Aliskiren Achieved Better Control Than Irbesartan
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Valturna Label
HIGHLIGHTS OF PRESCRIBING INFORMATION -------------------------WARNINGS AND PRECAUTIONS---------------- These highlights do not include all the information needed to use • Avoid fetal or neonatal exposure. (5.1) Valturna safely and effectively. See full prescribing information for • Head and neck angioedema: Discontinue Valturna and monitor until Valturna. signs and symptoms resolve. (5.2) • Hypotension in volume- or salt-depleted Patients: Correct imbalances Valturna (aliskiren and valsartan, USP) Tablets before initiating therapy with Valturna. (5.3) Initial U.S. Approval: 2009 • Patients with renal impairment: Decreases in renal function may be anticipated in susceptible individuals. (5.4) WARNING: AVOID USE IN PREGNANCY • Patients with hepatic impairment: Slower clearance may occur. (5.5) See full prescribing information for complete boxed warning. • Hyperkalemia: Consider periodic determinations of serum electrolytes to When pregnancy is detected, discontinue Valturna as soon as possible. detect possible electrolyte imbalances, particularly in patients at risk. When used in pregnancy during the second and third trimester, drugs (5.7) that act directly on the renin-angiotensin system can cause injury and death to the developing fetus. (5.1) --------------------------------ADVERSE REACTIONS----------------------- The most common adverse events (incidence ≥1.5% and more common than ---------------------------INDICATIONS AND USAGE----------------------- with placebo) are: fatigue and nasopharyngitis. (6.1) Valturna is a combination of aliskiren, a direct renin inhibitor, and valsartan, an angiotensin II receptor blocker (ARB), indicated for the treatment of To report SUSPECTED ADVERSE REACTIONS, contact Novartis hypertension: Pharmaceuticals Corporation at 1-888-669-6682 or FDA at • In patients not adequately controlled with monotherapy. (1) 1-800-FDA-1088 or www.fda.gov/medwatch • May be substituted for titrated components. -

Patient Information Telmisartan (TEL-Mi-SAR-Tan) Tablets, USP
Patient Information Telmisartan (TEL-mi-SAR-tan) Tablets, USP Read this Patient Information before you start taking telmisartan tablets and each time you get a refill. There may be new information. This information does not take the place of talking to your doctor about your medical condition or your treatment. What is the most important information I should know about telmisartan tablets? Telmisartan tablets can cause harm or death to an unborn baby. Talk to your doctor about other ways to lower your blood pressure if you plan to become pregnant. If you get pregnant while taking telmisartan tablets, tell your doctor right away. What are telmisartan tablets? Telmisartan tablets are a prescription medicine used: • to treat high blood pressure (hypertension) It is not known if telmisartan tablets are safe and effective in children. Who should not take telmisartan tablets? You should not take telmisartan tablets if you are allergic (hypersensitive) to the active ingredient (telmisartan) or any of the other ingredients listed at the end of this leaflet. For patients with diabetes, if you are taking telmisartan tablets you should not take aliskiren. What should I tell my doctor before taking telmisartan tablets? Before you take telmisartan tablets, tell your doctor if you: • are pregnant or are planning to become pregnant. See “What is the most important information I should know about telmisartan tablets?” • are breast-feeding or plan to breast-feed. It is not known if telmisartan passes into your breast milk. You and your doctor should decide if you will take telmisartan tablets or breast-feed. You should not do both. -

Effect of Aldosterone Breakthrough on Albuminuria During Treatment with a Direct Renin Inhibitor and Combined Effect with a Mineralocorticoid Receptor Antagonist
Hypertension Research (2013) 36, 879–884 & 2013 The Japanese Society of Hypertension All rights reserved 0916-9636/13 www.nature.com/hr ORIGINAL ARTICLE Effect of aldosterone breakthrough on albuminuria during treatment with a direct renin inhibitor and combined effect with a mineralocorticoid receptor antagonist Atsuhisa Sato and Seiichi Fukuda We have reported observing aldosterone breakthrough in the course of relatively long-term treatment with renin–angiotensin (RA) system inhibitors, where the plasma aldosterone concentration (PAC) increased following an initial decrease. Aldosterone breakthrough has the potential to eliminate the organ-protective effects of RA system inhibitors. We therefore conducted a study in essential hypertensive patients to determine whether aldosterone breakthrough occurred during treatment with the direct renin inhibitor (DRI) aliskiren and to ascertain its clinical significance. The study included 40 essential hypertensive patients (18 men and 22 women) who had been treated for 12 months with aliskiren. Aliskiren significantly decreased blood pressure and plasma renin activity (PRA). The PAC was also decreased significantly at 3 and 6 months; however, the significant difference disappeared after 12 months. Aldosterone breakthrough was observed in 22 of the subjects (55%). Urinary albumin excretion differed depending on whether breakthrough occurred. For the subjects in whom aldosterone breakthrough was observed, eplerenone was added. A significant decrease in urinary albumin excretion was observed after 1 month, independent of changes in blood pressure. In conclusion, this study demonstrated that aldosterone breakthrough occurs in some patients undergoing DRI therapy. Aldosterone breakthrough affects the drug’s ability to improve urinary albumin excretion, and combining a mineralocorticoid receptor antagonist with the DRI may be useful for decreasing urinary albumin excretion. -

