Morahan J Immunol 2016; 196:3043-3053; Prepublished online 24 February 2016; doi: 10.4049/jimmunol.1502056 Downloaded from http://www.jimmunol.org/content/196/7/3043 Supplementary http://www.jimmunol.org/content/suppl/2016/02/19/jimmunol.150205 Material 6.DCSupplemental http://www.jimmunol.org/ References This article cites 44 articles, 5 of which you can access for free at: http://www.jimmunol.org/content/196/7/3043.full#ref-list-1 Why The JI? Submit online. • Rapid Reviews! 30 days* from submission to initial decision by guest on September 23, 2021 • No Triage! Every submission reviewed by practicing scientists • Fast Publication! 4 weeks from acceptance to publication *average Subscription Information about subscribing to The Journal of Immunology is online at: http://jimmunol.org/subscription Permissions Submit copyright permission requests at: http://www.aai.org/About/Publications/JI/copyright.html Email Alerts Receive free email-alerts when new articles cite this article. Sign up at: http://jimmunol.org/alerts The Journal of Immunology is published twice each month by The American Association of Immunologists, Inc., 1451 Rockville Pike, Suite 650, Rockville, MD 20852 Copyright © 2016 by The American Association of Immunologists, Inc. All rights reserved. Print ISSN: 0022-1767 Online ISSN: 1550-6606. The Journal of Immunology Systematic Evaluation of Genes and Genetic Variants Associated with Type 1 Diabetes Susceptibility Ramesh Ram,*,† Munish Mehta,*,† Quang T. -

A CLEC16A Variant Confers Risk for Juvenile Idiopathic Arthritis and Anti
Concise report Ann Rheum Dis: first published as 10.1136/ard.2009.114934 on 3 September 2009. Downloaded from A CLEC16A variant confers risk for juvenile idiopathic arthritis and anti-cyclic citrullinated peptide antibody negative rheumatoid arthritis Beate Skinningsrud,1,2 Benedicte A Lie,3 Eystein S Husebye,4,5 Tore K Kvien,6 Øystein Førre,7 Berit Flatø,7 Alice Stormyr,1 Geir Joner,8,9 Pål R Njølstad,10,11 Thore Egeland,12,13 Dag E Undlien1,2 ▶ Additional data are published ABSTRACT SNP sets. However, there is extensive linkage online only. To view these fi les Objective Variants in CLEC16A have conferred disequilibrium (LD) between the most strongly please visit the journal online (http://ard.bmj.com). susceptibility to autoimmune diseases in genome- associated SNPs, and a representative subset of wide association studies. The present work aimed to these SNPs was analysed in this study to attempt 1 Department of Medical investigate the locus’ involvements in juvenile idiopathic to ascertain if these associations could point to a Genetics, Oslo University Hospital, Ullevål, Oslo, Norway arthritis (JIA) and further explore the association common SNP, or if the associations in fact rely on 2Institute of Medical Genetics, with rheumatoid arthritis (RA), type 1 diabetes (T1D) different SNPs. University of Oslo, Oslo, Norway and Addison’s disease (AD) in the Norwegian Our aim was to provide further support for 3Institute of Immunology, population. CLEC16A as an autoimmune risk locus and in par- Oslo University Hospital, Methods Three single nucleotide polymorphisms (SNPs) ticular to address the potential role in susceptibility Rikshospitalet, Oslo, Norway 4Section of Endocrinology, were genotyped in patients with RA (n=809), JIA to juvenile idiopathic arthritis (JIA), a disease not Institute of Medicine, University (n=509), T1D (n=1211) and AD (n=414) and in healthy previously studied in this context, as well as to fur- of Bergen, Bergen, Norway controls (n=2149). -

Sji.13050.Pdf
