National Survey of HIV and Syphilis Prevalence Among
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Integrated Testing for TB and HIV Zimbabwe
AUGUST 2019 ZIMBABWE TB AND HIV FAST FACTS 1.3 MILLION PEOPLE LIVING WITH HIV % ADULT HIV 13.3 PREVALENCE (AGES 15–49 YEARS) 37,000 PEOPLE FELL ILL WITH TUBERCULOSIS (TB)* © UNICEF/Costa/Zimbabwe INTEGRATED TESTING FOR TB AND HIV 23,000 USING GENEXPERT DEVICES EXPANDS PEOPLE LIVING WITH HIV ACCESS TO NEAR-POINT-OF-CARE TESTING FELL ILL * LESSONS LEARNED FROM ZIMBABWE WITH TB Introduction With limited funding for global health, identifying practical, cost- and time- OF TB PATIENTS % saving solutions while also ensuring quality of care is evermore important. 63ARE PEOPLE Globally, there are fleets of molecular testing platforms within laboratories WITH KNOWN HIV-POSITIVE and at the point of care (POC), the majority of which were placed to offer STATUS disease-specific services such as the diagnosis of tuberculosis (TB) or HIV in infants. Since November 2015, Clinton Health Access Initiative, Inc. (CHAI), the United Nations Children’s Fund (UNICEF) and the African Society of Laboratory Medicine (ASLM), with funding from Unitaid, have % OF HIV-EXPOSED been working closely with ministries of health across 10 countries in sub- Saharan Africa to introduce innovative POC technologies into national INFANTS 1 63 health programmes. RECEIVED AN HIV TEST WITHIN THE FIRST TWO One approach to increasing access to POC testing is integrated testing MONTHS OF LIFE (a term often used interchangeably with “multi-disease testing”), which is testing for different conditions or diseases using the same diagnostic *Annually platform.2 Leveraging excess capacity on existing devices to enable testing Sources: UNAIDS estimates 2019; World Health across multiple diseases offers the potential to optimize limited human Organization, ‘Global Tuberculosis Report 2018’ and financial resources at health facilities, while increasing access to rapid testing services. -

Organization Profile
Organization Profile “Community Participation and Ownership key to sustainable Development” 1 Organization Contact Details PHYSICAL ADDRESS: AVOCA REVIVAL CRUSADE MISSIONS CHURCH, AVOCA,FILABUSI, MATABELELAND SOUTH PROVINCE, ZIMBABWE, SOUTHERN AFRICA CELL: 00263- 712 686 536, 0715499853 E-mail: [email protected], [email protected] REGISTRATION DETAILS, TRUST REGISTRATION : M 446/2015 NAMES OF CONTACT PERSONS : Nkululeko Tshuma (Mr.) Director Praxcedes Moyo (Miss.) Programs Officer GEOGRAPHIC COVERAGE : Mat South- Insiza,Umzingwane, gwanda Districts (B)ORGANISATIONAL INFORMATION Organizational history Godlwayo Community Development Trust (GCDT) a community based organization (CBO) was founded in February 2014. Initially a community lobby and advocacy group on human rights issues encompassing HIV and AIDS issues, livelihoods and governance issues was founded within the Godlwayo (Filabusi) community (Matabeleland South, Zimbabwe). The need to improve schools pass rate within Filabusi area greatly informed the formation of this initiative as the community well wishers started making financial donations towards paying school fees for disadvantaged but ably performing school kids and this gave birth to a program called Godlwayo Education scholarship Program (GESP). Also the community identified gaps in information dissemination since there is a media blackout in the area so the idea of a community radio initiative was then muted and supported and this gave birth to a community radio initiative by name Godlwayofm specifically for information dissemination currently using bulk sms facility to share community news. After a year of operating in Godlwayo (Filabusi) it has been noted that the services of the organization are needed in other district and surrounding areas and since this means growth and expansion, the need to register as a formal organization was then realized. -

