Pharmacologyonline 2: 497-517 (2010) Ewsletter Bernardi Et
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Pharmacy Reengineering (PRE) V.0.5 Pre-Release Implementation
PHARMACY REENGINEERING (PRE) Version 0.5 Pre-Release Implementation Guide PSS*1*129 & PSS*1*147 February 2010 Department of Veterans Affairs Office of Enterprise Development Revision History Date Revised Patch Description Pages Number 02/2010 All PSS*1*147 Added Revision History page. Updated patch references to include PSS*1*147. Described files, fields, options and routines added/modified as part of this patch. Added Chapter 5, Additive Frequency for IV Additives, to describe the steps needed to ensure correct data is in the new IV Additive REDACTED 01/2009 All PSS*1*129 Original version REDACTED February 2010 Pharmacy Reengineering (PRE) V. 0.5 Pre-Release i Implementation Guide PSS*1*129 & PSS*1*147 Revision History (This page included for two-sided copying.) ii Pharmacy Reengineering (PRE) V. 0.5 Pre-Release February 2010 Implementation Guide PSS*1*129 & PSS*1*147 Table of Contents Introduction ................................................................................................................................. 1 Purpose ....................................................................................................................................1 Project Description ....................................................................................................................1 Scope ........................................................................................................................................3 Menu Changes ..........................................................................................................................4 -

)&F1y3x PHARMACEUTICAL APPENDIX to THE
)&f1y3X PHARMACEUTICAL APPENDIX TO THE HARMONIZED TARIFF SCHEDULE )&f1y3X PHARMACEUTICAL APPENDIX TO THE TARIFF SCHEDULE 3 Table 1. This table enumerates products described by International Non-proprietary Names (INN) which shall be entered free of duty under general note 13 to the tariff schedule. The Chemical Abstracts Service (CAS) registry numbers also set forth in this table are included to assist in the identification of the products concerned. For purposes of the tariff schedule, any references to a product enumerated in this table includes such product by whatever name known. Product CAS No. Product CAS No. ABAMECTIN 65195-55-3 ACTODIGIN 36983-69-4 ABANOQUIL 90402-40-7 ADAFENOXATE 82168-26-1 ABCIXIMAB 143653-53-6 ADAMEXINE 54785-02-3 ABECARNIL 111841-85-1 ADAPALENE 106685-40-9 ABITESARTAN 137882-98-5 ADAPROLOL 101479-70-3 ABLUKAST 96566-25-5 ADATANSERIN 127266-56-2 ABUNIDAZOLE 91017-58-2 ADEFOVIR 106941-25-7 ACADESINE 2627-69-2 ADELMIDROL 1675-66-7 ACAMPROSATE 77337-76-9 ADEMETIONINE 17176-17-9 ACAPRAZINE 55485-20-6 ADENOSINE PHOSPHATE 61-19-8 ACARBOSE 56180-94-0 ADIBENDAN 100510-33-6 ACEBROCHOL 514-50-1 ADICILLIN 525-94-0 ACEBURIC ACID 26976-72-7 ADIMOLOL 78459-19-5 ACEBUTOLOL 37517-30-9 ADINAZOLAM 37115-32-5 ACECAINIDE 32795-44-1 ADIPHENINE 64-95-9 ACECARBROMAL 77-66-7 ADIPIODONE 606-17-7 ACECLIDINE 827-61-2 ADITEREN 56066-19-4 ACECLOFENAC 89796-99-6 ADITOPRIM 56066-63-8 ACEDAPSONE 77-46-3 ADOSOPINE 88124-26-9 ACEDIASULFONE SODIUM 127-60-6 ADOZELESIN 110314-48-2 ACEDOBEN 556-08-1 ADRAFINIL 63547-13-7 ACEFLURANOL 80595-73-9 ADRENALONE -

