Care Choices Reference Guide
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Who Pays Soundexchange: Q1 - Q3 2017
Payments received through 09/30/2017 Who Pays SoundExchange: Q1 - Q3 2017 Entity Name License Type ACTIVAIRE.COM BES AMBIANCERADIO.COM BES AURA MULTIMEDIA CORPORATION BES CLOUDCOVERMUSIC.COM BES COROHEALTH.COM BES CUSTOMCHANNELS.NET (BES) BES DMX MUSIC BES ELEVATEDMUSICSERVICES.COM BES GRAYV.COM BES INSTOREAUDIONETWORK.COM BES IT'S NEVER 2 LATE BES JUKEBOXY BES MANAGEDMEDIA.COM BES MEDIATRENDS.BIZ BES MIXHITS.COM BES MTI Digital Inc - MTIDIGITAL.BIZ BES MUSIC CHOICE BES MUSIC MAESTRO BES MUZAK.COM BES PRIVATE LABEL RADIO BES RFC MEDIA - BES BES RISE RADIO BES ROCKBOT, INC. BES SIRIUS XM RADIO, INC BES SOUND-MACHINE.COM BES STARTLE INTERNATIONAL INC. BES Stingray Business BES Stingray Music USA BES STORESTREAMS.COM BES STUDIOSTREAM.COM BES TARGET MEDIA CENTRAL INC BES Thales InFlyt Experience BES UMIXMEDIA.COM BES SIRIUS XM RADIO, INC CABSAT Stingray Music USA CABSAT MUSIC CHOICE PES MUZAK.COM PES SIRIUS XM RADIO, INC SDARS 181.FM Webcasting 3ABNRADIO (Christian Music) Webcasting 3ABNRADIO (Religious) Webcasting 8TRACKS.COM Webcasting 903 NETWORK RADIO Webcasting A-1 COMMUNICATIONS Webcasting ABERCROMBIE.COM Webcasting ABUNDANT RADIO Webcasting ACAVILLE.COM Webcasting *SoundExchange accepts and distributes payments without confirming eligibility or compliance under Sections 112 or 114 of the Copyright Act, and it does not waive the rights of artists or copyright owners that receive such payments. Payments received through 09/30/2017 ACCURADIO.COM Webcasting ACRN.COM Webcasting AD ASTRA RADIO Webcasting ADAMS RADIO GROUP Webcasting ADDICTEDTORADIO.COM Webcasting ADORATION Webcasting AGM BAKERSFIELD Webcasting AGM CALIFORNIA - SAN LUIS OBISPO Webcasting AGM NEVADA, LLC Webcasting AGM SANTA MARIA, L.P. -

American Old-Time Musics, Heritage, Place A
THE UNIVERSITY OF CHICAGO SOUNDS OF THE MODERN BACKWOODS: AMERICAN OLD-TIME MUSICS, HERITAGE, PLACE A DISSERTATION SUBMITTED TO THE FACULTY OF THE DIVISION OF THE HUMANITIES IN CANDIDACY FOR THE DEGREE OF DOCTOR OF PHILOSOPHY DEPARTMENT OF MUSIC BY LAURA C.O. SHEARING CHICAGO, ILLINOIS JUNE 2020 ã Copyright 2020 Laura C.O. Shearing All rights reserved. ––For Henrietta Adeline, my wildwood flower Table of Contents List of Figures .............................................................................................................................. v List of Tables .............................................................................................................................. vi Acknowledgements .................................................................................................................... vii Abstract ...................................................................................................................................... ix Introduction ................................................................................................................................ 1 1. Contextualizing Old-Time ..................................................................................................... 22 2. The Making of an Old-Time Heritage Epicenter in Surry County, North Carolina ................... 66 3. Musical Trail-Making in Southern Appalachia ....................................................................... 119 4. American Old-Time in the British Isles ................................................................................ -