Received: 23 June 2020 | Revised: 20 April 2021 | Accepted: 28 April 2021 DOI: 10.1111/sji.13050 REGULAR ARTICLE Exploring the role of the multiple sclerosis susceptibility gene CLEC16A in T cells Anna M. Eriksson1,2 | Ingvild Sørum Leikfoss1,2,3 | Greger Abrahamsen4 | Vibeke Sundvold4 | Martine Mesel Isom1 | Pankaj K. Keshari1,2 | Torbjørn Rognes5,6 | Ole J. B. Landsverk7 | Steffan D. Bos1,2 | Hanne F. Harbo1,2 | Anne Spurkland4 | Tone Berge3,8 1Department of Neurology, Oslo University Hospital, Oslo, Norway Abstract 2 C- type lectin- like domain family 16 member A CLEC16A Institute of Clinical Medicine, University ( ) is associated with auto- of Oslo, Oslo, Norway immune disorders, including multiple sclerosis (MS), but its functional relevance is 3 Neuroscience Research Unit, Department not completely understood. CLEC16A is expressed in several immune cells, where of Research, Innovation and Education, it affects autophagic processes and receptor expression. Recently, we reported that Oslo University Hospital, Oslo, Norway CLEC16A 4Department of Molecular Medicine, the risk genotype of an MS-associated single nucleotide polymorphism in + Institute of Basic Medical Sciences, intron 19 is associated with higher expression of CLEC16A in CD4 T cells. Here, University of Oslo, Oslo, Norway we show that CLEC16A expression is induced in CD4+ T cells upon T cell activation. 5 Department of Informatics, University of By the use of imaging flow cytometry and confocal microscopy, we demonstrate that Oslo, Oslo, Norway 6 CLEC16A is located in Rab4a- positive recycling endosomes in Jurkat TAg T cells. Department of Microbiology, Oslo University Hospital, Oslo, Norway CLEC16A knock-down in Jurkat cells resulted in lower cell surface expression of 7Department of Pathology, Oslo University the T cell receptor, however, this did not have a major impact on T cell activation Hospital, Oslo, Norway response in vitro in Jurkat nor in human, primary CD4+ T cells. -

CLEC16A Regulates Splenocyte and NK Cell Function in Part Through MEK Signaling
RESEARCH ARTICLE CLEC16A regulates splenocyte and NK cell function in part through MEK signaling 1☯ 1☯ 1 1 Rahul Pandey , Marina Bakay , Heather S. HainID , Bryan Strenkowski , Barakat Z. 2 3 4 5 B. Elsaqa , Jeffrey D. RoizenID , Jake A. Kushner , Jordan S. Orange , 1,6 Hakon HakonarsonID * 1 The Center for Applied Genomics, The Children's Hospital of Philadelphia, Philadelphia, PA, United States of America, 2 Department of Medicine, Jordan University of Science and Technology, Irbid, Jordan, 3 Division of Endocrinology and Diabetes Children's Hospital of Philadelphia, Philadelphia, PA, United States of America, 4 Section of Pediatric Diabetes and Endocrinology, Department of Pediatric Medicine, Endocrine- Metabolism, Texas Children's Hospital, Houston, TX, United States of America, 5 Section of Immunology, a1111111111 Allergy, and Rheumatology, Department of Pediatric Medicine, Texas Children's Hospital, Houston, TX, a1111111111 United States of America, 6 Department of Pediatrics, the Perelman School of Medicine, University of a1111111111 Pennsylvania, Philadelphia, PA, United States of America a1111111111 a1111111111 ☯ These authors contributed equally to this work. * [email protected] Abstract OPEN ACCESS CLEC16A is implicated in multiple autoimmune diseases. We generated Clec16a inducible Citation: Pandey R, Bakay M, Hain HS, knockout (KO) mice to examine the functional link between CLEC16A auto-inflammation Strenkowski B, Elsaqa BZB, Roizen JD, et al. (2018) CLEC16A regulates splenocyte and NK cell and autoimmunity. Clec16a KO mice exhibited weight loss and thymic and splenic atrophy. function in part through MEK signaling. PLoS ONE Mitochondrial potential was lowered in KO mice splenocytes resulting in aggregation of 13(9): e0203952. https://doi.org/10.1371/journal. -