Pharmacologyonline 2: 727-753 (2010) Ewsletter Bradu and Rossini
Pharmacologyonline 2: 727-753 (2010) ewsletter Bradu and Rossini COTRAST AGETS - IODIATED PRODUCTS. SECOD WHO-ITA / ITA-OMS 2010 COTRIBUTIO O AGGREGATE WHO SYSTEM-ORGA CLASS DISORDERS AD/OR CLUSTERIG BASED O REPORTED ADVERSE REACTIOS/EVETS Dan Bradu and Luigi Rossini* Servizio Nazionale Collaborativo WHO-ITA / ITA-OMS, Università Politecnica delle Marche e Progetto di Farmacotossicovigilanza, Azienda Ospedaliera Universitaria Ospedali Riuniti di Ancona, Regione Marche, Italia Summary From the 2010 total basic adverse reactions and events collected as ADRs preferred names in the WHO-Uppsala Drug Monitoring Programme, subdivided in its first two twenty years periods as for the first seven iodinated products diagnostic contrast agents amidotrizoate, iodamide, iotalamate, iodoxamate, ioxaglate, iohexsol and iopamidol, their 30 WHO-system organ class disorders (SOCDs) aggregates had been compared. Their common maximum 97% levels identified six SOCDs only, apt to evaluate the most frequent single ADRs for each class, and their percentual normalization profiles for each product. The WILKS's chi square statistics for the related contingency tables, and Gabriel’s STP procedure applied to the extracted double data sets then produced profile binary clustering, as well as Euclidean confirmatory plots. They finally showed similar objectively evaluated autoclassificative trends of these products, which do not completely correspond to their actual ATC V08A A, B and C subdivision: while amidotrizoate and iotalamate, and respectively iohesol and iopamidol are confirmed to belong to the A and B subgroups, ioxaglate behaves fluctuating within A, B and C, but iodamide looks surprizingly, constantly positioned together with iodoxamate as binary/ternary C associated. In view of the recent work of Campillos et al (Science, 2008) which throws light on the subject, the above discrepancies do not appear anymore unexpected or alarming. -

Title 16. Crimes and Offenses Chapter 13. Controlled Substances Article 1
TITLE 16. CRIMES AND OFFENSES CHAPTER 13. CONTROLLED SUBSTANCES ARTICLE 1. GENERAL PROVISIONS § 16-13-1. Drug related objects (a) As used in this Code section, the term: (1) "Controlled substance" shall have the same meaning as defined in Article 2 of this chapter, relating to controlled substances. For the purposes of this Code section, the term "controlled substance" shall include marijuana as defined by paragraph (16) of Code Section 16-13-21. (2) "Dangerous drug" shall have the same meaning as defined in Article 3 of this chapter, relating to dangerous drugs. (3) "Drug related object" means any machine, instrument, tool, equipment, contrivance, or device which an average person would reasonably conclude is intended to be used for one or more of the following purposes: (A) To introduce into the human body any dangerous drug or controlled substance under circumstances in violation of the laws of this state; (B) To enhance the effect on the human body of any dangerous drug or controlled substance under circumstances in violation of the laws of this state; (C) To conceal any quantity of any dangerous drug or controlled substance under circumstances in violation of the laws of this state; or (D) To test the strength, effectiveness, or purity of any dangerous drug or controlled substance under circumstances in violation of the laws of this state. (4) "Knowingly" means having general knowledge that a machine, instrument, tool, item of equipment, contrivance, or device is a drug related object or having reasonable grounds to believe that any such object is or may, to an average person, appear to be a drug related object. -