Radio Stations
Date Contacted Comments RA_Call EMail FirstName Bluegrass(from Missy) James H. Bluegrass(from Missy) Joe Bluegrass(from Missy) James H. Sent dpk thru Airplay Direct [email protected] 2/9/2014 Bluegrass(from Missy) m Tom Sent dpk thru Airplay Direct cindy@kneedeepi 2/9/2014 Bluegrass(from Missy) nbluegrass.com Cindy Sent dpk thru Airplay Direct drdobro@mindspri 2/9/2014 Bluegrass(from Missy) ng.com Lawrence E. Sent dpk thru Airplay Direct georgemcknight@ 2/9/2014 Bluegrass(from Missy) telus.net George Sent dpk thru Airplay Direct greatstuffradio@y 2/9/2014 Bluegrass(from Missy) ahoo.com Gene Sent dpk thru Airplay Direct jadonchris@netco 2/9/2014 Bluegrass(from Missy) mmander.com Jadon Sent dpk thru Airplay Direct roy@mainstreetbl 2/9/2014 Bluegrass(from Missy) uegrass.com Roy From Americana Music Association reporting stations list ACOUSTIC CAFE Rob From Americana Music Association reporting stations list ALTVILLE Vicki From Americana Music Association reporting stations list Country Bear Stan From Americana Music Association reporting stations list Current 89.3 David From Americana Music Association reporting stations list Farm Fresh Radio Chip From Americana Music Association reporting stations list Folk Alley - WKSU Linda From Americana Music Association reporting stations list FolkScene Roz Sending physical copy 2/2014 per his arthu2go@yahoo. facebook request. Bluegrass(from Missy) 105.9 Bishop FM co.uk Terry Sent dpk thru Airplay Direct lindsay@ozemail. 2/9/2014 Bluegrass(from Missy) 2RRR com.au Lindsay Sent dpk thru Airplay Direct tony.lake@amtac. 2/9/2014 Bluegrass(from Missy) 400R net Tony Sent dpk thru Airplay Direct bluemoon@bluegr 2/9/2014 Bluegrass(from Missy) ACTV-4 asstracks.net Jon C. -

Inside This Issue
News Serving DX’ers since 1933 Volume 82, No. 7●December 29, 2014● (ISSN 0737-1639) Inside this issue . 2 … AM Switch 11 … Domestic DX Digest East 16 … College Sports Networks 5 … Membership Report 14 … International DX Digest 17 … Treasurer’s Report 6 … Domestic DX Digest West 15 … Musings of the Members 18 … Geo Indices/Space Wx Board Announcement: The NRC Board of DecaloMania in Fort Wayne, Indiana, July 10‐12, Directors is pleased to announce the 2015. More details will be forthcoming as our appointment of its newest member to the BoD to host Scott Fybush works them out. fill the vacant seat left by Ken Chatterton after DX Tests: If you want to help arrange tests, his resignation earlier this year. Dave Schmidt, contact Brandon Jordan, the NRC/IRCA Test who has served as Musings of the Members Coordination, at P.O. Box 338, Rossville TN editor for over twenty years and DDXD editor 38066, (901) 592‐9847, and [email protected]. before that, is our newest BoD member. Dave Brandon has set up a web site at also has a keen interest in record collecting and http://dxtests.net/ for the latest test info. And Internet radio (maybe he’ll tell you more in a follow him on Twitter @AMDXTests for the latest Musing soon!). Welcome, Dave! – Paul test info. Swearingen, NRC BoD Chairman. PARI DXpedition: Via the NASWA Journal, DXAS: Fred Vobbe has announced that he Thomas Witherspoon is planning a unique will be stepping down as publisher of the DX DXpedition to the Pisgah Astronomical Research Audio Service after the April 2015 issue. -

