Ambulance Station Newapproachcomprehensive Report
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Toronto Paramedic Services
CAPITAL PROGRAM SUMMARY 2015 – 2024 CAPITAL BUDGET AND PLAN OVERVIEW Toronto Paramedic Services (PS) is responsible for providing 24-hour emergency pre-hospital and out-of- hospital medical care and transportation to individuals experiencing injury or illness. Toronto Paramedic Services currently operates 45 ambulance stations which includes 5 service district centres, and the Toronto Paramedic Services' headquarters that have a total area of just over 289,056 sq. ft. and an Toronto Paramedic Services estimated replacement value of $122.569 million. toronto.ca/budget 2015 The 2015–2024 Capital Budget and Plan of $71.123 million focuses on the lifecycle replacement of major medical and Highlights communications equipment as well as addresses the increase in service demands due to a growing and aging Toronto population Overview & Recommendations by investing in the purchase of additional ambulance vehicles I: 10-Year Capital Plan 6 and construction of 3 new stations that will provide multi- function facilities for staff and vehicles to improve the efficient II: 2015 Capital Budget 16 use of City land/assets and more effective use of paramedic III: Issues for Discussion 20 resources. Appendices: 1. 2014 Performance 24 2. 10-Year Capital Plan Summary 27 3. 2015 Capital Budget; 2016-2024 Capital Plan 28 4. 2015 Cash Flow & Future Year Commitments 29 5. 2015 Capital Projects with Financing Detail 30 6. 2015 Reserve / Reserve Fund Review 31 toronto.ca/budget 2015 Page 2 2015 Capital Budget Toronto Paramedic Services Capital Spending and Financing Where does the money go? The 2015–2024 Capital Budget and Plan totals 2015-2024 Capital Budget and Plan by $71.123 million that will fund the following Expenditures Category major capital projects over the 10-year period: . -

PS COMMITTEE #2 April 29, 2021 Revised Worksession MEMORANDUM April 26, 2021 TO
PS COMMITTEE #2 April 29, 2021 Revised Worksession M E M O R A N D U M April 26, 2021 TO: Public Safety Committee FROM: Susan J. Farag, Legislative Analyst SUBJECT: Worksession: FY22 Operating Budget and FY21-26 CIP Amendments Montgomery County Fire and Rescue Service (MCFRS) PURPOSE: Vote on Recommendations for Council’s Consideration Those expected for this worksession: Chief Scott Goldstein, MCFRS Dominic Del Pozzo, Division Chief, MCFRS Rachel Silberman, Office of Management and Budget (OMB) Budget Summary • There are no proposed service cuts in the FY22 Recommended Operating Budget. • There are 10 new Paramedic Training Positions that help address understaffing. • There are one new Paramedic Chase Car and one new Daywork Ambulance to enhance EMS Service Delivery. • The Fire Department audit will be split into two studies, one for operations and one for racial equity and social justice, at a total cost of $200,000. • The Executive’s March 15 amendments to the Capital Improvements Program has minor adjustments to several projects. Overview For FY22, the County Executive recommends total expenditures of $232,685,066 for MCFRS, a 3.5% increase from the FY21 Approved Budget of 224,995,408. FY20 FY21 FY22 CE % Change Actual Approved Recommended FY21-22 Expenditures by fund Fire Tax District $244,508,043 $224,869,427 $232,685,066 3.5% Grant Fund $3,355,713 $125,981 $0 -100.0% TOTAL Expenditures $247,863,756 $224,995,408 $232,685,066 3.4% Positions: Full-time 1317 1318 1,327 0.7% Part-time 0 0 0 -- TOTAL Positions 1317 1318 1327 0.7% TOTAL FTEs 1318.26 1319.26 1,328.26 0.7% The FY20 County Executive’s recommendation is a net increase of $7,815,639. -

Evaluation of Paramedics Tasks and Equipment to Control the Risk of Musculoskeletal Injury
