Issue 4 | March 2020
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Challenges Affecting Zanzibar Revenue Board Effectiveness on Tax Collection: an Evaluative Study
IOSR Journal of Economics and Finance (IOSR-JEF) e-ISSN: 2321-5933, p-ISSN: 2321-5925. Volume 12, Issue 2 Ser. IV (Mar. –Apr. 2021), PP 32-38 www.iosrjournals.org Challenges Affecting Zanzibar Revenue Board Effectiveness on Tax Collection: An Evaluative Study. Ali Haji Pandu MBA Student, Zanzibar University Dr. Abdalla Ussi Hamad Head, Department of Economics, Zanzibar University Dr. Salama Yussuf Senior Lecturer, Faculty of Business Administration, Zanzibar University Abstract The main objective of this study was to evaluate the challenges affecting Zanzibar revenue board effectiveness on tax collection. The researcher has employed quantitative approach. Simple random sampling was used to select 41 Respondents. The data were collected through closed ended questionnaires. The findings of the study revealed that, over 50 percent agreed and strongly agreed bureaucracy in paying taxes, complex tax computation, unfriendly tax administration, multiple taxes and ineffective tax collection as the major challenges affecting ZRB on tax collection. Finally the study recommends that the Government of Zanzibar has to take intentionally measures to widen their tax base thereby reducing tax avoidance. For example, it is recommended to issues identification number or social security number, to keep track of their transactions. Key terms: Tax collection, Zanzibar Revenue Board, bureaucracy, Descriptive techniques. --------------------------------------------------------------------------------------------------------------------------------------- Date -

Managing Change at Universities. Volume
Frank Schröder (Hg.) Schröder Frank Managing Change at Universities Volume III edited by Bassey Edem Antia, Peter Mayer, Marc Wilde 4 Higher Education in Africa and Southeast Asia Managing Change at Universities Volume III edited by Bassey Edem Antia, Peter Mayer, Marc Wilde Managing Change at Universities Volume III edited by Bassey Edem Antia, Peter Mayer, Marc Wilde SUPPORTED BY Osnabrück University of Applied Sciences, 2019 Terms of use: Postfach 1940, 49009 Osnabrück This document is made available under a CC BY Licence (Attribution). For more Information see: www.hs-osnabrueck.de https://creativecommons.org/licenses/by/4.0 www.international-deans-course.org [email protected] Concept: wbv Media GmbH & Co. KG, Bielefeld wbv.de Printed in Germany Cover: istockphoto/Pavel_R Order number: 6004703 ISBN: 978-3-7639-6033-0 (Print) DOI: 10.3278/6004703w Inhalt Preface ............................................................. 7 Marc Wilde and Tobias Wolf Innovative, Dynamic and Cooperative – 10 years of the International Deans’ Course Africa/Southeast Asia .......................................... 9 Bassey E. Antia The International Deans’ Course (Africa): Responding to the Challenges and Opportunities of Expansion in the African University Landscape ............. 17 Bello Mukhtar Developing a Research Management Strategy for the Faculty of Engineering, Ahmadu Bello University, Zaria, Nigeria ................................. 31 Johnny Ogunji Developing Sustainable Research Structure and Culture in Alex Ekwueme Federal University, Ndufu Alike Ebonyi State Nigeria ....................... 47 Joseph Sungau A Strategy to Promote Research and Consultancy Assignments in the Faculty .. 59 Enitome Bafor Introduction of an annual research day program in the Faculty of Pharmacy, University of Benin, Nigeria ........................................... 79 Gratien G. Atindogbe Research management in Cameroon Higher Education: Data sharing and reuse as an asset to quality assurance ................................... -
Unai Members List August 2021
UNAI MEMBER LIST Updated 27 August 2021 COUNTRY NAME OF SCHOOL REGION Afghanistan Kateb University Asia and the Pacific Afghanistan Spinghar University Asia and the Pacific Albania Academy of Arts Europe and CIS Albania Epoka University Europe and CIS Albania Polytechnic University of Tirana Europe and CIS Algeria Centre Universitaire d'El Tarf Arab States Algeria Université 8 Mai 1945 Guelma Arab States Algeria Université Ferhat Abbas Arab States Algeria University of Mohamed Boudiaf M’Sila Arab States Antigua and Barbuda American University of Antigua College of Medicine Americas Argentina Facultad de Ciencias Económicas de la Universidad de Buenos Aires Americas Argentina Facultad Regional Buenos Aires Americas Argentina Universidad Abierta Interamericana Americas Argentina Universidad Argentina de la Empresa Americas Argentina Universidad Católica de Salta Americas Argentina Universidad de Congreso Americas Argentina Universidad de La Punta Americas Argentina Universidad del CEMA Americas Argentina Universidad del Salvador Americas Argentina Universidad Nacional de Avellaneda Americas Argentina Universidad Nacional de Cordoba Americas Argentina Universidad Nacional de Cuyo Americas Argentina Universidad Nacional de Jujuy Americas Argentina Universidad Nacional de la Pampa Americas Argentina Universidad Nacional de Mar del Plata Americas Argentina Universidad Nacional de Quilmes Americas Argentina Universidad Nacional de Rosario Americas Argentina Universidad Nacional de Santiago del Estero Americas Argentina Universidad Nacional de -