Surry County Schools
Middle Grades Student/Parent Handbook Grades 6 - 8 2017-2018 Central Middle Meadowview Middle 883 Zephyr Road, Dobson 27017 1282 McKinney Road, Mt. Airy 27030 336/386-4018 336/386-4371 (Fax) 336/789-0276 336/789-0449 (Fax) J. Sam Gentry Middle Pilot Mountain Middle 1915 West Pine Street, Mt. Airy 27030 543 Old Westfield Road, Pilot Mtn. 27041 336/786-4155 336/786-6863 (Fax) 336/368-2641 336/368-3935 (Fax) Board of Education Dr. Terri E. Mosley, Chairperson Mr. Clark G. Goings, Vice-Chairman Mr. Sexton Earlie Coe Mr. Brian K. Moser Mrs. Mamie M. Sutphin Central Office Administrators Dr. Travis L. Reeves, Superintendent Mr. Kevin T. Via, Assistant Superintendent Dr. Jill Y. Reinhardt, Assistant Superintendent Dr. Jeffrey C. Tunstall, Assistant Superintendent Table of Contents Introduction page 4 Middle School Philosophy page 4 Student Information page 4 Administering Medications Alternative Education Services Asbestos Notification Assembly/School Programs Conduct Bullying/Cyberbullying Child Custody/Court Orders Classroom/Team Policies Contact and Emergency Information Fighting Food Safety Gift Delivery to Students Guide to School Closings Homework Illness or Injury Immunization and Health Requirements for School Admission Laptop Distribution Lice Administrative Rule Lost and Found Narcotics, Alcoholic Beverages, and Stimulant Drugs Personal Property to be Left at Home Pest Management Positive Behavior Intervention and Support Public Displays of Affection School Day Sports Sportsmanship Student Dress Codes Student Searches Textbooks Vandalism -

Revitalization of the AM Radio Service ) ) ) )
Before the FEDERAL COMMUNICATIONS COMMISSION Washington, DC In the matter of: ) ) Revitalization of the AM Radio Service ) MB Docket 13-249 ) ) COMMENTS OF REC NETWORKS One of the primary goals of REC Networks (“REC”)1 is to assure a citizen’s access to the airwaves. Over the years, we have supported various aspects of non-commercial micro- broadcast efforts including Low Power FM (LPFM), proposals for a Low Power AM radio service as well as other creative concepts to use spectrum for one way communications. REC feels that as many organizations as possible should be able to enjoy spreading their message to their local community. It is our desire to see a diverse selection of voices on the dial spanning race, culture, language, sexual orientation and gender identity. This includes a mix of faith-based and secular voices. While REC lacks the technical knowledge to form an opinion on various aspects of AM broadcast engineering such as the “ratchet rule”, daytime and nighttime coverage standards and antenna efficiency, we will comment on various issues which are in the realm of citizen’s access to the airwaves and in the interests of listeners to AM broadcast band stations. REC supports a limited offering of translators to certain AM stations REC feels that there is a segment of “stand-alone” AM broadcast owners. These owners normally fall under the category of minority, women or GLBT/T2. These owners are likely to own a single AM station or a small group of AM stations and are most likely to only own stations with inferior nighttime service, such as Class-D stations. -
