View on Enteric Caliciviruses And
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Antiviral Bioactive Compounds of Mushrooms and Their Antiviral Mechanisms: a Review
viruses Review Antiviral Bioactive Compounds of Mushrooms and Their Antiviral Mechanisms: A Review Dong Joo Seo 1 and Changsun Choi 2,* 1 Department of Food Science and Nutrition, College of Health and Welfare and Education, Gwangju University 277 Hyodeok-ro, Nam-gu, Gwangju 61743, Korea; [email protected] 2 Department of Food and Nutrition, School of Food Science and Technology, College of Biotechnology and Natural Resources, Chung-Ang University, 4726 Seodongdaero, Daeduck-myun, Anseong-si, Gyeonggi-do 17546, Korea * Correspondence: [email protected]; Tel.: +82-31-670-4589; Fax: +82-31-676-8741 Abstract: Mushrooms are used in their natural form as a food supplement and food additive. In addition, several bioactive compounds beneficial for human health have been derived from mushrooms. Among them, polysaccharides, carbohydrate-binding protein, peptides, proteins, enzymes, polyphenols, triterpenes, triterpenoids, and several other compounds exert antiviral activity against DNA and RNA viruses. Their antiviral targets were mostly virus entry, viral genome replication, viral proteins, and cellular proteins and influenced immune modulation, which was evaluated through pre-, simultaneous-, co-, and post-treatment in vitro and in vivo studies. In particular, they treated and relieved the viral diseases caused by herpes simplex virus, influenza virus, and human immunodeficiency virus (HIV). Some mushroom compounds that act against HIV, influenza A virus, and hepatitis C virus showed antiviral effects comparable to those of antiviral drugs. Therefore, bioactive compounds from mushrooms could be candidates for treating viral infections. Citation: Seo, D.J.; Choi, C. Antiviral Bioactive Compounds of Mushrooms Keywords: mushroom; bioactive compound; virus; infection; antiviral mechanism and Their Antiviral Mechanisms: A Review. -

Guide for Common Viral Diseases of Animals in Louisiana
Sampling and Testing Guide for Common Viral Diseases of Animals in Louisiana Please click on the species of interest: Cattle Deer and Small Ruminants The Louisiana Animal Swine Disease Diagnostic Horses Laboratory Dogs A service unit of the LSU School of Veterinary Medicine Adapted from Murphy, F.A., et al, Veterinary Virology, 3rd ed. Cats Academic Press, 1999. Compiled by Rob Poston Multi-species: Rabiesvirus DCN LADDL Guide for Common Viral Diseases v. B2 1 Cattle Please click on the principle system involvement Generalized viral diseases Respiratory viral diseases Enteric viral diseases Reproductive/neonatal viral diseases Viral infections affecting the skin Back to the Beginning DCN LADDL Guide for Common Viral Diseases v. B2 2 Deer and Small Ruminants Please click on the principle system involvement Generalized viral disease Respiratory viral disease Enteric viral diseases Reproductive/neonatal viral diseases Viral infections affecting the skin Back to the Beginning DCN LADDL Guide for Common Viral Diseases v. B2 3 Swine Please click on the principle system involvement Generalized viral diseases Respiratory viral diseases Enteric viral diseases Reproductive/neonatal viral diseases Viral infections affecting the skin Back to the Beginning DCN LADDL Guide for Common Viral Diseases v. B2 4 Horses Please click on the principle system involvement Generalized viral diseases Neurological viral diseases Respiratory viral diseases Enteric viral diseases Abortifacient/neonatal viral diseases Viral infections affecting the skin Back to the Beginning DCN LADDL Guide for Common Viral Diseases v. B2 5 Dogs Please click on the principle system involvement Generalized viral diseases Respiratory viral diseases Enteric viral diseases Reproductive/neonatal viral diseases Back to the Beginning DCN LADDL Guide for Common Viral Diseases v. -