Bulawayo City Mpilo Central Hospital
Province District Name of Site Bulawayo Bulawayo City E. F. Watson Clinic Bulawayo Bulawayo City Mpilo Central Hospital Bulawayo Bulawayo City Nkulumane Clinic Bulawayo Bulawayo City United Bulawayo Hospital Manicaland Buhera Birchenough Bridge Hospital Manicaland Buhera Murambinda Mission Hospital Manicaland Chipinge Chipinge District Hospital Manicaland Makoni Rusape District Hospital Manicaland Mutare Mutare Provincial Hospital Manicaland Mutasa Bonda Mission Hospital Manicaland Mutasa Hauna District Hospital Harare Chitungwiza Chitungwiza Central Hospital Harare Chitungwiza CITIMED Clinic Masvingo Chiredzi Chikombedzi Mission Hospital Masvingo Chiredzi Chiredzi District Hospital Masvingo Chivi Chivi District Hospital Masvingo Gutu Chimombe Rural Hospital Masvingo Gutu Chinyika Rural Hospital Masvingo Gutu Chitando Rural Health Centre Masvingo Gutu Gutu Mission Hospital Masvingo Gutu Gutu Rural Hospital Masvingo Gutu Mukaro Mission Hospital Masvingo Masvingo Masvingo Provincial Hospital Masvingo Masvingo Morgenster Mission Hospital Masvingo Mwenezi Matibi Mission Hospital Masvingo Mwenezi Neshuro District Hospital Masvingo Zaka Musiso Mission Hospital Masvingo Zaka Ndanga District Hospital Matabeleland South Beitbridge Beitbridge District Hospital Matabeleland South Gwanda Gwanda Provincial Hospital Matabeleland South Insiza Filabusi District Hospital Matabeleland South Mangwe Plumtree District Hospital Matabeleland South Mangwe St Annes Mission Hospital (Brunapeg) Matabeleland South Matobo Maphisa District Hospital Matabeleland South Umzingwane Esigodini District Hospital Midlands Gokwe South Gokwe South District Hospital Midlands Gweru Gweru Provincial Hospital Midlands Kwekwe Kwekwe General Hospital Midlands Kwekwe Silobela District Hospital Midlands Mberengwa Mberengwa District Hospital . -

Promotion of Climate-Resilient Lifestyles Among Rural Families in Gutu
Promotion of climate-resilient lifestyles among rural families in Gutu (Masvingo Province), Mutasa (Manicaland Province) and Shamva (Mashonaland Central Province) Districts | Zimbabwe Sahara and Sahel Observatory 26 November 2019 Promotion of climate-resilient lifestyles among rural families in Gutu Project/Programme title: (Masvingo Province), Mutasa (Manicaland Province) and Shamva (Mashonaland Central Province) Districts Country(ies): Zimbabwe National Designated Climate Change Management Department, Ministry of Authority(ies) (NDA): Environment, Water and Climate Development Aid from People to People in Zimbabwe (DAPP Executing Entities: Zimbabwe) Accredited Entity(ies) (AE): Sahara and Sahel Observatory Date of first submission/ 7/19/2019 V.1 version number: Date of current submission/ 11/26/2019 V.2 version number A. Project / Programme Information (max. 1 page) ☒ Project ☒ Public sector A.2. Public or A.1. Project or programme A.3 RFP Not applicable private sector ☐ Programme ☐ Private sector Mitigation: Reduced emissions from: ☐ Energy access and power generation: 0% ☐ Low emission transport: 0% ☐ Buildings, cities and industries and appliances: 0% A.4. Indicate the result ☒ Forestry and land use: 25% areas for the project/programme Adaptation: Increased resilience of: ☒ Most vulnerable people and communities: 25% ☒ Health and well-being, and food and water security: 25% ☐ Infrastructure and built environment: 0% ☒ Ecosystem and ecosystem services: 25% A.5.1. Estimated mitigation impact 399,223 tCO2eq (tCO2eq over project lifespan) A.5.2. Estimated adaptation impact 12,000 direct beneficiaries (number of direct beneficiaries) A.5. Impact potential A.5.3. Estimated adaptation impact 40,000 indirect beneficiaries (number of indirect beneficiaries) A.5.4. Estimated adaptation impact 0.28% of the country’s total population (% of total population) A.6. -

