Comparative Efficacy of Caffeic Acid Phenethyl Ester (CAPE), Olopatadine Hydrochloride, and Dexamethasone Sodium Phosphate in Experimental Allergic Conjunctivitis*
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Prediction of Premature Termination Codon Suppressing Compounds for Treatment of Duchenne Muscular Dystrophy Using Machine Learning
Prediction of Premature Termination Codon Suppressing Compounds for Treatment of Duchenne Muscular Dystrophy using Machine Learning Kate Wang et al. Supplemental Table S1. Drugs selected by Pharmacophore-based, ML-based and DL- based search in the FDA-approved drugs database Pharmacophore WEKA TF 1-Palmitoyl-2-oleoyl-sn-glycero-3- 5-O-phosphono-alpha-D- (phospho-rac-(1-glycerol)) ribofuranosyl diphosphate Acarbose Amikacin Acetylcarnitine Acetarsol Arbutamine Acetylcholine Adenosine Aldehydo-N-Acetyl-D- Benserazide Acyclovir Glucosamine Bisoprolol Adefovir dipivoxil Alendronic acid Brivudine Alfentanil Alginic acid Cefamandole Alitretinoin alpha-Arbutin Cefdinir Azithromycin Amikacin Cefixime Balsalazide Amiloride Cefonicid Bethanechol Arbutin Ceforanide Bicalutamide Ascorbic acid calcium salt Cefotetan Calcium glubionate Auranofin Ceftibuten Cangrelor Azacitidine Ceftolozane Capecitabine Benserazide Cerivastatin Carbamoylcholine Besifloxacin Chlortetracycline Carisoprodol beta-L-fructofuranose Cilastatin Chlorobutanol Bictegravir Citicoline Cidofovir Bismuth subgallate Cladribine Clodronic acid Bleomycin Clarithromycin Colistimethate Bortezomib Clindamycin Cyclandelate Bromotheophylline Clofarabine Dexpanthenol Calcium threonate Cromoglicic acid Edoxudine Capecitabine Demeclocycline Elbasvir Capreomycin Diaminopropanol tetraacetic acid Erdosteine Carbidopa Diazolidinylurea Ethchlorvynol Carbocisteine Dibekacin Ethinamate Carboplatin Dinoprostone Famotidine Cefotetan Dipyridamole Fidaxomicin Chlormerodrin Doripenem Flavin adenine dinucleotide -

Allergies Your Amerigroup Community Care Patients May Experience a Pharmacy Claim Rejection When Prescribed Nonpreferred Products
Provider update Hot Tip: Allergies Your Amerigroup Community Care patients may experience a pharmacy claim rejection when prescribed nonpreferred products. To avoid additional steps or delays at the pharmacy, consider prescribing preferred products whenever possible. Utilization Management edits may apply to select preferred products. Coverage should be verified by reviewing the Preferred Drug List (PDL) on the Amerigroup provider website. The PDL is subject to change quarterly. Therapeutic class Preferred products Nonpreferred products Oral • Fexofenadine (generic Allegra) • Cetirizine (generic Zyrtec) antihistamines1 • Fexofenadine/ pseudoephedrine • Cetirizine/pseudoephedrine (generic Allegra-D) (generic Zyrtec D) • Loratadine (generic Claritin) • Zyrtec (cetirizine) • Loratadine/pseudoepherine • Zyrtec D (cetirizine/ (generic Claritin D) pseudoephedrine) • Clarinex (desloratadine) • Desloratadine (generic Clarinex) • Alegra (fexofenadine) • Allegra D (fexofenadine/ pseudoephedrine) • Levocetirizine (generic Xyzal) • Xyzal (levocetirizine) • Claritin (loratadine) • Claritin D (loratadine/ pseudoephedrine) Nasal steroids2 • OTC budesonide nasal spray • Flonase Sensimist (fluticasone (generic Rhinocort) furoate) • OTC Rhinocort Allergy • Flonase (fluticasone propionate) (budesonide) • Rx fluticasone propionate (generic • OTC fluticasone propionate Rx Flonase) (generic Flonase) • Mometasone furoate (generic • OTC triamcinolone acetonide Nasonex) (generic Nasacort) • Nasacort (triamcinolone acetonide) • Nasonex (mometasone furoate) • Omnaris -