Calicivirus from Novel Recovirus Genogroup in Human Diarrhea
DISPATCHES οf ≈6.4–8.4 kb, cause illness in animals and humans (8,9), Calicivirus from including gastroenteritis in humans. The family Caliciviri- dae consists of 5 genera, Norovirus, Sapovirus, Lagovirus, Novel Recovirus Vesivirus, and Nebovirus, and 3 proposed genera, Recovi- Genogroup in rus, Valovirus, and chicken calicivirus (8–10). The Study Human Diarrhea, Each year, >100,000 diarrhea patients are admitted to Bangladesh the Dhaka hospital of the International Centre for Diarrheal Disease Research, Bangladesh (ICDDR,B). Fecal samples Saskia L. Smits, Mustafi zur Rahman, from 2% of these patients are collected and examined as part Claudia M.E. Schapendonk, Marije van Leeuwen, of systematic routine surveillance system for the presence Abu S.G. Faruque, Bart L. Haagmans, of enteric pathogens (11). All procedures were performed in Hubert P. Endtz, and Albert D.M.E. Osterhaus compliance with relevant laws and institutional guidelines and in accordance with the Declaration of Helsinki. To identify unknown human viruses in the enteric tract, we examined 105 stool specimens from patients with diar- rhea in Bangladesh. A novel calicivirus was identifi ed in a sample from 1 patient and subsequently found in samples from 5 other patients. Phylogenetic analyses classifi ed this virus within the proposed genus Recovirus. iarrhea, characterized by frequent liquid or loose Dstools, commonly results from gastroenteritis caused by infection with bacteria, parasites, or viruses. Patients with mild diarrhea do not require medical attention; the ill- ness is typically self-limited, and disease symptoms usually resolve quickly. However, diarrheal diseases can result in severe illness and death worldwide and are the second lead- ing cause of death around the world in children <5 years of age, particularly in low- and middle-income countries (1). -

Downloads/Global-Burden-Report.Pdf (Accessed on 20 December 2017)
viruses Review The Interactions between Host Glycobiology, Bacterial Microbiota, and Viruses in the Gut Vicente Monedero 1, Javier Buesa 2 and Jesús Rodríguez-Díaz 2,* ID 1 Department of Food Biotechnology, Institute of Agrochemistry and Food Technology (IATA, CSIC), Av Catedrático Agustín Escardino, 7, 46980 Paterna, Spain; [email protected] 2 Departament of Microbiology, Faculty of Medicine, University of Valencia, Av. Blasco Ibañez 17, 46010 Valencia, Spain; [email protected] * Correspondence: [email protected]; Tel.: +34-96-386-4903; Fax: +34-96-386-4960 Received: 31 January 2018; Accepted: 22 February 2018; Published: 24 February 2018 Abstract: Rotavirus (RV) and norovirus (NoV) are the major etiological agents of viral acute gastroenteritis worldwide. Host genetic factors, the histo-blood group antigens (HBGA), are associated with RV and NoV susceptibility and recent findings additionally point to HBGA as a factor modulating the intestinal microbial composition. In vitro and in vivo experiments in animal models established that the microbiota enhances RV and NoV infection, uncovering a triangular interplay between RV and NoV, host glycobiology, and the intestinal microbiota that ultimately influences viral infectivity. Studies on the microbiota composition in individuals displaying different RV and NoV susceptibilities allowed the identification of potential bacterial biomarkers, although mechanistic data on the virus–host–microbiota relation are still needed. The identification of the bacterial and HBGA interactions that are exploited by RV and NoV would place the intestinal microbiota as a new target for alternative therapies aimed at preventing and treating viral gastroenteritis. Keywords: rotavirus; norovirus; secretor; fucosyltransferase-2 gene (FUT2); histo-blood group antigens (HBGAs); microbiota; host susceptibility 1. -