TREATMENT SITES Southern Africa HIV and AIDS Information LISTED by PROVINCE and AREA Dissemination Service
ARV TREATMENT SITES Southern Africa HIV and AIDS Information LISTED BY PROVINCE AND AREA Dissemination Service MASVINGO · Bulilima: Plumtree District hospital: · Bikita: Silveira Mission Hospital: Tel: (038)324 Tel. (019) 2291; 2661-3 · Chiredzi: Hippo Valley Estates Clinic: · Gwanda: Gwanda OI Clinic: Tel: (084)22661-3: Tel: (031)2264 - Mangwe: St. Annes Brunapeg: · Chiredzi: Colin Saunders Hosp. Tel: (082) 361/466 AN HIV/AIDS Tel: (033)6387:6255 · Kezi-Matobo: Tshelanyemba Mission Hosp: · Chiredzi: Chiredzi District Hosp.: Tel: (033) Tel: (082) 254 · Gutu: Gutu Mission Hosp: · Maphisa District Hosp: Tel. (082) 244 Tel: (030)2323:2313:2631:3229 · Masvingo: Morgenster Mission Hosp: MIDLANDS Tel: (039)262123 · Chivhu General Hosp: Tel: (056):2644:2351 TREATMENT - Masvingo Provincial Hosp: · Chirumhanzu: Muvonde Hosp: Tel: (032)346 Tel: (039)263358/9; 263360 · Mvuma: St Theresas Mission Hosp: - Masvingo: Mukurira Memorial Private Hospital: Tel: (0308)208/373 Tel. (039) 264919 · Gweru: Gweru Provincial Hospital: ROADMAP FOR · Mwenezi: Matibi Mission Hospital: Tel. (0517) 323 Tel: (054) 221301:221108 · Zaka: Musiso Mission Hosp: · Gweru: Gweru City Hospital: Tel: (054) Tel: (034)2286:2322:2327/8 221301:221108 - Gweru: Mkoba 1 Polyclinic, Tel. MATEBELELAND NORTH - Gweru: Lower Gweru Rural Health Clinic: · Hwange: St Patricks Mission Hosp: Tel: (054) 227023 Tel: (081)34316-7 · Kwekwe: Kwekwe General Hospital: ZIMBABWE · Lupane: St Lukes Mission Hosp: Tel: (055)22333/7:24828/31 Tel: (0898)362:549:349 · Mberengwa: Mnene Mission Hospital: · Tsholotsho: Tsholotsho District Hosp: Tel. (0518) 352/3 Tel: (0878) 397/216/299 A guide for accessing anti- PRIVATE DOCTORS retroviral treatment in MATEBELELAND SOUTH For a list of private doctors who have special Zimbabwe: what it is, where · Beitbridge: Beitbridge District Hosp: training in ARV treatment and counselling, ask Tel.(086) 22496-8 your own doctor or contact SAfAIDS. -

Faculty of Arts Department of History And
FACULTY OF ARTS DEPARTMENT OF HISTORY AND INTERNATIONAL STUDIES RESOURCE NATIONALISM AND LOCAL EMPOWERMENT, THE CASE OF ZVISHAVANE COMMUNITY SHARE OWNERSIP TRUST, 2012 TO 2017. By FAITH MAFUNGA R147013M SUPERVISOR: DR T. MASHINGAIDZE A DISSERTATION SUBMITTED TO THE HISTORY DEPARTMENT OF THE MIDLANDS STATE UNIVERSITY IN PARTIAL FULFILMENT OF THE REQUIREMENTS OF THE BACHELOR OF ARTS IN HISTORY AND INTERNATIONAL STUDIES HONOURS DEGREE. ZVISHAVANE, ZIMBABWE JUNE 2018 Declaration I, Faith Mafunga declare that this dissertation hereby submitted for the Bachelor of Arts Honors Degree in History and International Studies at Midlands State University is my own effort. Information from published and unpublished work from other authors have been acknowledged. …………………………. ……………………………… Student Date i Approval form The undersigned certify that they have supervised and recommended to Midlands State University the student FAITH MAFUNGA dissertation entitled RESOURCE NATIONALISM AND LOCAL EMPOWERMENT, THE CASEOF ZVISHAVANE COMMUNITY SHARE OWNERSIP TRUST, 2012 TO 2017. The dissertation submitted in partial fulfillment of the requirements for the History and International Studies Department. …………………………. ……………………………… Supervisor Date …………………………… …………………………………. Chairperson Date …………………………. ……………………………………… External Examiner Date ii Dedication This piece of work is dedicated to my late father Mr. E.C Mafunga, my mother Mrs. E Mauto, my siblings Yvonne, Tanaka and Tafadzwa Mafunga. Thank you all for your constant love and support. God Bless you. iii Acknowledgements Utmost gratitude goes to God Almighty for he has been an unwavering source of strength throughout my academic years. I must pay tribute to my academic supervisor Doctor Mashingaidze who has given me supervision and motivation throughout this research. My exceptional gratefulness also goes to Mr. N.T Jinga the C.E.O of ZCSOT and the entire organization for helping me in crafting this dissertation. -