Therapeutic Class Overview Intranasal Histamine H1-Receptor Antagonists (Antihistamines)
Therapeutic Class Overview Intranasal Histamine H1-receptor Antagonists (Antihistamines) Therapeutic Class • Overview/Summary: The four intranasal histamine-1 receptor antagonist (H1-antihistamines) products that are approved for the management of rhinitis include azelastine (Astelin®, Astepro®), olopatadine (Patanase®) and azelastine hydrochloride/fluticasone propionate (Dymista®).1-4 Allergic rhinitis, often referred to as rhinosinusitis, is a condition characterized by episodes of sneezing, rhinorrhea, nasal congestion, itchy and watery eyes, nose and palate. Other common symptoms may include cough, postnasal drip, and fatigue.5 Allergic rhinitis is also referred to in terms of the cyclical or persistent nature of symptoms. Seasonal allergic rhinitis is that which occurs at a particular time of the year; whereas, perennial allergic rhinitis describes symptoms that are present year round. Mast cell activation, histamine release, prostaglandin and leukotrienes propagation, along with other cytokine mediators (e.g., platelet activating factor, tumor necrosis factor, transforming growth factor beta, eosinophils, etc.) are known to play a direct role in the disease pathology and symptomatology.6 Allergic rhinitis may be classified by its intermittent or persistent pattern and by severity (mild or moderate to severe). Intermittent patterns involve the presence of symptoms for less than four days per week or for less than four weeks; whereas persistent patterns entail the presence of symptoms more than four days per week and for more than four weeks. Conditions associated with allergic rhinitis include: allergic conjunctivitis, sinusitis, asthma, atopic dermatitis, oral allergy syndrome, eustachian tube dysfunction, sleep disturbances, nasal obstruction leading to anosmia, and migraine headaches.5,7 Astelin® nasal spray is the only agent within the class that is available generically. -

The Basics of Pharmacology
THE BASICS OF PHARMACOLOGY Endocrine, Musculoskeletal, Genitourinary, Ear And Eye Systems Jassin M. Jouria, MD Dr. Jassin M. Jouria is a practicing Emergency Medicine physician, professor of academic medicine, and medical author. He graduated from Ross University School of Medicine and has completed his clinical clerkship training in various teaching hospitals throughout New York, including King’s County Hospital Center and Brookdale Medical Center, among others. Dr. Jouria has passed all USMLE medical board exams, and has served as a test prep tutor and instructor for Kaplan. He has developed several medical courses and curricula for a variety of educational institutions. Dr. Jouria has also served on multiple levels in the academic field including faculty member and Department Chair. Dr. Jouria continues to serve as a Subject Matter Expert for several continuing education organizations covering multiple basic medical sciences. He has also developed several continuing medical education courses covering various topics in clinical medicine. Recently, Dr. Jouria has been contracted by the University of Miami/Jackson Memorial Hospital’s Department of Surgery to develop an e- module training series for trauma patient management. Dr. Jouria is currently authoring an academic textbook on Human Anatomy & Physiology. ABSTRACT The science of pharmacology and the responsibility relationship building with patients are important elements of a health professional’s clinical knowledge and skills to provide safe and appropriate pharmacotherapeutic regimens in everyday practice. Interdisciplinary members of the health team are required to continually interpret specific patient health data to implement and evaluate outcomes of medication treatment. All health clinicians are increasingly relying on practice guidelines and the applied specialized training of health team members when obtaining the patient health history to improve therapeutic medication regimens, avoid adverse effects, and to safely and effectively treat a disease state. -

Protective Effect of Lodoxamide on Hepatic Steatosis Through GPR35 T ⁎ So-Yeon Nam, Soo-Jin Park, Dong-Soon Im
Cellular Signalling 53 (2019) 190–200 Contents lists available at ScienceDirect Cellular Signalling journal homepage: www.elsevier.com/locate/cellsig Protective effect of lodoxamide on hepatic steatosis through GPR35 T ⁎ So-Yeon Nam, Soo-Jin Park, Dong-Soon Im College of Pharmacy, Pusan National University, Busan 609-735, Republic of Korea ARTICLE INFO ABSTRACT Keywords: Although GPR35 is an orphan G protein-coupled receptor, synthetic agonists and antagonists have been de- GPR35 veloped. Recently, cromolyn, a mast cell stabilizer, was reported as an agonist of GPR35 and was shown to Steatosis exhibit antifibrotic effects through its actions on hepatocytes and stellate cells. In this study, the roleofGPR35in Lodoxamide hepatic steatosis was investigated using an in vitro model of liver X receptor (LXR)-mediated hepatocellular Hepatocyte steatosis and an in vivo model of high fat diet-induced liver steatosis. GPR35 was expressed in Hep3B human Fatty liver hepatoma cells and mouse primary hepatocytes. A specific LXR activator, T0901317, induced lipid accumulation GPCR in Hep3B cells. Lodoxamide, the most potent agonist of GPR35, inhibited lipid accumulation in a concentration- dependent manner. The protective effect of lodoxamide was inhibited by a specific GPR35 antagonist, CID2745687, and by siRNA-mediated knockdown of GPR35. The expression of SREBP-1c, a key transcription factor for lipid synthesis, was induced by T0901317 and the induction was inhibited by lodoxamide. Through the use of specific inhibitors of cellular signaling components, the lodoxamide-induced inhibition of lipid accu- mulation was found to be mediated through p38 MAPKs and JNK, but not through Gi/o proteins and ERKs. Furthermore, the protective effect of lodoxamide was confirmed in mouse primary hepatocytes. -