FINDING SOLUTIONS Research at the Workers’ Compensation Board 1150-20 B 1999 (99FS-14) EVALUATION OF PARAMEDICS TASKS AND EQUIPMENT TO CONTROL THE RISK OF MUSCULOSKELETAL INJURY Ambulance Paramedics of British Columbia © 2001 Workers’ Compensation Board of British Columbia. All rights reserved. The Workers’ Compensation Board of B.C. encourages the copying, reproduction, and distribution of this document to promote health and safety in the workplace, provided that the Workers’ Compensation Board of B.C. is acknowledged. However, no part of this publication may be copied, reproduced, or distributed for profit or other commercial enterprise or may be incorporated into any other publication without written permission of the Workers’ Compensation Board of B.C. Additional copies of this publication may be obtained by contacting: Workers’ Compensation Board of British Columbia Publications & Videos Department 6711 Elmbridge Way Richmond, BC V7C 4N1 Phone (604) 276-3068 / Fax (604) 279-7406 Toll-free within BC – 1-800-661-2112 1150-20 A1999 (99FS-14 Evaluation of Paramedics Tasks and Equipment to Control the Risk of Musculoskeletal Injury Issue: Reducing the risk of musculoskeletal injury for paramedics. Agency: Ambulance Paramedics of British Columbia CUPE Local 873 Representative: Donald Cragg Funding: $49,500.00 Context: A paramedic’s work environment is often unpredictable. The confined space of the patient compartment, the task requirements, and the configuration of equipment within the patient compartment contribute to the risk of MSI. Currently there is little information regarding design guidance for ambulances and related equipment that is based on prevention of MSI through the application of ergonomic principles. Objective: To evaluate aspects of the main stretcher and patient compartment of the ambulance that contribute to the risk of musculoskeletal injury for paramedics, to priortize issues and suggest possible solutions, and to evaluate two of the suggested solutions. -
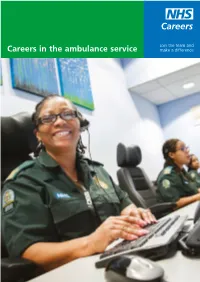
Careers in the Ambulance Service Make a Difference Careers in Healthcare Science 2
Join the team and Careers in the ambulance service make a difference Careers in healthcare science 2 Welcome to the NHS The NHS offers a huge range of exciting and challenging opportunities for people who are passionate about making a difference. With more than 350 different careers on offer, there is a job for you no matter what your interests, skills or qualifications. What’s more, you’ll be given every opportunity to build on your skills and learn new ones as part of the Career Framework – a system that demonstrates our commitment to skills development. See pages 10 and 11 for more information about this. Scientists, accountants, porters, psychologists, nurses, information technologists and estate managers, to name but a few, are all needed to ensure the smooth running of the NHS. These people, and many more, work together as a team to deliver the very best care for our patients. To find out more about becoming a member of the NHS team, call 0345 60 60 655, email [email protected] or visit www.nhscareers.nhs.uk We look forward to hearing from you! Contents 2 The NHS – a rewarding place to work 12 What opportunities are available? Benefits Ambulance care assistants Pay and conditions Assistant practitioners Work-life balance Call handlers Emergency medical dispatchers 6 Your career in the ambulance service Paramedics Patient transport services controllers 10 Career Framework Senior paramedics Developing your career in the NHS 16 Getting started NHS Constitution Entry level/assistant roles Graduate opportunities and approved courses Work placements 19 What’s your next step? Foreword In this booklet you’ll learn about the exciting range Whatever your academic background, preferences of opportunities that today’s ambulance service has and interests, if you would like to help others in a to offer. -

3201 Ambulance Permits
Administrative Policy 3201 Effective Expires April 1, 2021 March 31, 2022 Policy: Approval: Medical Director Signed Ambulance Permits Reza Vaezazizi, MD Applies To: Approval: EMS Administrator Signed Transport Services, EMS System Trevor Douville PURPOSE To establish criteria for permitting ambulance operations within Riverside County. AUTHORITY California Health and Safety Code - Division 2.5: Emergency Medical Services [1797.200.] California Health and Safety Code - Division 2.5: Emergency Medical Services [1797.222.] County of Riverside Ordinance 756 (Ambulance Ordinance) Initial Permit Application To receive an ambulance service permit, the applicant must: 1. Complete and submit an interest letter in the form of an ambulance permit pre-application form. The form can be found here: https://rivcoems.org/Programs/Ambulance-Permits 2. Complete the Riverside County Emergency Medical Services Agency (REMSA) ambulance permit application. 3. Initial ambulance permit applications are accepted from July 1 thru September 30 each year. Completed application must be submitted to REMSA no later than September 30. 