Swiss Spirit Hotel & Suites Alisa, Accra, Ghana
Pedagogical Leadership in Africa/MRPP Concept Note on Pedagogical Leadership in Africa (PedaL)/ Collaborative Master of Research and Public Policy (MRPP) University of Ghana, Western Hub Training Swiss Spirit Hotel & Suites Alisa, Accra, Ghana July 31 to August 8, 2019 1. Background Since its inception in August 2018, the Pedagogical Leadership in Africa (PedaL) training programme has grown phenomenally. The programme has been mainstreamed in a number of university graduate programmes particularly the Master of Research and Public Policy (MRPP) programme offered by 141 universities in 8 African countries. The synergy created with MRPP universities has facilitated engagement with other universities within the host countries and broadened the scope for uptake of pedagogical innovations. 1.1 Partnership for Pedagogical Leadership in Africa (PedaL) The Partnership for Pedagogical Leadership in Africa (PedaL) is a formal partnership of eight institutions that aims to embed and catalyse systemic change in teaching and learning practices and to maximize learning outcomes through strategic interventions in graduate social science programmes. PedaL is one of nine partnerships supported by the Strategic Partnerships for Higher Education Innovation and Reform (SPHEIR) grant scheme to catalyse systemic change in teaching and learning in African universities. SPHEIR partnerships seek to transform the quality, relevance, access and affordability of higher education to achieve sustainable, systemic change. SPHEIR has been established by the UK Department for International Development (DFID) to deliver systemic and sustainable change within higher education systems, enabling them to meet labour market needs and generate the job-ready, entrepreneurial graduates needed to accelerate development, build inclusive societies and promote strong economic growth. -

African Dialogue Facebook: Biographies of Participants
AFRICAN DIALOGUE FACEBOOK: BIOGRAPHIES OF PARTICIPANTS The Sixth Annual African Consumer Protection Dialogue Conference: Strengthening the Framework for Dealing with Cross Border Consumer Violations 8-10 September, 2014 Lilongwe, Malawi Sponsored by: THE COMESA COMPETITION COMMISSION, THE MALAWI COMPETITION AND FAIR TRADING COMMISSION AND THE U.S. FEDERAL TRADE COMMISSION 1 Common Market for Eastern and Southern Africa (COMESA) George K. Lipimile Director and Chief Executive Officer COMESA Competition Commission George K Lipimile is the current Director and Chief Executive Officer of the COMESA Competition Commission. Prior to his current appointment, he served as Senior Advisor at the United Nations Conference on Trade and Development (UNCTAD) in the Division of Competition and Consumer Law Policy. At UNCTAD he was in charge of the technical assistance and capacity building programmes in the area of competition and consumer policies for the developing and least developed countries. Mr. Lipimile established and became the first Executive Director of the Zambia Competition Commission in Zambia (the first modern competition Authority in the Eastern and Southern African Region). His duties included advising the government on a range of trade and competition issues, including the negotiations of the Doha Rounds, WTO Agreements, EPAs negotiations, in addition to issues relating to the regional trade and economic integration of the SADC/COMESA Agreements. For a long time, Mr. Lipimile served as the head of Zambia Intellectual Property office. He was the Chairperson of the African Regional Intellectual Property Organization (ARIPO) for two terms. He sits on several boards of research and academic institutions. Mr. Lipmile is highly consulted on issues pertaining to the enforcement of competition and consumer law and policy. -