National PBM Drug Monograph Epinastine (Elestat™) May 2004 VHA Pharmacy Benefits Management Strategic Healthcare Group and the Medical Advisory Panel
National PBM Drug Monograph Epinastine (Elestat™) May 2004 VHA Pharmacy Benefits Management Strategic Healthcare Group and the Medical Advisory Panel EXECUTIVE SUMMARY • Antihistamine ophthalmic drops provide quick relief from allergic conjunctivitis (AC) symptoms such as itching and redness, without the potential adverse effects associated with systemic absorption. • Epinastine is the fourth ophthalmic antihistamines/mast cell stabilizer approved for the itching associated with AC. Other ophthalmic preparations for allergic conjunctivitis include antihistamines, mast cell stabilizers, nonsteroidal anti-inflammatory agents (NSAIDs), corticosteroids, decongestants, and decongestant/antihistamines. • An ideal agent would offer improved efficacy and safety, reduce polypharmacy as a combination product or through replacing oral agents, and provide evidence for chronic AC prevention. INTRODUCTION1 The purposes of this monograph are to (1) evaluate the available evidence of safety, tolerability, efficacy, cost, and other pharmaceutical issues that would be relevant to evaluating epinastine ophthalmic solution for possible addition to the VA National Formulary (VANF); (2) define its role in therapy; and (3) identify parameters for its rational use in the VA. PHARMACOLOGY/PHARMACOKINETICS1, 2 Antihistamines are receptor antagonists used to avoid the inflammatory effects of histamine. Taken orally, these agents have been shown to be effective for treating allergic symptoms such as pruritis (itching). Epinastine in particular has been found to have a rapid onset of action.3 Topical antihistamine eye drops provide relief from ocular symptoms without systemic absorption or related adverse events, allowing for the combination of oral and topical agents when indicated. Ophthalmic antihistamine/mast cell stabilizers such as epinastine combine H1-receptor actions to block ocular itching and redness with H2-receptor affinity. -

Alphabetical Listing of ATC Drugs & Codes
Alphabetical Listing of ATC drugs & codes. Introduction This file is an alphabetical listing of ATC codes as supplied to us in November 1999. It is supplied free as a service to those who care about good medicine use by mSupply support. To get an overview of the ATC system, use the “ATC categories.pdf” document also alvailable from www.msupply.org.nz Thanks to the WHO collaborating centre for Drug Statistics & Methodology, Norway, for supplying the raw data. I have intentionally supplied these files as PDFs so that they are not quite so easily manipulated and redistributed. I am told there is no copyright on the files, but it still seems polite to ask before using other people’s work, so please contact <[email protected]> for permission before asking us for text files. mSupply support also distributes mSupply software for inventory control, which has an inbuilt system for reporting on medicine usage using the ATC system You can download a full working version from www.msupply.org.nz Craig Drown, mSupply Support <[email protected]> April 2000 A (2-benzhydryloxyethyl)diethyl-methylammonium iodide A03AB16 0.3 g O 2-(4-chlorphenoxy)-ethanol D01AE06 4-dimethylaminophenol V03AB27 Abciximab B01AC13 25 mg P Absorbable gelatin sponge B02BC01 Acadesine C01EB13 Acamprosate V03AA03 2 g O Acarbose A10BF01 0.3 g O Acebutolol C07AB04 0.4 g O,P Acebutolol and thiazides C07BB04 Aceclidine S01EB08 Aceclidine, combinations S01EB58 Aceclofenac M01AB16 0.2 g O Acefylline piperazine R03DA09 Acemetacin M01AB11 Acenocoumarol B01AA07 5 mg O Acepromazine N05AA04 -