A Comparison of the Tolerability of the Direct Renin Inhibitor Aliskiren and Lisinopril in Patients with Severe Hypertension
Journal of Human Hypertension (2007) 21, 780–787 & 2007 Nature Publishing Group All rights reserved 0950-9240/07 $30.00 www.nature.com/jhh ORIGINAL ARTICLE A comparison of the tolerability of the direct renin inhibitor aliskiren and lisinopril in patients with severe hypertension RH Strasser1, JG Puig2, C Farsang3, M Croket4,JLi5 and H van Ingen4 1Technical University Dresden, Heart Center, University Hospital, Dresden, Germany; 2Department of Internal Medicine, La Paz Hospital, Madrid, Spain; 31st Department of Internal Medicine, Semmelweis University, Budapest, Hungary; 4Novartis Pharma AG, Basel, Switzerland and 5Novartis Institutes for Biomedical Research, Cambridge, MA, USA Patients with severe hypertension (4180/110 mm Hg) LIS 3.4%). The most frequently reported AEs in both require large blood pressure (BP) reductions to reach groups were headache, nasopharyngitis and dizziness. recommended treatment goals (o140/90 mm Hg) and At end point, ALI showed similar mean reductions from usually require combination therapy to do so. This baseline to LIS in msDBP (ALI À18.5 mm Hg vs LIS 8-week, multicenter, randomized, double-blind, parallel- À20.1 mm Hg; mean treatment difference 1.7 mm Hg group study compared the tolerability and antihyperten- (95% confidence interval (CI) À1.0, 4.4)) and mean sitting sive efficacy of the novel direct renin inhibitor aliskiren systolic blood pressure (ALI À20.0 mm Hg vs LIS with the angiotensin converting enzyme inhibitor À22.3 mm Hg; mean treatment difference 2.8 mm Hg lisinopril in patients with severe hypertension (mean (95% CI À1.7, 7.4)). Responder rates (msDBPo90 mm Hg sitting diastolic blood pressure (msDBP)X105 mm Hg and/or reduction from baselineX10 mm Hg) were 81.5% and o120 mm Hg). -

Summary of Product Characteristics
Proposed var 24 psusa cilazapril SUMMARY OF PRODUCT CHARACTERISTICS 1. NAME OF THE MEDICINAL PRODUCT [Fosinopril sodium 10 mg, tablets] [Fosinopril sodium 20 mg, tablets] 2. QUALITATIVE AND QUANTITATIVE COMPOSITION Each tablet contains 10 or 20 mg fosinopril sodium. Excipient with known effect: Each tablet fosinopril sodium 10 mg contains 87 mg of lactose, anhydrous. Each tablet fosinopril sodium 20 mg contains 174 mg of lactose, anhydrous. For the full list of excipients, see section 6.1. 3. PHARMACEUTICAL FORM Tablet. The 10 mg tablets are white and shaped like a capsule with indents. On one side they are engraved with the letters “APO” and on the other side with “FOS-10”. The 20 mg tablets are white and their shape is oval. On one side they are engraved with the letters “APO” and on the other side with “FOS-20”. 4. CLINICAL PARTICULARS 4.1 Therapeutic indications - Treatment of hypertension. - Treatment of symptomatic heart failure. 4.2 Posology and method of administration Posology Fosinopril sodium should be administered orally in a single daily dose. As with all other medicinal products taken once daily, it should be taken at approximately the same time each day. The absorption of fosinopril sodium is not affected by food. The dose should be individualised according to patient profile and blood pressure response (see section 4.4). Hypertension: Fosinopril sodium may be used as a monotherapy or in combination with other classes of antihypertensive medicinal products (see section 4.3, 4.4, 4.5 and 5.1). Hypertensive patients not being treated with diuretics: Starting dose The initial recommended dose is 10 mg once a day. -