Grant Assistance for Grassroots Human Projects in Zimbabwe
Grant Assistance for Grassroots Human Projects in Zimbabwe Amount Amount No Year Project Title Implementing Organisation District (US) (yen) 1 1989 Mbungu Primary School Development Project Mbungu Primary School Gokwe 16,807 2,067,261 2 1989 Sewing and Knitting Project Rutowa Young Women's Club Gutu 5,434 668,382 3 1990 Children's Agricultural Project Save the Children USA Nyangombe 8,659 1,177,624 Mbungo Uniform Clothing Tailoring Workshop 4 1990 Mbungo Women's Club Masvingo 14,767 2,008,312 Project Construction of Gardening Facilities in 5 1991 Cold Comfort Farm Trust Harare 42,103 5,431,287 Support of Small-Scale Farmers 6 1991 Pre-School Project Kwayedza Cooperative Gweru 33,226 4,286,154 Committee for the Rural Technical 7 1992 Rural Technical Training Project Murehwa 38,266 4,936,314 Training Project 8 1992 Mukotosi Schools Project Mukotosi Project Committee Chivi 20,912 2,697,648 9 1992 Bvute Dam Project Bvute Dam Project Committee Chivi 3,558 458,982 10 1992 Uranda Clinic Project Uranda Clinic Project Committee Chivi 1,309 168,861 11 1992 Utete Dam Project Utete Dam Project Committee Chivi 8,051 1,038,579 Drilling of Ten Boreholes for Water and 12 1993 Irrigation in the Inyathi and Tsholotsho Help Age Zimbabwe Tsholotsho 41,574 5,072,028 PromotionDistricts of ofSocialForestry Matabeleland andManagement Zimbabwe National Conservation 13 1993 Buhera 46,682 5,695,204 ofWoodlands inCommunalAreas ofZimbabwe Trust Expansion of St. Mary's Gavhunga Primary St. Mary's Gavhunga Primary 14 1994 Kadoma 29,916 3,171,096 School School Tsitshatshawa -

High Frequency Monitoring Report Bulletin #21 | February 2019
Bulletin #21 • February 2019 • www.zrbf.co.zw The purpose of the ZRBF High Frequency Monitoring Bulletin is to avail real IN THIS REPORT time data and information on identified and agreed trigger indicators for Overall Results and Implications 2 the activation of the crisis modifier, performance monitoring, programming Implications and Actions related to Resilience and other decisions for the overall ZRBF adaptive programme management. Programming 4 Information presented in this bulletin is readily available in the HFM Online Status Update on Macro-Trigger Indicators 5 Database, accessible using this url Vegetation Condition Index 5 https://197.155.231.242/undp/ZRBF/HFMS/index.php Real-time water levels in major rivers 5 The bulletin contains official information for the month of January 2019 collected Summary of Broad Classification: Micro Trigger from various sources by ZRBF partners and analysed by ZRBF PMU. The High Indicators 5 Frequency Monitoring Bulletin is a product of collaboration between the ZRBF Detailed Micro Trigger Indicators Update 6 Partners and other government agencies. For questions and comments regarding National Media Monitoring for Early-Warning this bulletin, kindly get in touch withVhusomuzi Sithole (vhusomuzi.sithole@ Signals 10 undp.org), Alfios Mayoyo ([email protected]) or Rufael Fassil (rufael. Annex 1: Flood monitoring thresholds for water [email protected]). level in selected rivers 11 UNDP Zimbabwe, ZRBF Programme Management Unit Arundel Office Park, Block 9, Norfolk Rd, Mt. Pleasant, Harare, Zimbabwe, Phone: +263 4 338836-44 Page 2 | High Frequency Monitoring Report Bulletin #21 | February 2019 Overall Results and Implications Summary Classification Key Highlights According to the High Frequency Monitoring (HFM) classification, 15 districts were rated “Alert” and the remaining three did not report. -