Supratarsal Injection of Triamcinolone Acetonide in the Treatment of Refractory Vernal Keratoconjunctivitis
Original Article SUPRATARSAL INJECTION OF TRIAMCINOLONE ACETONIDE IN THE TREATMENT OF REFRACTORY VERNAL KERATOCONJUNCTIVITIS , † Davood Aghadoost, * MD; and Mohammad Zare,** MD *Department of Ophthalmology, Kashan University of Medical Sciences, Kashan, ** Department of Ophthalmology, Shaheed Beheshti University of Medical Sciences, Tehran, Iran cold compresses, artificial tears, topical vasoconstrictors, BACKGROUND—Vernal keratoconjunctivitis (VKC) 1 cases are often resistant to conventional treatments. We or topical antihistamines. More severe cases may need aimed to assess the effect of supratarsal injection of topical nonsteroidal anti inflammatory drugs triamcinolone acetonide in these patients. (NSAID), or topical steroids, mast cell stabilizers, or PATIENTS AND METHODS—Sixteen patients (32 eyes) with severe VKC, and resistant to conventional even oral steroids and cyclosporin. More recently, method of treatments were selected and underwent topical ketotifen fumarate, mipragoside levocabastatine injection of 0.5 mL triamcinolone acetonide in supratarsal area (in conjuctival side of upper lid) and hydrochloride, lodoxamide tromethamine, excimer were followed up for 54 months. The results were laser, and surgical therapy have also been used.4 – 11 analyzed with SPSS program with 95% confidence These conventional methods of treatment may not interval. RESULTS—Relief of symptoms (burning, itching, be effective in patients with giant papillae, severe lacrimation and photophobia, ropy discharge) was limbal involvement, or corneal shield's ulcer. And dramatically seen in all patients, in first few days. Size therefore, the patients are severely debilitated and of giant papillae, thickening of limbus, vascularization 4 – 14 of cornea (pannus) decreased in the first month. can not live their daily routine. Recurrence of disease was seen in 2 (12.5%) patients Because of ineffective conventional therapeutic after one month. -
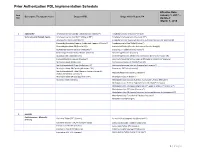
Prior Authorization PDL Implementation Schedule
Prior Authorization PDL Implementation Schedule Effective Date: Item January 1, 2017 – Descriptive Therapeutic Class Drugs on PDL Drugs which Require PA Nbr Updated: March 1, 2018 1 ADD/ADHD Amphetamine Salt Combo Tablet ( Generic Adderall®) Amphetamine ODT (Adzenys® XR ODT) Stimulants and Related Agents Amphetamine Salt Combo ER (Adderall XR®) Amphetamine Suspension (Dyanavel XR®) Atomoxetine Capsule (Strattera®) Amphetamine Salt Combo ER (Generic; Authorized Generic for Adderall XR) Dexmethylphenidate (Generic; Authorized Generic of Focalin®) Amphetamine Sulfate Tablet (Evekeo®) Dexmethylphenidate ER (Focalin XR®) Armodafinil Tablet (Generic; Authorized Generic; Nuvigil®) Dextroamphetamine Solution (Procentra®) Clonidine ER Tablet (Generic; Kapvay®) Dextroamphetamine Sulfate Tablet (Generic) Dexmethylphenidate (Focalin®) Guanfacine ER Tablet (Generic) Dexmethylphenidate XR (Generic; Authorized Generic for Focalin XR) Lisdexamfetamine Capsule (Vyvanse®) Dextroamphetamine Sulfate Capsule ER (Generic; Dexedrine®Spansule) Methylphenidate IR (Generic) Dextroamphetamine IR Tablet (Zenzedi®) Methylphenidate ER Chew (Quillichew ER®) Dextroamphetamine Solution (Generic for Procentra®) Methylphenidate ER Capsule (Metadate CD®) Guanfacine ER Tablet (Intuniv®) Methylphenidate ER Tablet (Generic; Generic Concerta®; Methamphetamine (Generic; Desoxyn®) Authorized Generic Concerta®) Methylphenidate ER Susp (Quillivant XR®) Methylphenidate IR (Ritalin®) Modafinil Tablet (Generic) Methylphenidate Solution (Generic; Authorized Generic; Methylin®) Methylphenidate -