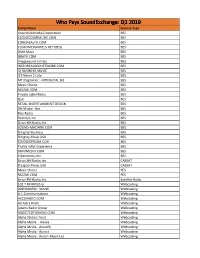
Licensee Count Q1 2019.Xlsx
Who Pays SoundExchange: Q1 2019 Entity Name License Type Aura Multimedia Corporation BES CLOUDCOVERMUSIC.COM BES COROHEALTH.COM BES CUSTOMCHANNELS.NET (BES) BES DMX Music BES GRAYV.COM BES Imagesound Limited BES INSTOREAUDIONETWORK.COM BES IO BUSINESS MUSIC BES It'S Never 2 Late BES MTI Digital Inc - MTIDIGITAL.BIZ BES Music Choice BES MUZAK.COM BES Private Label Radio BES Qsic BES RETAIL ENTERTAINMENT DESIGN BES Rfc Media - Bes BES Rise Radio BES Rockbot, Inc. BES Sirius XM Radio, Inc BES SOUND-MACHINE.COM BES Stingray Business BES Stingray Music USA BES STUDIOSTREAM.COM BES Thales Inflyt Experience BES UMIXMEDIA.COM BES Vibenomics, Inc. BES Sirius XM Radio, Inc CABSAT Stingray Music USA CABSAT Music Choice PES MUZAK.COM PES Sirius XM Radio, Inc Satellite Radio 102.7 FM KPGZ-lp Webcasting 999HANKFM - WANK Webcasting A-1 Communications Webcasting ACCURADIO.COM Webcasting Ad Astra Radio Webcasting Adams Radio Group Webcasting ADDICTEDTORADIO.COM Webcasting Aloha Station Trust Webcasting Alpha Media - Alaska Webcasting Alpha Media - Amarillo Webcasting Alpha Media - Aurora Webcasting Alpha Media - Austin-Albert Lea Webcasting Alpha Media - Bakersfield Webcasting Alpha Media - Biloxi - Gulfport, MS Webcasting Alpha Media - Brookings Webcasting Alpha Media - Cameron - Bethany Webcasting Alpha Media - Canton Webcasting Alpha Media - Columbia, SC Webcasting Alpha Media - Columbus Webcasting Alpha Media - Dayton, Oh Webcasting Alpha Media - East Texas Webcasting Alpha Media - Fairfield Webcasting Alpha Media - Far East Bay Webcasting Alpha Media -

White's Log Radio Stations Television
FALL 1956 ISSUE TVCHANNEL NUMBERS cm FREQUENCY BANDS g RADIO STATIONS KEEP "UP-TO-DATE" ON RADIO STATIONS RADIOWHITE'S LOG RADIO STATIONS TELEVISION FREQUENCYFmMODUI ATION Vol. 33 Keep "Up -to -Date" on Radio Stations No. 2 WHITE'S RADIO LOG Published three times a year by C. DeWitt White Co., Yonkers, N. Y. (Bronxville Branch, Box 142) Charles D'W. White. Prop.35c per copy, $1.00 yearly subscription. FALL 1956 ISSUE October - November - December Entered as second-class matter May 21, 1936, at the Post Office at Yonkers, N. Y.(Bronxville Branch), under the act of March 3, 1879. C. DeW1TT WHITE CO., Publishers P. 0. Box 142, Bronxville 8, N. Y. COPYRIGHT 1956 BY C. DeW1TT WHITE CO. Absolute accuracy of Station and Program information listed in this publication is not guaranteed, although the publishers have applied their best endeavors in compiling same. Contents of this booklet fully covered by U. S. copyright. Any person who wilfully or for profit shall infringe any part thereof will be prosecuted to the full extent of the law. 35c Per Copy Yearly Subscription $1.00 Printed in U. S. A. UNITED STATES BROADCASTING STATIONS ARRANGED ALPHABETICALLY BY CALL LETTERS NOTE: OnlyStations that have been granted a license at time we go to press, appear in this list. FOR WATT POWER OF STATION SEE LIST ARRANGED BY KILOCYCLES Abbreviation: Kc., frequency in kilocycles. Call Let'rs Kc.Call Let'rs Ks. Call Let'rs Ks. I Call Let'rs Ke. DY BU Cebu,P.1. 1260KAWT Douglas,Arlz. 1450 K BST Big Spring,Texas 490KCO H Houston.Texas 430 DZPI Manila,P.1. -