COZAAR (Losartan Potassium) Tablets, for Oral Use
HIGHLIGHTS OF PRESCRIBING INFORMATION • Increase dose to 100 mg once daily if further blood pressure These highlights do not include all the information needed to use response is needed. (2.3) COZAAR safely and effectively. See full prescribing information for COZAAR. --------------------- DOSAGE FORMS AND STRENGTHS --------------------- Tablets: 25 mg; 50 mg; and 100 mg. (3) ® COZAAR (losartan potassium) tablets, for oral use ------------------------------- CONTRAINDICATIONS ------------------------------- Initial U.S. Approval: 1995 • Hypersensitivity to any component. (4) • Coadministration with aliskiren in patients with diabetes. (4) WARNING: FETAL TOXICITY See full prescribing information for complete boxed warning. ----------------------- WARNINGS AND PRECAUTIONS ----------------------- • Hypotension: Correct volume or salt depletion prior to administration When pregnancy is detected, discontinue COZAAR as soon as of COZAAR. (5.2) possible. Drugs that act directly on the renin-angiotensin system • Monitor renal function and potassium in susceptible patients. (5.3, can cause injury and death to the developing fetus. (5.1) 5.4) --------------------------- RECENT MAJOR CHANGES --------------------------- ------------------------------ ADVERSE REACTIONS ------------------------------ Warnings and Precautions Hyperkalemia (5.4) 10/2018 Most common adverse reactions (incidence ≥2% and greater than placebo) are: dizziness, upper respiratory infection, nasal congestion, ----------------------------INDICATIONS AND USAGE ---------------------------- and back pain. (6.1) COZAAR is an angiotensin II receptor blocker (ARB) indicated for: • Treatment of hypertension, to lower blood pressure in adults and To report SUSPECTED ADVERSE REACTIONS, contact Merck children greater than 6 years old. Lowering blood pressure reduces Sharp & Dohme Corp., a subsidiary of Merck & Co., Inc., at 1-877- the risk of fatal and nonfatal cardiovascular events, primarily strokes 888-4231 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch. -
![1 SUMMARY of PRODUCT CHARACTERISTICS 1. NAME of the MEDICINAL PRODUCT [Nationally Completed Name] 5 Mg Film-Coated Tablets [Nati](https://docslib.b-cdn.net/cover/8783/1-summary-of-product-characteristics-1-name-of-the-medicinal-product-nationally-completed-name-5-mg-film-coated-tablets-nati-2518783.webp)
1 SUMMARY of PRODUCT CHARACTERISTICS 1. NAME of the MEDICINAL PRODUCT [Nationally Completed Name] 5 Mg Film-Coated Tablets [Nati
SUMMARY OF PRODUCT CHARACTERISTICS 1. NAME OF THE MEDICINAL PRODUCT [nationally completed name] 5 mg film-coated tablets [nationally completed name] 10 mg film-coated tablets [nationally completed name] 20 mg film-coated tablets 2. QUALITATIVE AND QUANTITATIVE COMPOSITION One film-coated tablet contains 5/10/20 mg Benazepril hydrochloride. For the full list of excipients see section 6.1 3. PHARMACEUTICAL FORM Film-coated tablet [nationally completed name] 5 mg film-coated tablets: Oval (4 x 8 mm), light yellow film-coated tablets with score on both sides. [nationally completed name] 10 mg film-coated tablets: Oval (11 x 5.5 mm) yellow film-coated tablets with score on both sides. [nationally completed name] 20 mg film-coated tablets: Oval (11 x 5.5 mm) light red film-coated tablet with score on both sides. The tablet can be divided into equal doses. 4. CLINICAL PARTICULARS 4.1 Therapeutic indications Essential hypertension, congestive heart failure - in addition to diuretics and especially to digitalis glycosides in cases of severe congestive heart failure 4.2 Posology and method of administration Posology Paediatric population [nationally completed name] is not recommended for use in children due to insufficient data on safety and efficacy (see section 4.4). Essential hypertension 10 to 20 mg daily divided in one or two doses. Maximum daily dose is 40 mg. Congestive heart failure Initially 2.5 mg daily. After 2-4 weeks the dosage can be increased to 5 mg daily. Maximum dose is 20 mg daily. Dosage at renal impairment For the treatment of essential hypertension the dose should be reduced if creatinine clearance is below 30 ml/min. -
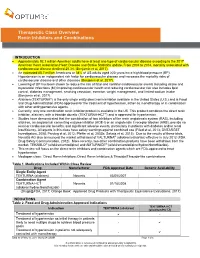
Therapeutic Class Overview Renin Inhibitors and Combinations
Therapeutic Class Overview Renin Inhibitors and Combinations INTRODUCTION Approximately 92.1 million American adults have at least one type of cardiovascular disease according to the 2017 American Heart Association Heart Disease and Stroke Statistics update. From 2004 to 2014, mortality associated with cardiovascular disease declined 25.3% (Benjamin et al, 2017). An estimated 85.7 million Americans or 34% of US adults aged ≥20 years have high blood pressure (BP). Hypertension is an independent risk factor for cardiovascular disease and increases the mortality risks of cardiovascular disease and other diseases (Benjamin et al, 2017). Lowering of BP has been shown to reduce the risk of fatal and nonfatal cardiovascular events including stroke and myocardial infarctions (MI) improving cardiovascular health and reducing cardiovascular risk also includes lipid control, diabetes management, smoking cessation, exercise, weight management, and limited sodium intake (Benjamin et al, 2017). Aliskiren (TEKTURNA®) is the only single entity direct renin inhibitor available in the United States (U.S.) and is Food and Drug Administration (FDA)-approved for the treatment of hypertension, either as monotherapy or in combination with other antihypertensive agents. Currently, only one combination renin inhibitor product is available in the US. This product combines the direct renin inhibitor, aliskiren, with a thiazide diuretic (TEKTURNA-HCT®) and is approved for hypertension. Studies have demonstrated that the combination of two inhibitors of the renin angiotensin system (RAS), including aliskiren, an angiotensin converting enzyme inhibitor (ACE-I) or an angiotensin II receptor blocker (ARB), provide no renal or cardiovascular benefits, and significant adverse events, particularly in patients with diabetes and/or renal insufficiency. -