Lodoxamide Attenuates Hepatic Fibrosis in Mice: Involvement of GPR35
Original Article Biomol Ther 28(1), 92-97 (2020) Lodoxamide Attenuates Hepatic Fibrosis in Mice: Involvement of GPR35 Mi-Jeong Kim, Soo-Jin Park, So-Yeon Nam and Dong-Soon Im* College of Pharmacy, Pusan National University, Busan 46241, Republic of Korea Abstract A previous pharmacogenomic analysis identified cromolyn, an anti-allergic drug, as an effective anti-fibrotic agent that acts on hepatocytes and stellate cells. Furthermore, cromolyn was shown to be a G protein-coupled receptor 35 (GPR35) agonist. How- ever, it has not been studied whether anti-fibrotic effects are mediated by GPR35. Therefore, in this study, the role of GPR35 in hepatic fibrosis was investigated through the use of lodoxamide, another anti-allergic drug and a potent GPR35 agonist. Long- term treatment with carbon tetrachloride induced hepatic fibrosis, which was inhibited by treatment with lodoxamide. Furthermore, CID2745687, a specific GPR35 antagonist, reversed lodoxamide-mediated anti-fibrotic effects. In addition, lodoxamide treatment showed significant effects on the mRNA expression of collagen Iα1, collagen Iα2, and TGF-β1 in the extracellular matrix. However, a transforming growth factor α (TGF-α) shedding assay revealed lodoxamide not to be a potent agonist of mouse GPR35 in vitro. Therefore, these results showed anti-fibrotic effects of lodoxamide in mice and raise concerns how lodoxamide protects against liver fibrosis in vivo and whether GPR35 is involved in the action. Key Words: Fibrosis, Liver, Lodoxamide, CID2745687, Carbon tetrachloride INTRODUCTION et al., 2010a, 2010b; Jenkins et al., 2010; Zhao et al., 2010; Jenkins et al., 2012; Funke et al., 2013; Neetoo-Isseljee et al., Liver fibrosis results from acute damage and the subse- 2013; Thimm et al., 2013; MacKenzie et al., 2014). -

BCBSM Clinical Drug List (Formulary)
Blue Cross Blue Shield of Michigan ® ® Clinical Drug List (Formulary) Please note that this listing of medications contained in this Blue Cross Blue Shield of Michigan Clinical Drug List (Formulary) is current at the time that the list is posted to this website, and is subject to change. INTRODUCTION Blue Cross Blue Shield of Michigan is pleased to provide the Clinical Drug List as a useful reference and educational tool to assist providers in selecting cost-effective therapies. Please familiarize yourself with this information. To provide effective high-quality care, this Clinical Drug List requires the continuing support of physicians and phar - macists. Your questions and suggestions are welcome. PREFACE The Blue Cross Blue Shield of Michigan Clinical Drug List is a list of FDA-approved prescription drug medications reviewed by the BCBSM/BCN Pharmacy and Therapeutics (P&T) Committee. The Clinical Drug List will assist in maintaining the quality of patient care and containing cost for the member’s drug benefit plan. Providers, physicians, and pharmacists are encouraged to refer to the Clinical Drug List when selecting prescription drug therapy for eligible plan members. Physicians are encouraged to prescribe med ications included in the Clinical Drug List whenever possible. If a prescrip tion is written for a nonpreferred drug or for a drug or dose not recommended for use in the elderly or pregnant, phar macists are encouraged to contact the physician. The benefit plan administrator will monitor provider- specific drug list prescribing and communicate with providers to optimize compliance. The Clinical Drug List is divided into major therapeutic categories (chapters) for easy use. -

FDA Listing of Established Pharmacologic Class Text Phrases January 2021
FDA Listing of Established Pharmacologic Class Text Phrases January 2021 FDA EPC Text Phrase PLR regulations require that the following statement is included in the Highlights Indications and Usage heading if a drug is a member of an EPC [see 21 CFR 201.57(a)(6)]: “(Drug) is a (FDA EPC Text Phrase) indicated for Active Moiety Name [indication(s)].” For each listed active moiety, the associated FDA EPC text phrase is included in this document. For more information about how FDA determines the EPC Text Phrase, see the 2009 "Determining EPC for Use in the Highlights" guidance and 2013 "Determining EPC for Use in the Highlights" MAPP 7400.13.