4. All BLS services must establish an EMT AED program which meets or exceeds the requirements of the REMSA Policy for EMT AED Service Provider. 5. Each ambulance will utilize two-way communications equipment, as specified by REMSA, capable of direct two- way voice communications with the first response agencies and ALS transport services operating within the Riverside County EMS system; and with REMSA. 6. Each ground ambulance service must establish at least one ambulance station within Riverside County. a. Each ambulance based at that location must be available as a disaster resource within one hour of REMSA request. b. Each ambulance station will comply with all applicable zoning, building, and occupational health and safety regulations. -

Elko County Human Services Employment Opportunity Announcement
Position opens: 11/23/16 Elko County Human Services Employment Opportunity Announcement POSITION: Assistant Ambulance Director SALARY: Step 1 - $23.3173 Step 2 - $24.0168 Step 3 - $24.7373 APPLICATION DEADLINE: December 2, 2016 Grade 524/22702 Elko County is accepting applications for the position of Assistant Ambulance Director. This is an hourly position within the Elko County Ambulance Services responsible for assisting the Ambulance Director with day-to-day management of the Ambulance Service. This includes duties as a responding paramedic and supporting the comprehensive administrative, operational, and clinical functions of the department. Must be a current ECAS Paramedic to be eligible for promotion. It is the intent to fill this position by intra-department promotion. Applications outside of the Elko County Ambulance Department will not be accepted. 100% PERS Retirement Minimal Fee for Employee Health, Vision, Dental and Life Insurance Obtain an application and full job description at www.elkocountynv.net. Elko County Human Services 540 Court St, Suite 105 (Physical Address) 571 Idaho St. (Mailing Address) Elko, NV 89801 (775) 738-4375 phone (775) 738-5984 fax Elko County is an Equal Opportunity Provider and Employer In compliance with applicable laws reasonable accommodations may be provided for qualified individuals with a disability who require and request such accommodations. ASSISTANT AMBULANCE DIRECTOR DEFINITION This is an hourly position within the Elko County Ambulance Services responsible for assisting the Ambulance Director with day-to-day management of the Ambulance Service. This includes duties as a responding paramedic and supporting the comprehensive administrative, operational, and clinical functions of the department. -

CMS Cost Data Collection Round 1 Master File
Medicare Ground Ambulance Data Collection Ground Ambulance Providers and Suppliers Selected to Submit Data in Year 1 Note: This list consists of randomly selected ground ambulance providers and suppliers that submitted and were paid for at least one ground ambulance claim to Medicare in 2017, the most recent year for which CMS has complete claims data, using the NPI listed. We are aware that some of the organizations listed may not be enrolled in or may not be furnishing ground ambulance services at present. However, all ambulance organizations on this list must confirm with their MAC the starting date for their data collection period. Please see the Medicare Ground Ambulance webpage for more details concerning this data collection. This website is available at: https://www.cms.gov/Center/Provider-Type/Ambulances-Services-Center.html If you have questions concerning this data collection please email us at: [email protected] Sampled NPPES National Mailing Provider Address Identifier (NPI) NPPES Organization Name State 1023069622 MUNICIPALITY OF ANCHORAGE AK 1225101041 NORTON SOUND HEALTH CORPORATION AK 1376598755 TRI -VALLEY VOLUNTEER FIRE DEPARTMENT AK 1407928898 CITY OF ANDERSON AK 1477687374 MUNICIPALITY OF NENANA AK 1619005683 CITY OF BETHEL AK 1720039076 FAIRBANKS NORTH STAR BOROUGH AK 1871754473 LIFEMED ALASKA, LLC AK 1013098300 DEKALB COUNTY HOSPITAL ASSOCIATION AL 1043746902 LIFEGUARD AMBULANCE SERVICE LLC AL 1073931515 LIFEGUARD AMBULANCE SERVICE LLC AL 1114090909 CLAY COUNTY RESCUE SQUAD AL 1134377062 NORTHSTAR -
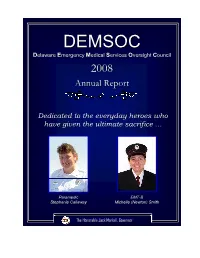
2008 DEMSOC Annual Report