530 CIAO BRAMPTON on ETHNIC AM 530 N43 35 20 W079 52 54 09-Feb
frequency callsign city format identification slogan latitude longitude last change in listing kHz d m s d m s (yy-mmm) 530 CIAO BRAMPTON ON ETHNIC AM 530 N43 35 20 W079 52 54 09-Feb 540 CBKO COAL HARBOUR BC VARIETY CBC RADIO ONE N50 36 4 W127 34 23 09-May 540 CBXQ # UCLUELET BC VARIETY CBC RADIO ONE N48 56 44 W125 33 7 16-Oct 540 CBYW WELLS BC VARIETY CBC RADIO ONE N53 6 25 W121 32 46 09-May 540 CBT GRAND FALLS NL VARIETY CBC RADIO ONE N48 57 3 W055 37 34 00-Jul 540 CBMM # SENNETERRE QC VARIETY CBC RADIO ONE N48 22 42 W077 13 28 18-Feb 540 CBK REGINA SK VARIETY CBC RADIO ONE N51 40 48 W105 26 49 00-Jul 540 WASG DAPHNE AL BLK GSPL/RELIGION N30 44 44 W088 5 40 17-Sep 540 KRXA CARMEL VALLEY CA SPANISH RELIGION EL SEMBRADOR RADIO N36 39 36 W121 32 29 14-Aug 540 KVIP REDDING CA RELIGION SRN VERY INSPIRING N40 37 25 W122 16 49 09-Dec 540 WFLF PINE HILLS FL TALK FOX NEWSRADIO 93.1 N28 22 52 W081 47 31 18-Oct 540 WDAK COLUMBUS GA NEWS/TALK FOX NEWSRADIO 540 N32 25 58 W084 57 2 13-Dec 540 KWMT FORT DODGE IA C&W FOX TRUE COUNTRY N42 29 45 W094 12 27 13-Dec 540 KMLB MONROE LA NEWS/TALK/SPORTS ABC NEWSTALK 105.7&540 N32 32 36 W092 10 45 19-Jan 540 WGOP POCOMOKE CITY MD EZL/OLDIES N38 3 11 W075 34 11 18-Oct 540 WXYG SAUK RAPIDS MN CLASSIC ROCK THE GOAT N45 36 18 W094 8 21 17-May 540 KNMX LAS VEGAS NM SPANISH VARIETY NBC K NEW MEXICO N35 34 25 W105 10 17 13-Nov 540 WBWD ISLIP NY SOUTH ASIAN BOLLY 540 N40 45 4 W073 12 52 18-Dec 540 WRGC SYLVA NC VARIETY NBC THE RIVER N35 23 35 W083 11 38 18-Jun 540 WETC # WENDELL-ZEBULON NC RELIGION EWTN DEVINE MERCY R. -
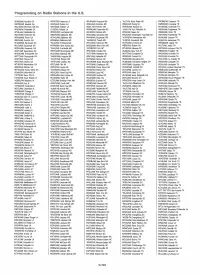
Programming on Radio Stations in the US
Programming on Radio Stations in the U.S. WHBS(AM) Moultrie GA WPRF(FM) Reserve LA WRJW(AM) Picayune MS 'KJLT-FM North Platte NE WSGM(FM) Coalmonl TN WMTM(AM) Moultrie GA KRUS(AM) Ruston LA WSEL(AM) Pontotoc MS WIMG(AM) Ewing NJ WMRB(AM) Columbia TN WALH(AM) Mountain City GA KBYK(AM) Tallulah LA WSEL -FM Pontotoc MS WNSW(AM) Newark NJ WHUB(AM) Cookeville TN WRBX(FM) Reidsville GA KTJZ(FM) Tallulah LA WRPM(AM) Poplarville MS 'WXXY-FM Port Republic NJ WENR(AM) Englewood TN WTNL(AM) Reidsville GA WCMX(AM) Leominster MA WXXB(FM) Richton MS WFAI(AM) Salem NJ WEMB(AM) Erwin TN WZOT(AM) Rockmart GA WBGR(AM) Baltimore MD WSAO(AM) Senatobia MS WNJC(AM) Washington Township NJ WEKR(AM) Fayetteville TN WROM(AM) Rome GA WCAO(AM) Baltimore MD WAVN(AM) Southaven MS 'KUPR(FM) Alamogordo NM WJAK(AM) Jackson TN WBIC(AM) Royston GA WWI(AM) Baltimore MD 'WAQB(FM) Tupelo MS 'KHII(FM) Cloudcroft NM WDEB -FM Jamestown TN WHGM(AM) Savannah GA 'WLIC(FM) Frostburg MD WFCG(FM) Tyler town MS WUFO(AM) Amherst NY WWAM(AM) Jasper TN WJLG(AM) Savannah GA WFBR(AM) Glen Bumie MD WROB(AM) West Point MS WBBF(AM) Buffalo NY WJJT(AM) Jellico TN WSOK(AM) Savannah GA ' WAIJFM) Grantsville MD 'KPGB(FM) Pryor MT WTHE(AM) Mineola NY WETB(AM) Johnson City TN WJAT(AM) Swainsboro GA WPGC(AM) Morningside MD WRCS(AM) Ahoskie NC WLIB(AM) New York NY WBBX(AM) Kingston TN WHGH(AM) Thomasville GA WJDY(AM) Salisbury MD 'WTJY(FM) Asheboro NC WGFT(AM) Campbell OH WKGN(AM) Knoxville TN WSTT(AM) Thomasville GA ' WMDR(AM) Augusta ME WSKY(AM) Asheville NC WINW(AM) Canton OH WKXV(AM) Knoxville -