Norovirus Infectious Agent Information Sheet
Norovirus Infectious Agent Information Sheet Introduction Noroviruses are non-enveloped (naked) RNA viruses with icosahedral nucleocapsid symmetry. The norovirus genome consists of (+) ssRNA, containing three open reading frames that encode for proteins required for transcription, replication, and assembly. There are five norovirus genogroups (GI-GV), and only GI, GII, and GIV infect humans. Norovirus belongs to the Caliciviridae family of viruses, and has had past names including, Norwalk virus and “winter-vomiting” disease. Epidemiology and Clinical Significance Noroviruses are considered the most common cause of outbreaks of non-bacterial gastroenteritis worldwide, are the leading cause of foodborne illness in the United States (58%), and account for 26% of hospitalizations and 10% of deaths associated with food consumption. Salad ingredients, fruit, and oysters are the most implicated in norovirus outbreaks. Aside from food and water, Noroviruses can also be transmitted by person to person contact and contact with environmental surfaces. The rapid spread of secondary infections occurs in areas where a large population is enclosed within a static environment, such as cruise ships, military bases, and institutions. Symptoms typically last for 24 to 48 hours, but can persist up to 96 hours in the immunocompromised. Pathogenesis, Immunity, Treatment and Prevention Norovirus is highly infectious due to low infecting dose, high excretion level (105 to 107 copies/mg stool), and continual shedding after clinical recovery (>1 month). The norovirus genome undergoes frequent change due to mutation and recombination, which increases its prevalence. Studies suggest that acquired immunity only last 6 months after infection. Gastroenteritis, an inflammation of the stomach and small and large intestines, is caused by norovirus infection. -

Metagenomic Analysis of the Turkey Gut RNA Virus Community J Michael Day1*, Linda L Ballard2, Mary V Duke2, Brian E Scheffler2, Laszlo Zsak1
Day et al. Virology Journal 2010, 7:313 http://www.virologyj.com/content/7/1/313 RESEARCH Open Access Metagenomic analysis of the turkey gut RNA virus community J Michael Day1*, Linda L Ballard2, Mary V Duke2, Brian E Scheffler2, Laszlo Zsak1 Abstract Viral enteric disease is an ongoing economic burden to poultry producers worldwide, and despite considerable research, no single virus has emerged as a likely causative agent and target for prevention and control efforts. Historically, electron microscopy has been used to identify suspect viruses, with many small, round viruses eluding classification based solely on morphology. National and regional surveys using molecular diagnostics have revealed that suspect viruses continuously circulate in United States poultry, with many viruses appearing concomitantly and in healthy birds. High-throughput nucleic acid pyrosequencing is a powerful diagnostic technology capable of determining the full genomic repertoire present in a complex environmental sample. We utilized the Roche/454 Life Sciences GS-FLX platform to compile an RNA virus metagenome from turkey flocks experiencing enteric dis- ease. This approach yielded numerous sequences homologous to viruses in the BLAST nr protein database, many of which have not been described in turkeys. Our analysis of this turkey gut RNA metagenome focuses in particular on the turkey-origin members of the Picornavirales, the Caliciviridae, and the turkey Picobirnaviruses. Introduction remains elusive, and many enteric viruses can be Enteric disease syndromes such as Poult Enteritis Com- detected in otherwise healthy turkey and chicken flocks plex (PEC) in young turkeys and Runting-Stunting Syn- [3,4]. Regional and national enteric virus surveys have drome (RSS) in chickens are a continual economic revealed the ongoing presence of avian reoviruses, rota- burden for poultry producers. -