Aliskiren – an Alternative to Angiotensin-Converting Enzyme Inhibitors Or Angiotensin Receptor Blockers in the Therapy of Arterial Hypertension
State of the art paper Aliskiren – an alternative to angiotensin-converting enzyme inhibitors or angiotensin receptor blockers in the therapy of arterial hypertension Iwona Zaporowska-Stachowiak 1, Karolina Hoffmann 2, Wiesław Bryl 2, Andrzej Minczykowski 3 1Chair and Department of Pharmacology, Poznan University of Medical Sciences, Corresponding author: Poland Iwona Zaporowska- 2Chair and Department of Internal Medicine, Metabolic Disorders and Arterial Stachowiak MD, PhD Hypertension, Poznan University of Medical Sciences, Poland Chair and Department 3Department of Cardiology-Intensive Therapy, Poznan University of Medical Sciences, of Pharmacology Poland Poznan University of Medical Sciences Submitted: 18 September 2012 5A Rokietnicka St Accepted: 20 December 2012 60-806 Poznan, Poland Phone: +48 61 854 72 62 Arch Med Sci 2014; 10, 4: 830–836 Fax: +48 61 854 72 52 DOI: 10.5114/aoms.2013.34723 E-mail: [email protected] Copyright © 2014 Termedia & Banach Abstract There has been enormous progress in antihypertensive therapy over the last few decades. However, the management of arterial hypertension is still insuf - ficient and more efforts are needed to improve both non-pharmacological and pharmacological treatment of this widely prevalent disease. Renin-angiotensin- aldosterone system (RAAS) inhibition is crucial both for blood pressure (BP) con - trol and for prevention of organ damage or its development in patients with hypertension. Angiotensin-converting enzyme inhibitors and/or sartans block RAAS incompletely. Aliskiren is one of the novel drugs that has been introduced to antihypertensive therapy recently. Up to now no trial has confirmed that aliskiren is efficacious in reducing cardiovascular events. Double RAAS blockade with aliskiren was not always safe. -

Angiotensin Modulators: ACE Inhibitors and Direct Renin Inhibitors Review 10/09/2008
Angiotensin Modulators: ACE Inhibitors and Direct Renin Inhibitors Review 10/09/2008 Copyright © 2004 - 2008 by Provider Synergies, L.L.C. All rights reserved. Printed in the United States of America. All rights reserved. No part of this publication may be reproduced or transmitted in any form or by any means, electronic or mechanical, including photocopying, recording, digital scanning, or via any information storage and retrieval system without the express written consent of Provider Synergies, L.L.C. All requests for permission should be mailed to: Attention: Copyright Administrator Intellectual Property Department Provider Synergies, L.L.C. 5181 Natorp Blvd., Suite 205 Mason, Ohio 45040 The materials contained herein represent the opinions of the collective authors and editors and should not be construed to be the official representation of any professional organization or group, any state Pharmacy and Therapeutics committee, any state Medicaid Agency, or any other clinical committee. This material is not intended to be relied upon as medical advice for specific medical cases and nothing contained herein should be relied upon by any patient, medical professional or layperson seeking information about a specific course of treatment for a specific medical condition. All readers of this material are responsible for independently obtaining medical advice and guidance from their own physician and/or other medical professional in regard to the best course of treatment for their specific medical condition. This publication, inclusive of all forms contained herein, is intended to be educational in nature and is intended to be used for informational purposes only. Comments and suggestions may be sent to [email protected]. -