Exhibit 2181
Exhibit 2181 Case 1:18-cv-04420-LLS Document 131 Filed 03/23/20 Page 1 of 4 Electronically Filed Docket: 19-CRB-0005-WR (2021-2025) Filing Date: 08/24/2020 10:54:36 AM EDT NAB Trial Ex. 2181.1 Exhibit 2181 Case 1:18-cv-04420-LLS Document 131 Filed 03/23/20 Page 2 of 4 NAB Trial Ex. 2181.2 Exhibit 2181 Case 1:18-cv-04420-LLS Document 131 Filed 03/23/20 Page 3 of 4 NAB Trial Ex. 2181.3 Exhibit 2181 Case 1:18-cv-04420-LLS Document 131 Filed 03/23/20 Page 4 of 4 NAB Trial Ex. 2181.4 Exhibit 2181 Case 1:18-cv-04420-LLS Document 132 Filed 03/23/20 Page 1 of 1 NAB Trial Ex. 2181.5 Exhibit 2181 Case 1:18-cv-04420-LLS Document 133 Filed 04/15/20 Page 1 of 4 ATARA MILLER Partner 55 Hudson Yards | New York, NY 10001-2163 T: 212.530.5421 [email protected] | milbank.com April 15, 2020 VIA ECF Honorable Louis L. Stanton Daniel Patrick Moynihan United States Courthouse 500 Pearl St. New York, NY 10007-1312 Re: Radio Music License Comm., Inc. v. Broad. Music, Inc., 18 Civ. 4420 (LLS) Dear Judge Stanton: We write on behalf of Respondent Broadcast Music, Inc. (“BMI”) to update the Court on the status of BMI’s efforts to implement its agreement with the Radio Music License Committee, Inc. (“RMLC”) and to request that the Court unseal the Exhibits attached to the Order (see Dkt. -

Hadiotv EXPERIMENTER AUGUST -SEPTEMBER 75C
DXer's DREAM THAT ALMOST WAS SHASILAND HadioTV EXPERIMENTER AUGUST -SEPTEMBER 75c BUILD COLD QuA BREE ... a 2-FET metal moocher to end the gold drain and De Gaulle! PIUS Socket -2 -Me CB Skyhook No -Parts Slave Flash Patrol PA System IC Big Voice www.americanradiohistory.com EICO Makes It Possible Uncompromising engineering-for value does it! You save up to 50% with Eico Kits and Wired Equipment. (%1 eft ale( 7.111 e, si. a er. ortinastereo Engineering excellence, 100% capability, striking esthetics, the industry's only TOTAL PERFORMANCE STEREO at lowest cost. A Silicon Solid -State 70 -Watt Stereo Amplifier for $99.95 kit, $139.95 wired, including cabinet. Cortina 3070. A Solid -State FM Stereo Tuner for $99.95 kit. $139.95 wired, including cabinet. Cortina 3200. A 70 -Watt Solid -State FM Stereo Receiver for $169.95 kit, $259.95 wired, including cabinet. Cortina 3570. The newest excitement in kits. 100% solid-state and professional. Fun to build and use. Expandable, interconnectable. Great as "jiffy" projects and as introductions to electronics. No technical experience needed. Finest parts, pre -drilled etched printed circuit boards, step-by-step instructions. EICOGRAFT.4- Electronic Siren $4.95, Burglar Alarm $6.95, Fire Alarm $6.95, Intercom $3.95, Audio Power Amplifier $4.95, Metronome $3.95, Tremolo $8.95, Light Flasher $3.95, Electronic "Mystifier" $4.95, Photo Cell Nite Lite $4.95, Power Supply $7.95, Code Oscillator $2.50, «6 FM Wireless Mike $9.95, AM Wireless Mike $9.95, Electronic VOX $7.95, FM Radio $9.95, - AM Radio $7.95, Electronic Bongos $7.95.