Global Burden of Norovirus and Prospects for Vaccine Development
Global Burden of Norovirus and Prospects for Vaccine Development Primary author Ben Lopman Centers for Disease Control and Prevention Contributors and Reviewers Robert Atmar, Baylor College of Medicine Ralph Baric, University of North Carolina Mary Estes, Baylor College of Medicine Kim Green, NIH; National Institute of Allergy and Infectious Diseases Roger Glass, NIH; Fogarty International Center Aron Hall, Centers for Disease Control and Prevention Miren Iturriza-Gómara, University of Liverpool Cherry Kang, Christian Medical College Bruce Lee, Johns Hopkins University Umesh Parashar, Centers for Disease Control and Prevention Mark Riddle, Naval Medical Research Center Jan Vinjé, Centers for Disease Control and Prevention The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention, or the US Department of Health and Human Services. This work was funded in part by a grant from the Bill & Melinda Gates Foundation to the CDC Foundation. GLOBAL BURDEN OF NOROVIRUS AND PROSPECTS FOR VACCINE DEVELOPMENT | 1 Table of Contents 1. Executive summary ....................................................................3 2. Burden of disease and epidemiology 7 a. Burden 7 i. Global burden and trends of diarrheal disease in children and adults 7 ii. The role of norovirus 8 b. Epidemiology 9 i. Early childhood infections 9 ii. Risk factors, modes and settings of transmission 10 iii. Chronic health consequences associated with norovirus infection? 11 c. Challenges in attributing disease to norovirus 12 3. Norovirus biology, diagnostics and their interpretation for field studies and clinical trials..15 a. Norovirus virology 15 i. Genetic diversity, evolution and related challenges for diagnosis 15 ii. -

Non-Norovirus Viral Gastroenteritis Outbreaks Reported to the National Outbreak Reporting System, USA, 2009–2018 Claire P
Non-Norovirus Viral Gastroenteritis Outbreaks Reported to the National Outbreak Reporting System, USA, 2009–2018 Claire P. Mattison, Molly Dunn, Mary E. Wikswo, Anita Kambhampati, Laura Calderwood, Neha Balachandran, Eleanor Burnett, Aron J. Hall During 2009–2018, four adenovirus, 10 astrovirus, 123 The Study rotavirus, and 107 sapovirus gastroenteritis outbreaks NORS is a dynamic, voluntary outbreak reporting were reported to the US National Outbreak Reporting system. For each reported outbreak, health depart- System (annual median 30 outbreaks). Most were at- ments report the mode of transmission, number of tributable to person-to-person transmission in long-term confirmed and suspected cases, and aggregate epi- care facilities, daycares, and schools. Investigations of demiologic and demographic information as avail- norovirus-negative gastroenteritis outbreaks should in- able. NORS defines outbreaks as >2 cases of similar clude testing for these viruses. illness associated with a common exposure or epi- demiologic link (9). Health departments determine n the United States, ≈179 million cases of acute gas- reported outbreak etiologies on the basis of available troenteritis (AGE) occur annually (1). Norovirus is I laboratory, epidemiologic, and clinical data; specific the leading cause of AGE in the United States; other laboratory testing protocols vary by health depart- viral causes include adenovirus (specifically group F ment. Outbreak etiologies are considered confirmed or types 40 and 41), astrovirus, sapovirus, and rotavi- when >2 laboratory-confirmed cases are reported rus (2,3). These viruses are spread primarily through and considered suspected when <2 laboratory-con- the fecal–oral route through person-to-person contact firmed cases are reported. Outbreaks are considered or through contaminated food, water, or fomites (4–8). -