ANALYSIS of SPATIAL PATTERNS of SETTLEMENT, INTERNAL MIGRATION, and WELFARE INEQUALITY in ZIMBABWE 1 Analysis of Spatial
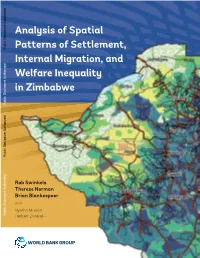
ANALYSIS OF SPATIAL PATTERNS OF SETTLEMENT, INTERNAL MIGRATION, AND WELFARE INEQUALITY IN ZIMBABWE 1 Analysis of Spatial Public Disclosure Authorized Patterns of Settlement, Internal Migration, and Welfare Inequality in Zimbabwe Public Disclosure Authorized Public Disclosure Authorized Rob Swinkels Therese Norman Brian Blankespoor WITH Nyasha Munditi Public Disclosure Authorized Herbert Zvirereh World Bank Group April 18, 2019 Based on ZIMSTAT data Zimbabwe District Map, 2012 Zimbabwe Altitude Map ii ANALYSIS OF SPATIAL PATTERNS OF SETTLEMENT, INTERNAL MIGRATION, AND WELFARE INEQUALITY IN ZIMBABWE TABLE OF CONTENTS ACKNOWLEDGMENTS iii ABSTRACT v EXECUTIVE SUMMARY ix ABBREVIATIONS xv 1. INTRODUCTION AND OBJECTIVES 1 2. SPATIAL ELEMENTS OF SETTLEMENT: WHERE DID PEOPLE LIVE IN 2012? 9 3. RECENT POPULATION MOVEMENTS 27 4. REASONS BEHIND THE SPATIAL SETTLEMENT PATTERN AND POPULATION MOVEMENTS 39 5. CONSEQUENCES OF THE POPULATION’S SPATIAL DISTRIBUTION 53 6. POLICY DISCUSSION 71 AREAS FOR FURTHER RESEARCH 81 REFERENCES 83 APPENDIX A. SUPPLEMENTAL MAPS AND CHARTS 87 APPENDIX B. RESULTS OF REGRESSION ANALYSIS 99 APPENDIX C. EXAMPLE OF LOCAL DEVELOPMENT INDEX 111 ACKNOWLEDGMENTS This report was prepared by a team led by Rob Swinkels, comprising Therese Norman and Brian Blankespoor. Important background work was conducted by Nyasha Munditi and Herbert Zvirereh. Wishy Chipiro provided valuable technical support. Overall guidance was provided by Andrew Dabalen, Ruth Hill, and Mukami Kariuki. Peer reviewers were Luc Christiaensen, Nagaraja Rao Harshadeep, Hans Hoogeveen, Kirsten Hommann, and Marko Kwaramba. Tawanda Chingozha commented on an earlier draft and shared the shapefiles of the Zimbabwe farmland use types. Yondela Silimela, Carli Bunding-Venter, Leslie Nii Odartey Mills, and Aiga Stokenberga provided inputs to the policy section. -

Original Research Article the Spatial Dimension of Health Service
Scholars Journal of Applied Medical Sciences (SJAMS) ISSN 2320-6691 (Online) Sch. J. App. Med. Sci., 2016; 4(1C):201-204 ISSN 2347-954X (Print) ©Scholars Academic and Scientific Publisher (An International Publisher for Academic and Scientific Resources) www.saspublisher.com Original Research Article The Spatial Dimension of Health Service Provision in Mashonaland West Province, Zimbabwe Takudzwa Mhandu, Dr Evans Chazireni Great Zimbabwe University, P O Box 1235, Masvingo, Zimbabwe *Corresponding author Dr Evans Chazireni Email: Abstract: Zimbabwe like many other developing countries has serious problems in its healthcare system. The quality of health service provision in Zimbabwe is generally poor Chazireni. Different parts of the country have serious healthcare problems. Mashonaland West, like other provinces in Zimbabwe, experiences numerous healthcare challenges. The research examines health service provision in Mashonaland West province in Zimbabwe. Data for this study was collected from ZIMSTAT published census reports and Ministry of health and Child Welfare published national health profiles. The analysis of the data was done through the composite index method. The calculated composite indices were used to rank the districts according to the level of health service provision. The researcher found out that there overall, the conditions of health service provision in Mashonaland West province is poor and that there are health service disparities among administrative districts in Mashonaland West province of Zimbabwe. There are many reasons which contribute to disparities in health care services at different levels (global, continental, regional, national and district level). It emerged from the research that the disparities are due to social, economic, physical and political factors. -