DEDEMSOMSOCC Delaware Ememergeencyncy Medical Serviviceces Oversight Council 20082008 AnnualAnnual ReportReport Dedicated to the everyday heroes who have given the ultimate sacrifice … ParaParamedic EMT-B Stephanianie Callllaway Michelchellele ((NewNewttoon) Smith The Honorable Jack Markelell,, GoGovernor Page Left Blank Intentionally April 15, 2009 To the Citizens of Delaware: On Behalf of Governor Jack Markell and the Delaware Emergency Medical Services Oversight Council (DEMSOC), I am pleased to present the 2008 DEMSOC Annual Report. DEMSOC was created in 1999 to promote the continuous development and improvement of our Emergency Medical Services (EMS) System. There can be no greater reminder of the sacrifice that the men and women of Delaware’s Emergency Medical Community make than the line-of-duty deaths of Stephanie Calloway and Michelle Smith. This year’s DEMSOC report is dedicated to the memory of Stephanie and Michelle and all who have given the ultimate sacrifice while providing care to someone else. The membership of DEMSOC includes professionals from several EMS provider agencies, representatives from agencies that frequently work with and support EMS, and private citizens knowledgeable in the delivery of EMS care. The Council meets several times throughout the year to address current issues and provide support for developing workable solutions to those issues. The purpose of this report is to inform others about Delaware’s EMS system and increase awareness of the issues that most directly affect the delivery of EMS service and the quality of EMS patient care. Throughout the year we have witnessed great achievements in the EMS community and this report attempts to capture those successes as well as to build the framework for addressing the challenges that lie ahead. -
![Final Report Town of Northampton EMS Stu[...]](https://docslib.b-cdn.net/cover/7832/final-report-town-of-northampton-ems-stu-3617832.webp)
Final Report Town of Northampton EMS Stu[...]
Ron Graner Public Safety Consultant Strategic Planning For Efficiency Effectiveness & Safety 19 Gazebo Path Fayetteville NY 13066 10/14/19 Final Report A Comprehensive Review of Emergency Medical Services Northampton Ambulance Service Prepared For the Town of Northampton New York Primary Town of Northampton Contact William H. Gritsavage Councilman Town of Northampton 412 S. Main St, PO Box 479, Northville, NY 12134 Final Report EMS Services Study for Town of Northampton NY Ron Graner Public Safety Consultant Phone: 770 630 0104 Email: [email protected] HTTP://FIRERESCUECONSULTING.COM Page 1 of 127 Table of Contents Table of Contents ............................................................................................................................. 2 Project Goals .................................................................................................................................... 5 Disclaimer ........................................................................................................................................ 5 Acknowledgements .......................................................................................................................... 6 Executive Summary ......................................................................................................................... 7 Immediate Actions Required To Assure Efficient, Effective & Safe Emergency Medical Services in Northampton ............................................................................................................................. -

Cosumnes CSD Fire Department—Standards of Cover and Headquarters Services Assessment Volume 2—Technical Report
Folsom (Sacramento), CA Management Consultants Standards of Cover and Headquarters Services Assessment for the Cosumnes CSD Fire Department Volume 2 of 3 – Technical Report May 26, 2015 2250 East Bidwell St., Ste #100 Folsom, CA 95630 (916) 458-5100 Fax: (916) 983-2090 This page was intentionally left blank Cosumnes CSD Fire Department—Standards of Cover and Headquarters Services Assessment Volume 2—Technical Report TABLE OF CONTENTS Section Page VOLUME 1 of 3 – Executive Summary (separately bound) VOLUME 2 of 3 – Standards of Cover and Headquarters Services Assessment Technical Report (this volume) Section 1—Introduction and Background ...................................................................................1 1.1 Report Organization ........................................................................................ 