Schizophrenia-Associated Differential DNA Methylation in the Superior Temporal
medRxiv preprint doi: https://doi.org/10.1101/2020.08.02.20166777; this version posted August 4, 2020. The copyright holder for this preprint (which was not certified by peer review) is the author/funder, who has granted medRxiv a license to display the preprint in perpetuity. It is made available under a CC-BY-NC-ND 4.0 International license . Schizophrenia-associated differential DNA methylation in the superior temporal gyrus is distributed to many sites across the genome and annotated by the risk gene MAD1L1 Brandon C. McKinney1,, Christopher M. Hensler4, Yue Wei2, David A. Lewis1,4, Jiebiao Wang2, Ying Ding2, Robert A. Sweet1,3,4. University of Pittsburgh Departments of 1Psychiatry, 2Biostatistics, 3Neurology, and 4Translational Neuroscience Program, Pittsburgh, PA For questions and correspondence, please contact Brandon C. McKinney, MD, PhD. Mail: Biomedical Science Tower, Room W-1658 3811 O’Hara Street, Pittsburgh, PA 15213-2593 Express Mail: Biomedical Science Tower, Room W-1658 Lothrop and Terrace Streets, Pittsburgh, PA 15213-2593 Word Count Abstract: 246 Body: 3170 NOTE: This preprint reports new research that has not been certified by peer review and should not be used to guide clinical practice. medRxiv preprint doi: https://doi.org/10.1101/2020.08.02.20166777; this version posted August 4, 2020. The copyright holder for this preprint (which was not certified by peer review) is the author/funder, who has granted medRxiv a license to display the preprint in perpetuity. It is made available under a CC-BY-NC-ND 4.0 International license . ABSTRACT: Background: Many genetic variants and multiple environmental factors increase risk for schizophrenia (SZ). -

NIH Public Access Author Manuscript Nat Genet
NIH Public Access Author Manuscript Nat Genet. Author manuscript; available in PMC 2014 February 01. NIH-PA Author ManuscriptPublished NIH-PA Author Manuscript in final edited NIH-PA Author Manuscript form as: Nat Genet. 2013 August ; 45(8): 907–911. doi:10.1038/ng.2686. A genome-wide association meta-analysis of self-reported allergy identifies shared and allergy-specific susceptibility loci David A. Hinds1, George McMahon2, Amy K. Kiefer1, Chuong B. Do1, Nicholas Eriksson1, David M. Evans2, Beate St Pourcain3, Susan M. Ring3, Joanna L. Mountain1, Uta Francke1, George Davey-Smith2, Nicholas J. Timpson2,*, and Joyce Y. Tung1,* 123andMe, Inc., Mountain View, CA 94043, USA 2Medical Research Council (MRC) Centre for Causal Analyses in Translational Epidemiology, School of Social and Community Medicine, University of Bristol, Bristol, United Kingdom 3School of Social and Community Medicine, University of Bristol, Bristol, United Kingdom Allergic disease is very common and carries substantial public health burdens. We conducted a meta-analysis of genome-wide association with self-reported cat, dust-mite, and pollen allergy in 53,862 individuals. We used generalized estimating equations to model shared and allergy-specific genetic effects. We identified 16 shared susceptibility loci with P<5×10−8, including 8 loci previously associated with asthma, as well as 4p14 near TLR1, TLR6, and TLR10 (rs2101521: P=5.3×−21); 6p21.33 near HLA-C and MICA (rs9266772: P=3.2×10−12); 5p13.1 near PTGER4 (rs7720838: P=8.2×10−11); 2q33.1 in PLCL1 (rs10497813: P=6.1×10−10); 3q28 in LPP (rs9860547: P=1.2×10−9); 20q13.2 in NFATC2 (rs6021270: P=6.9×10−9); 4q27 in ADAD1 (rs17388568: P=3.9×10−8); and 14q21.1 near FOXA1 and TTC6 (rs1998359: P=4.8×10−8). -