Alluvial Aquifers in the Mzingwane Catchment: Their Distribution, Properties, Current Usage and Potential Expansion
Physics and Chemistry of the Earth 31 (2006) 988–994 www.elsevier.com/locate/pce Alluvial aquifers in the Mzingwane catchment: Their distribution, properties, current usage and potential expansion William Moyce a,*, Pride Mangeya a, Richard Owen a,d, David Love b,c a Department of Geology, University of Zimbabwe, P.O. Box MP167, Mt. Pleasant, Harare, Zimbabwe b WaterNet, P.O. Box MP600, Mt. Pleasant, Harare, Zimbabwe c ICRISAT Bulawayo, Matopos Research Station, P.O. Box 776, Bulawayo, Zimbabwe d Minerals Resources Centre, University of Zimbabwe, P.O. Box MP167, Mt. Pleasant, Harare, Zimbabwe Abstract The Mzingwane River is a sand filled channel, with extensive alluvial aquifers distributed along its banks and bed in the lower catch- ment. LandSat TM imagery was used to identify alluvial deposits for potential groundwater resources for irrigation development. On the false colour composite band 3, band 4 and band 5 (FCC 345) the alluvial deposits stand out as white and dense actively growing veg- etation stands out as green making it possible to mark out the lateral extent of the saturated alluvial plain deposits using the riverine fringe and vegetation . The alluvial aquifers form ribbon shaped aquifers extending along the channel and reaching over 20 km in length in some localities and are enhanced at lithological boundaries. These alluvial aquifers extend laterally outside the active channel, and individual alluvial aquifers have been measured with area ranging from 45 ha to 723 ha in the channels and 75 ha to 2196 ha on the plains. The alluvial aquifers are more pronounced in the Lower Mzingwane, where the slopes are gentler and allow for more sediment accumulation. -

Climate-Smart Agriculture Manual for Zimbabwe, Climate Technology Centre and Network, Denmark, 2017
Climate-Smart Agriculture supporting low carbon and climate resilient development Climat e-Smart A griculture Manual f or A griculture Educ The Climate Technology Centre and Network (CTCN) fosters technology transfer and deployment at the request of developing countries through three core services: technical assistance, capacity building and scaling up international collaboration. The Centre is the operational arm of the UNFCCC Technology Mechanism, it is hosted and managed by Email: [email protected] the United Nations Environment and the United Nations Industrial Development Organisation Web: www.ctc-n.org (UNIDO), and supported by more than 300 network partners around the world. ation in Zimbab CTCN Supported by: w e United Nations Framework Convention on Climate Change Climate-Smart Ministry of Agriculture, Mechanisation and Irrigation Development Department of Agriculture Education and Farmer Training Agriculture Manual Ngungunyana Building No. 1 Borrowdale Road for Agriculture Education in Zimbabwe Harare, Zimbabwe Tel: +263 (0) 4 797390 Email: [email protected] www.moa.gov.zw Ministry of Environment, Water and Climate 11th Floor, Kaguvi Building, Cnr S. V. Muzenda Street and Central Avenue, Harare, Zimbabwe Tel: +263-4-701681/3 e-mail: [email protected] website: www.climatechange.org.zw Climate-SmartClimate-SmartClimate-SmartClimate-Smart AAAgricultureAgriculturegriculturegriculture Manual ManualManual Manual for ffAororgriculturefor AA griculturegricultureAgriculture Educ EducEduc Educationationationation in Zimbab inin