1 1.2 Project Scope of Work .................................................................................... 2 1.3 District and Department Overview .................................................................. 4 1.4 Previous Studies of the Cosumnes Fire Department ....................................... 6 Section 2—Standards of Coverage Introduction ........................................................................7 2.1 Standards of Coverage Study Processes .......................................................... 7 Section 3—District Deployment Goals/Measures and Risk Assessment ................................11 3.1 Why Does the Department Exist and How Does it Deliver the Existing Fire -
A Feasibility Study of the Placement of an Emergency Medical Services Vehicle/Ambulance in Every County
Mississippi State Department of Health Division of Emergency Medical Services MSDH Report to House and Senate Public Health and Welfare Committees December 2001 Emergency Medical Services A Feasibility Study of the Placement of an Emergency Medical Services Vehicle/Ambulance in Every County in Mississippi, With Focus on Benton, Carroll, Greene and Smith Counties Jim Craig, State EMS Director Mississippi State Department of Health P.O. Box 1700, Jackson, Mississippi 39215-1700 (601) 576-7366 - Voice, (601) 576-7373 - Fax Introduction On a typical day in Mississippi, hundreds of people face medical emergencies that require immediate treatment before reaching a hospital. For these people, emergency medical services (EMS) systems B including a 911 telephone dispatch center, medical treatment by responding emergency personnel, and emergency transportation to a hospital B are the front line of care. In some situations, emergency services can be the difference between life and death. For example, chances of surviving a sudden cardiac arrest decrease an estimated 10 percent for every minute=s delay in treatment. People who need such emergency, prehospital care depend on well-trained personnel reaching them quickly, identifying the type of treatment they need, and, in the case of life-threatening situations such as cardiac arrest, administering needed life-sustaining treatment wherever the person may be. EMS systems are primarily local, but the state plays a major role in regulating them. The federal government has also adopted a role supporting and promoting efforts to improve EMS systems B for example, by making the improvement of EMS a national health priority. In its Healthy People 2010 initiative outlining health care improvement goals for the next decade, the Department of Health and Human Services (HHS) 2 established a goal of increasing the proportion of people who can be reached by EMS within 5 minutes in urban areas and within 10 minutes in rural areas. -
Wilbur Fire/EMS Department Policies and Procedures
Town of Wilbur FIRE AND EMS DEPARTMENT Updated April 2, 2008 1 LETTER OF RECEIPT AND NOTIFICATION I do hereby certify that I have read and understand the content of this policy and procedures manual. I understand that a copy of the policies and procedure manual is available in the Wilbur station and is available for my review. I further agree that I shall read any addition or revision to this manual at such time as it is posted in the stations. I further understand my responsibility to be obedient to these policies and to faithfully serve the citizens of Town of Wilbur Fire and EMS Department Fire and EMS Department in the discharge of my duties as a member to the best of my knowledge and ability. __________________________________________ Signature __________________________________________ Print Name __________________________________________ Date 2 TABLE OF CONTENTS COVER 1 RECIEPT AND NOTIFICATION 2 TABLE OF CONTENTS 3 HEADING 5 ORGANIZATIONAL TREE 6 ORGANIZATIONAL STRUCTURE 7 VOLUNTEER POSITION DECRIPTIONS 9 SECTION 1 INDIVIDUAL/MEMBER POLICIES MEMBERSHIP CRITERIA 15 ALL MEMBERS 16 OFFICERS 17 GENERAL CONDUCT 17 PUBLIC CONDUCT 19 INTOXICATING LIQUORS & DRUGS 19 TESTIMONY 19 CALL TO DUTY AND HOME TELEPHONES 19 SMOKING 20 LENDING OF NAMES TO COMMERCIAL ENTERPRISES 20 REWARDS FOR SERVICE RENDERED 20 PERSONAL BUSINESS 20 RETURN OF EQUIPMENT 20 FAMILIARITY WITH RULES AND ORDERS 20 MEMBERSHIP COMMITTEE 20 SECTION 2 ACCEPTANCE OF MEMBERS ACCEPTANCE OF MEMBERS 21 SECTION 3 DEPARTMENT PROCEDURES DISCRIMINATION 24 ORGANIZATION RECOGNITION