Viruses in Transplantation - Not Always Enemies
Viruses in transplantation - not always enemies Virome and transplantation ECCMID 2018 - Madrid Prof. Laurent Kaiser Head Division of Infectious Diseases Laboratory of Virology Geneva Center for Emerging Viral Diseases University Hospital of Geneva ESCMID eLibrary © by author Conflict of interest None ESCMID eLibrary © by author The human virome: definition? Repertoire of viruses found on the surface of/inside any body fluid/tissue • Eukaryotic DNA and RNA viruses • Prokaryotic DNA and RNA viruses (phages) 25 • The “main” viral community (up to 10 bacteriophages in humans) Haynes M. 2011, Metagenomic of the human body • Endogenous viral elements integrated into host chromosomes (8% of the human genome) • NGS is shaping the definition Rascovan N et al. Annu Rev Microbiol 2016;70:125-41 Popgeorgiev N et al. Intervirology 2013;56:395-412 Norman JM et al. Cell 2015;160:447-60 ESCMID eLibraryFoxman EF et al. Nat Rev Microbiol 2011;9:254-64 © by author Viruses routinely known to cause diseases (non exhaustive) Upper resp./oropharyngeal HSV 1 Influenza CNS Mumps virus Rhinovirus JC virus RSV Eye Herpes viruses Parainfluenza HSV Measles Coronavirus Adenovirus LCM virus Cytomegalovirus Flaviviruses Rabies HHV6 Poliovirus Heart Lower respiratory HTLV-1 Coxsackie B virus Rhinoviruses Parainfluenza virus HIV Coronaviruses Respiratory syncytial virus Parainfluenza virus Adenovirus Respiratory syncytial virus Coronaviruses Gastro-intestinal Influenza virus type A and B Human Bocavirus 1 Adenovirus Hepatitis virus type A, B, C, D, E Those that cause -
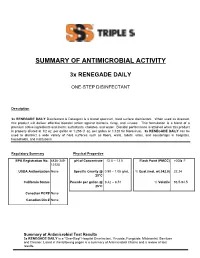
Summary of Antimicrobial Activity
SUMMARY OF ANTIMICROBIAL ACTIVITY 3x RENEGADE DAILY ONE-STEP DISINFECTANT Description 3x RENEGADE DAILY Disinfectant & Detergent is a broad spectrum, hard surface disinfectant. When used as directed, this product will deliver effective biocidal action against bacteria, fungi, and viruses. This formulation is a blend of a premium active ingredients and inerts: surfactants, chelates, and water. Biocidal performance is attained when this product is properly diluted at 1/2 oz. per gallon or 1:256 (1 oz. per gallon or 1:128 for Norovirus). 3x RENEGADE DAILY can be used to disinfect a wide variety of hard surfaces such as floors, walls, toilets, sinks, and countertops in hospitals, households, and institutions. Regulatory Summary Physical Properties EPA Registration No. 6836-349- pH of Concentrate 12.0 – 13.5 Flash Point (PMCC) >200 F 12120 USDA Authorization None Specific Gravity @ 0.98 – 1.05 g/mL % Quat (mol. wt.342.0) 22.24 25°C California Status Pounds per gallon @ 8.42 – 8.51 % Volatile 93.5-94.5 25°C Canadian PCP# None Canadian Din # None Summary of Antimicrobial Test Results 3x RENEGADE DAILY is a "One-Step" Hospital Disinfectant, Virucide, Fungicide, Mildewstat, Sanitizer and Cleaner. Listed in the following pages is a summary of Antimicrobial Claims and a review of test results. Claim: Contact time: Organic Soil: Water Conditions: Disinfectant Varies 5% 250ppm as CaCO3 Test Method: AOAC Germicidal Spray Test Organism Contact Dilution Time (Min) 868 ppm (1/2oz. per Acinetobacter baumannii 3 Gal) Bordetella bronchiseptica 3 868 ppm Bordetella pertussis 3 868 ppm Campylobacter jejuni 3 868 ppm Enterobacter aerogenes 3 1736 PPM (1 oz per Gal) Enterococcus faecalis 3 868 ppm Enterococcus faecalis - Vancomycin resistant [VRE] 3 868 ppm Escherichia coli 3 868 ppm Escherichia coli [O157:H7] 3 868 ppm Escherichia coli ESBL – Extended spectrum beta- 868 ppm 10 lactamase containing E. -
Emergence of Pathogenicity in Lagoviruses: Evolution from Pre-Existing Nonpathogenic Strains Or Through a Species Jump?