University of Ghana, Legon
University of Ghana http://ugspace.ug.edu.gh UNIVERSITY OF GHANA, LEGON COLLEGE OF EDUCATION” SCHOOL OF INFORMATION AND COMMUNICATION STUDIES” DEPARTMENT OF INFORMATION STUDIES” THE USE OF ELECTRONIC RESOURCES BY” GRADUATE “STUDENTS OF UNIVERSITY OF GHANA” BY: HORATIA OBIOKOR AMOO (10404141) THIS DISSERTATION IS SUBMITTED TO THE “UNIVERSITY OF GHANA, LEGON, IN” PARTIAL FULFILMENT “OF THE” REQUIREMENTS “FOR THE AWARD OF MA INFORMATION STUDIES DEGREE.” “JULY”, 2018. University of Ghana http://ugspace.ug.edu.gh “DECLARATION” I, hereby, declare that except “for references to other” works “which have been” duly “acknowledged, this dissertation is the result of my own original work” under the supervision of Prof. Ellis Badu of the “Department of Information Studies, University of Ghana, Legon, and that” no part of “it has been” presented “for another degree” in this university or elsewhere. I accept responsibility for any shortcomings of this work. Signature ………………. Date ………………… Horatia Obiokor Amoo (Student) Signature ………………. Date ……………… Prof. Ellis Badu (Supervisor) i University of Ghana http://ugspace.ug.edu.gh “DEDICATION” This dissertation is dedicated to my father and mentor, Mr. Jonathan Nii Amoo Onukpa, my family, friends, well-wishers and to all lecturers at the Department of Information studies for their immense contribution towards the completion of this work. ii University of Ghana http://ugspace.ug.edu.gh ACKNOWLEDGEMENT ”What shall I render to my God for all His mercy‟s store? I‟ll take the gifts He” has “bestowed, and humbly ask for more”. Foremost, my sincere gratitude is to God Almighty for this rare opportunity and for how far He has brought me. -

Prospectus 2020/2021
PROSPECTUS 2020/2021 The Open University of Tanzania Kawawa Road, Kinondoni Municipality, P.O. Box 23409, Tel: +255 (0)22 2668960/+255 (0)22 2668992 Fax: +255 (0)22 2668759 E-mail: [email protected] [email protected] [email protected] [email protected] Website: http//www.out.ac.tz DAR ES SALAAM, TANZANIA PROSPECTUS 2020/2021 © The Open University of Tanzania, 2020 Published by the Office of the Deputy Vice Chancellor (Academic) Tel: +255 22 2668820 E-mail: [email protected] ii CONTENTS PRINCIPAL ADDRESSES OF THE UNIVERSITY .............................................................. iv SENIOR OFFICERS OF THE OPEN UNIVERSITY OF TANZANIA ................................... 1 DIRECTORS OF REGIONAL/COORDINATION CENTRES................................................ 2 INTRODUCTION TO THE OPEN UNIVERSITY OF TANZANIA ...................................... 3 ACADEMIC PROGRAMMES OFFERED BY THE UNIVERSITY ...................................... 4 ADMISSION REGULATIONS ............................................... Error! Bookmark not defined. GENERAL UNIVERSITY EXAMINATION REGULATIONS FOR UNDERGRADUATE COURSES ................................................................................................................................ 33 DIRECTORATE OF POSTGRADUATE STUDIES .............................................................. 50 GENERAL REGULATIONS AND GUIDELINES FOR HIGHER DEGREES AT THE OPEN UNIVERSITY OF TANZANIA ................................................................................ 50 DIRECTORATE OF RESEARCH AND PUBLICATIONS.................................................. -