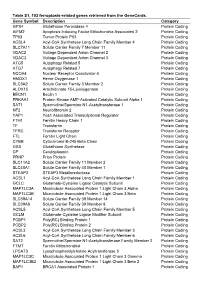
Table S1. 103 Ferroptosis-Related Genes Retrieved from the Genecards
Table S1. 103 ferroptosis-related genes retrieved from the GeneCards. Gene Symbol Description Category GPX4 Glutathione Peroxidase 4 Protein Coding AIFM2 Apoptosis Inducing Factor Mitochondria Associated 2 Protein Coding TP53 Tumor Protein P53 Protein Coding ACSL4 Acyl-CoA Synthetase Long Chain Family Member 4 Protein Coding SLC7A11 Solute Carrier Family 7 Member 11 Protein Coding VDAC2 Voltage Dependent Anion Channel 2 Protein Coding VDAC3 Voltage Dependent Anion Channel 3 Protein Coding ATG5 Autophagy Related 5 Protein Coding ATG7 Autophagy Related 7 Protein Coding NCOA4 Nuclear Receptor Coactivator 4 Protein Coding HMOX1 Heme Oxygenase 1 Protein Coding SLC3A2 Solute Carrier Family 3 Member 2 Protein Coding ALOX15 Arachidonate 15-Lipoxygenase Protein Coding BECN1 Beclin 1 Protein Coding PRKAA1 Protein Kinase AMP-Activated Catalytic Subunit Alpha 1 Protein Coding SAT1 Spermidine/Spermine N1-Acetyltransferase 1 Protein Coding NF2 Neurofibromin 2 Protein Coding YAP1 Yes1 Associated Transcriptional Regulator Protein Coding FTH1 Ferritin Heavy Chain 1 Protein Coding TF Transferrin Protein Coding TFRC Transferrin Receptor Protein Coding FTL Ferritin Light Chain Protein Coding CYBB Cytochrome B-245 Beta Chain Protein Coding GSS Glutathione Synthetase Protein Coding CP Ceruloplasmin Protein Coding PRNP Prion Protein Protein Coding SLC11A2 Solute Carrier Family 11 Member 2 Protein Coding SLC40A1 Solute Carrier Family 40 Member 1 Protein Coding STEAP3 STEAP3 Metalloreductase Protein Coding ACSL1 Acyl-CoA Synthetase Long Chain Family Member 1 Protein -

Clarifying the Function of Genes at the Chromosome 16P13 Locus in Type 1 Diabetes: CLEC16A and DEXI
Genes & Immunity (2020) 21:79–82 https://doi.org/10.1038/s41435-019-0087-7 EDITORIAL Clarifying the function of genes at the chromosome 16p13 locus in type 1 diabetes: CLEC16A and DEXI 1 1 1,2 Morgan A. Gingerich ● Vaibhav Sidarala ● Scott A. Soleimanpour Received: 1 September 2019 / Revised: 9 September 2019 / Accepted: 18 September 2019 / Published online: 1 October 2019 © The Author(s), under exclusive licence to Springer Nature Limited 2019 Abstract More than a decade after the discovery of a novel type 1 diabetes risk locus on chromosome 16p13, there remains complexity and controversy over the specific gene(s) that regulate diabetes pathogenesis. A new study by Nieves-Bonilla et al. shows that one of these genes, DEXI, is unlikely to contribute to type 1 diabetes pathogenesis and positions the endolysosomal E3 ubiquitin ligase CLEC16A as the primary culprit by which this gene locus influences diabetes risk. Type 1 diabetes (T1D) is characterized by the destruction of for half of the genetic predisposition to T1D suggesting the 1234567890();,: 1234567890();,: insulin-producing pancreatic β cells by infiltrating cells of existence of other genetic determinants that remain unex- the immune system. Although the precise mechanisms plored. Over a decade ago, a Wellcome Trust Case Control underlying this disease remain elusive, it has become evi- Consortium study of ~2000 patients with T1D to identify dent that T1D is a complex polygenic disease with both novel genetic risk alleles identified several new regions of genetic and environmental components owing to defects in interest to T1D, including at chromosome 16p13 [4]. This the immune system, the gut microbiome, and pancreatic β was later confirmed by several other T1D cohorts [5, 6], cells [1–3].