OPINION Emergence of Pathogenicity in Lagoviruses: Evolution from Pre-existing Nonpathogenic Strains or through a Species Jump? Pedro José Esteves1,2,3*, Joana Abrantes1, Stéphane Bertagnoli4,5, Patrizia Cavadini6, Dolores Gavier-Widén7, Jean-Sébastien Guitton8, Antonio Lavazza9, Evelyne Lemaitre10,11, Jérôme Letty8, Ana Margarida Lopes1,2, Aleksija S. Neimanis7, Nathalie Ruvoën-Clouet12, Jacques Le Pendu12, Stéphane Marchandeau8, Ghislaine Le Gall-Reculé10,11 a11111 1 InBIO—Research Network in Biodiversity and Evolutionary Biology, CIBIO, Campus de Vairão, Universidade do Porto, Vairão, Portugal, 2 Departamento de Biologia, Faculdade de Ciências da Universidade do Porto, Porto, Portugal, 3 CESPU, Instituto de Investigação e Formação Avançada em Ciências e Tecnologias da Saúde, Gandra, Portugal, 4 UMR 1225, INRA, Toulouse, France, 5 INP-ENVT, University of Toulouse, Toulouse, France, 6 Proteomic Unit, Istituto Zooprofilattico Sperimentale della Lombardia e dell’Emilia Romagna “Bruno Ubertini”, Brescia, Italy, 7 Department of Pathology and Wildlife Diseases, National Veterinary Institute, Uppsala, Sweden, 8 Department of Studies and Research, National Hunting and Wildlife Agency (ONCFS), Nantes, France, 9 Virology Unit, Istituto Zooprofilattico Sperimentale della Lombardia e dell’Emilia Romagna “Bruno Ubertini”, Brescia, Italy, 10 Avian and Rabbit Virology OPEN ACCESS Immunology Parasitology Unit, Ploufragan-Plouzané Laboratory, French Agency for Food, Environmental Citation: Esteves PJ, Abrantes J, Bertagnoli S, and Occupational Health & Safety (Anses), Ploufragan, France, 11 European University of Brittany, Rennes, Cavadini P, Gavier-Widén D, Guitton J-S, et al. France, 12 Inserm U892; CNRS, UMR 6299University of Nantes, Nantes France (2015) Emergence of Pathogenicity in Lagoviruses: * [email protected] Evolution from Pre-existing Nonpathogenic Strains or through a Species Jump? PLoS Pathog 11(11): e1005087. -

Package Insert Astrovirus, Sapovirus Open System PCR Reagents 450-052-Series
Package Insert Astrovirus, Sapovirus Open System PCR Reagents 450-052-Series For Research Use Only Research use only reagents are not intended for human or animal diagnostic use. It is the responsibility of the end user to determine the performance of the reagents in an appropriately designed validation study for their intended use. The Astrovirus, Sapovirus real-time PCR-based detection reagent is manufactured and packaged as an open system reagent (OSR) for use with open system platforms and has to be validated by the user. Examples of open system platforms are the Applied Biosystems QuantStudioTM 5 (Design & Analysis software version 1.5.1 or later), Applied Biosystems 7500 Fast Dx (SDS software version 1.4 or later), Bio-Rad CFX96 TouchTM or CFX384 TouchTM (Maestro software version 1.1 or later) real-time PCR platforms. PLEASE READ ENTIRE PACKAGE INSERT BEFORE PROCEEDING TO USE THE OSR. PRODUCT OVERVIEW The BioGX Sample-Ready™ OSR has been formulated in lyophilized format for the multiplex real-time PCR-based detection of RNA from Astrovirus (ORF1a gene1), Sapovirus (polymerase/capsid junction gene1) and a synthetic single stranded RNA [Internal Amplification Control (IAC)/Sample Processing Control (SPC)]. The synthetic single stranded RNA serves as both a sample processing control and an internal amplification control. Two different formats for the lyophilized Sample-Ready OSR kits are available: 1. BD MAXTM System REF 450-052-C-MAX 2. ABI QuantStudioTM 5, ABI 7500 Fast Dx, Bio-Rad CFX96 TouchTM and Bio-Rad CFX384 TouchTMPlatforms REF 450-052-LMP Note: BD MAXTM System OSR (450-052-C-MAX) contains all PCR primers, probes, enzymes, dNTPs, MgCl2, buffers, and other components required for PCR reaction.