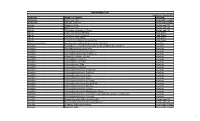
Tanzania Commission for Universities
Tanzania Commission for Universities List of Approved University Institutions in Tanzania as of 4th February, 2019 Tanzania Commission for Universities List of Approved University Institutions in Tanzania as of 4th February, 2019 1: FULLY FLEDGED UNIVERSITIES 1A: Public Universities Approved SN Name of the University Head Office Current Status Acronym 1. University of Dar es Salaam UDSM Dar es Salaam Accredited and Chartered 2. Sokoine University of Agriculture SUA Morogoro Accredited and Chartered 3. Open University of Tanzania OUT Dar es Salaam Accredited and Chartered 4. Ardhi University ARU Dar es Salaam Accredited and Chartered Certificate of Full 5. State University of Zanzibar SUZA Zanzibar Registration (CFR) 6. Mzumbe University MU Morogoro Accredited and Chartered Muhimbili University of Health & 7. MUHAS Dar es Salaam Accredited and Chartered Allied Sciences Certificate of Full Nelson Mandela African Institute of 8. NMAIST Arusha Registration (CFR) and Science and Technology Chartered Certificate of Full 9. University of Dodoma UDOM Dodoma Registration (CFR) and Chartered Certificate of Full Mbeya University of Science and 10. MUST Mbeya Registration (CFR) and Technology Chartered Certificate of Full 11. Moshi Cooperative University MoCU Moshi Registration (CFR) and Chartered Mwalimu Julius K. Nyerere University 12. MJNUAT Musoma Provisional Licence1 of Agriculture and Technology 1 1B: Private Universities Approved SN Name of the University Head Office Current Status Acronym 1. Hubert Kairuki Memorial University HKMU Dar es Salaam Accredited and Chartered International Medical and Certificate of Full Registration 2. Technological University and IMTU Dar es Salaam (CFR) and Chartered Chartered 3. Tumaini University Makumira TUMA Arusha Accredited and Chartered 4. St. -

STRENGTHENING the CHILD PROTECTION SYSTEM to END VIOLENCE AGAINST CHILDREN in EASTERN and SOUTHERN AFRICA Credit for Cover Photo: © UNICEF/UNI361764/Sobecki
STRENGTHENING THE CHILD PROTECTION SYSTEM TO END VIOLENCE AGAINST CHILDREN IN EASTERN AND SOUTHERN AFRICA Credit for cover photo: © UNICEF/UNI361764/Sobecki Acknowledgements The UNICEF Eastern and Southern Africa Regional Office (ESARO) commissioned Child Frontiers to develop a compendium of promising practices on ending harmful practices and violence against children across the region. This documentation was written by Emily Delap of Child Frontiers with significant contributions from UNICEF Ethiopia, Kenya, Madagascar, Rwanda, Somalia, South Africa, South Sudan, Tanzania, Uganda, and Zambia country office staff. Thanks also go to the ESARO child protection team for their inputs under the leadership of Jean Francois Basse and Mona Aika. The publication was designed by hopeworks. May 2021 Summary What is a child protection system? COMPONENTS GOALS • Legal and regulatory framework End all forms of violence against Effective governance structures, x • children including coordination mechanisms • Prevention and response services • Physical violence and injury • Minimum standards and oversight • Mental / emotional violence • Human, financial and infrastructure • Sexual violence resources • Abuse • Mechanisms for child participation and Neglect community engagement • Exploitation • Data collection and monitoring • x Ensure that children grow-up in caring and nurturing families Why take a system strengthening approach to child protection? • To be able to respond to all the forms of violence that children experience. • To ensure the engagement -