TEKTURNA (Aliskiren) Oral Pellets Tekturna Is Contraindicated in Pediatric Patients Less Than 2 Years of Age
HIGHLIGHTS OF PRESCRIBING INFORMATION --------------------------------CONTRAINDICATIONS---------------------------- These highlights do not include all the information needed to use Do not use with angiotensin receptor blockers (ARBs) or angiotensin TEKTURNA safely and effectively. See full prescribing information for converting enzyme inhibitors (ACEIs) in patients with diabetes. (4) TEKTURNA. TEKTURNA® (aliskiren) tablets, for oral use Hypersensitivity to any of the components. (4) TEKTURNA (aliskiren) oral pellets Tekturna is contraindicated in pediatric patients less than 2 years of age. (4) Initial U.S. Approval: 2007 -----------------------WARNINGS AND PRECAUTIONS---------------------- WARNING: FETAL TOXICITY See full prescribing information for complete boxed warning. Avoid concomitant use with ARBs or ACEIs particularly in patients with renal impairment [creatinine clearance (CrCl) <60 mL/min]. (5.2, When pregnancy is detected, discontinue Tekturna as soon as 5.4) possible. (5.1, 8.1) Anaphylactic Reactions and Head and Neck Angioedema. (5.3) Drugs that act directly on the renin-angiotensin system can cause Hypotension: Correct imbalances in volume and/or salt depleted injury and death to the developing fetus. (5.1, 8.1) patients. (5.4) Impaired Renal Function: Monitor serum creatinine periodically. (5.5) ---------------------------RECENT MAJOR CHANGES-------------------------- Hyperkalemia: Monitor potassium levels periodically. (5.6) Dosage and Administration (2.2, 2.3) 11/2017 ------------------------------ADVERSE -

Tekturna (Aliskiren) Tablets Label
HIGHLIGHTS OF PRESCRIBING INFORMATION -----------DOSAGE FORMS AND STRENGTHS------------ Tablets: 150 mg, 300 mg (3) These highlights do not include all the information needed to use ® TEKTURNA safely and effectively. See full prescribing information for --------------------CONTRAINDICATIONS--------------------- TEKTURNA®. Do not use with angiotensin receptor blockers (ARBs) or ACE inhibitors Tekturna® (aliskiren) tablets, for oral use (ACEIs) in patients with diabetes (4) Initial U.S. Approval: 2007 ---------------WARNINGS AND PRECAUTIONS------------ WARNING: FETAL TOXICITY Avoid concomitant use with ARBs or ACEIs in patients with renal impairment (GFR<60 mL/min) (5.2) See full prescribing information for complete boxed warning Anaphylactic Reactions and Head and Neck Angioedema: Discontinue use of Tekturna and monitor until signs and symptoms When pregnancy is detected, discontinue Tekturna as soon as resolve (5.3) possible. (5.1) Hypotension in volume and/or salt depleted patients: Correct Drugs that act directly on the renin-angiotensin system can cause imbalances before initiating therapy with Tekturna (5.4) injury and death to the developing fetus. (5.1) Impaired renal function: Monitor serum creatinine periodically. (5.5) --------------RECENT MAJOR CHANGES--------------------- Hyperkalemia: Monitor potassium levels periodically. (5.6) Boxed Warning: Fetal Toxicity 02/2012 Contraindications: Concomitant use with ARBs or ACEIs in -------------------ADVERSE REACTIONS---------------------- diabetes (4) 03/2012 Most common adverse reaction: diarrhea (incidence 2.3%) (6.1) Warnings and Precautions (5.1) 02/2012 To report SUSPECTED ADVERSE REACTIONS, contact Novartis Warnings and Precautions (5.2, 5.4, 5.5, 5.6) 03/2012 Pharmaceuticals Corporation at 1-888-669-6682 or FDA at 1-800 Warnings and Precautions (5.3) 09/2012 FDA-1088 or www.fda.gov/medwatch.