STRENGTHENING UNIVERSITY-INDUSTRY LINKAGES in AFRICA a Study on Institutional Capacities and Gaps
STRENGTHENING UNIVERSITY-INDUSTRY LINKAGES IN AFRICA A Study on Institutional Capacities and Gaps JOHN SSEBUWUFU, TERALYNN LUDWICK AND MARGAUX BÉLAND Funded by the Canadian Government through CIDA Canadian International Agence canadienne de Development Agency développement international STRENGTHENING UNIVERSITY-INDUSTRY LINKAGES IN AFRICA: A Study on Institutional Capacities and Gaps Prof. John Ssebuwufu Director, Research & Programmes Association of African Universities (AAU) Teralynn Ludwick Research Officer AAU Research and Programmes Department / AUCC Partnership Programmes Margaux Béland Director, Partnership Programmes Association of Universities and Colleges of Canada (AUCC) Currently on secondment to the Canadian Bureau for International Education (CBIE) Strengthening University-Industry Linkages in Africa: A Study of Institutional Capacities and Gaps @ 2012 Association of African Universities (AAU) All rights reserved Printed in Ghana Association of African Universities (AAU) 11 Aviation Road Extension P.O. Box 5744 Accra-North Ghana Tel: +233 (0) 302 774495/761588 Fax: +233 (0) 302 774821 Email: [email protected], [email protected] Web site: http://www.aau.org This study was undertaken by the Association of African Universities (AAU) and the Association of Universities and Colleges of Canada (AUCC) as part of the project, Strengthening Higher Education Stakeholder Relations in Africa (SHESRA). The project is generously funded by Government of Canada through the Canadian International Development Agency (CIDA). The views and opinions -

Widening Participation in Higher Education in Ghana and Tanzania: Developing an Equity Scorecard
Widening Participation in Higher Education in Ghana and Tanzania: Developing an Equity Scorecard An ESRC/DfID Poverty Reduction Programme funded Research Project Working Paper 1: Setting the Scene Louise Morley Fiona Leach Rosemary Lugg Amandina Lihamba James Opare Eustella Bhalalusesa Linda Dzama Forde Godwin Egbenya Rosemarie Mwaipopo March 2007 www.sussex.ac.uk/education/wideningparticipation WPHE Working Paper 1 Table of Contents List of Acronyms ...........................................................................................................4 1. Setting the Scene for the ESRC/DFID Project on Widening Participation in Higher Education in Ghana and Tanzania ...............................................6 1.1 Aims...................................................................................................................6 1.2 Objectives ..........................................................................................................7 1.3 Research Questions............................................................................................8 1.4 The Equity Scorecard.........................................................................................9 1.5 Why This Research is Important......................................................................10 1.6 Which Groups are Under-represented?............................................................12 1.7 Policy Interventions .........................................................................................14 1.8 Higher Education and Poverty -

ARDI Participating Academic Institutions
ARDI Participating Academic Institutions Filter Summary Country City Institution Name Afghanistan Charikar Parwan University Cheghcharan Ghor Institute of Higher Education Gardez Paktia University Ghazni Ghazni University Jalalabad Nangarhar University Kabul Social and Health Development Program (SHDP) Emergency NGO - Afghanistan French Medical Institute for children, FMIC American University of Afghanistan Kabul Polytechnic University Kateb University Afghan Evaluation Society Prof. Ghazanfar Institute of Health Sciences Information and Communication Technology Institute (ICTI) Kabul Medical University 19-Dec-2017 3:15 PM Prepared by Payment, HINARI Page 1 of 80 Country City Institution Name Afghanistan Kabul Ministry of Public Health , Surveillance Department Kandahar Kandahar University Kapisa Alberoni University Lashkar Gah Helmand University Sheberghan Jawzjan university Albania Tirana Agricultural University of Tirana University of Tirana. Faculty of Natural Sciences Tirane, Albania Albanian Centre for Sustainable Development Algeria Alger Institut National Algerien de La Propriete Industrielle (INAPI) ouargla pépinière d'entreprises incubateur ouargla Tebessa Université Larbi Tébessi (University of Tebessa) 19-Dec-2017 3:15 PM Prepared by Payment, HINARI Page 2 of 80 Country City Institution Name Angola Luanda Instituto Superior Politécnico de Tecnologia e Ciências, ISPTEC Instituto oftalmológico nacional de Angola Instituto Nacional de Recursos Hídricos (INRH) Angolan Institute of Industrial Property MALANJE INSTITUTO SUPERIOR