Page 1 Note: Within Nine Months from the Publication of the Mention
Europäisches Patentamt (19) European Patent Office & Office européen des brevets (11) EP 1 411 992 B1 (12) EUROPEAN PATENT SPECIFICATION (45) Date of publication and mention (51) Int Cl.: of the grant of the patent: A61K 49/04 (2006.01) A61K 49/18 (2006.01) 13.12.2006 Bulletin 2006/50 (86) International application number: (21) Application number: 02758379.8 PCT/EP2002/008183 (22) Date of filing: 23.07.2002 (87) International publication number: WO 2003/013616 (20.02.2003 Gazette 2003/08) (54) IONIC AND NON-IONIC RADIOGRAPHIC CONTRAST AGENTS FOR USE IN COMBINED X-RAY AND NUCLEAR MAGNETIC RESONANCE DIAGNOSTICS IONISCHES UND NICHT-IONISCHES RADIOGRAPHISCHES KONTRASTMITTEL ZUR VERWENDUNG IN DER KOMBINIERTEN ROENTGEN- UND KERNSPINTOMOGRAPHIEDIAGNOSTIK SUBSTANCES IONIQUES ET NON-IONIQUES DE CONTRASTE RADIOGRAPHIQUE UTILISEES POUR ETABLIR DES DIAGNOSTICS FAISANT APPEL AUX RAYONS X ET A L’IMAGERIE PAR RESONANCE MAGNETIQUE (84) Designated Contracting States: (74) Representative: Minoja, Fabrizio AT BE BG CH CY CZ DE DK EE ES FI FR GB GR Bianchetti Bracco Minoja S.r.l. IE IT LI LU MC NL PT SE SK TR Via Plinio, 63 20129 Milano (IT) (30) Priority: 03.08.2001 IT MI20011706 (56) References cited: (43) Date of publication of application: EP-A- 0 759 785 WO-A-00/75141 28.04.2004 Bulletin 2004/18 US-A- 5 648 536 (73) Proprietor: BRACCO IMAGING S.p.A. • K HERGAN, W. DORINGER, M. LÄNGLE W.OSER: 20134 Milano (IT) "Effects of iodinated contrast agents in MR imaging" EUROPEAN JOURNAL OF (72) Inventors: RADIOLOGY, vol. 21, 1995, pages 11-17, • AIME, Silvio XP002227102 20134 Milano (IT) • K.M. -

Studies on Experimental Iodine Allergy: 1. Antigen Recognition of Guinea Pig Anti-Iodine Antibody
The Journal of Toxicological Sciences, 131 Vol.29, No.2, 131-136, 2004 STUDIES ON EXPERIMENTAL IODINE ALLERGY: 1. ANTIGEN RECOGNITION OF GUINEA PIG ANTI-IODINE ANTIBODY Hiroshi SHIONOYA1 Yoshiki SUGIHARA2, Kazuo OKANO3, Fumio SAGAMI1, Takashi MIKAMI1 and Kouichi KATAYAMA3 1Department of Drug Safety Research, Eisai Kawashima Research Laboratories, Eisai Co., Ltd., 1 Takehaya-cho, Kawashima-cho, Hashima-gun, Gifu 501-0061, Japan 2Department of Drug Safety Research, Eisai Tsukuba Research Laboratories, Eisai Co., Ltd., 5-1-3 Tohkodai, Tsukuba-shi, Ibaraki 300-2635, Japan 3Exploratory Division, Eisai Tsukuba Research Laboratories, Eisai Co., Ltd., 5-1-3 Tohkodai, Tsukuba-shi, Ibaraki 300-2635, Japan (Received September 3, 2003; Accepted February 18, 2004) ABSTRACT — It has generally been thought that iodine allergy is cross-sensitive to various iodine-con- taining chemicals. However, this concept seems to deviate from the immunological principle that immune recognition is specific. To solve this contradiction, we hypothesize that iodine allergy is an immunological reaction to iodi- nated autologous proteins produced in vivo by iodination reaction from various iodine-containing chemi- cals. Antisera to iodine were obtained from guinea pigs immunized subcutaneously with iodine-potassium iodide solution emulsified in complete Freund’s adjuvant (CFA). The specificity of guinea pig anti-iodine antiserum was determined by enzyme-linked immunosorbent assay (ELISA) inhibition experiments using microplates coated with iodinated guinea pig serum albumin (I-GSA). Antibody activities were inhibited by I-GSA, diiodo-L-tyrosine, and thyroxine, but not by potassium iodide, monoiodo-L-tyrosine, 3,5,3’-tri- iodothyronine, monoiodo-L-histidine, or diiodo-L-histidine, or by ionic or non-ionic iodinated contrast media. -
![Ehealth DSI [Ehdsi V2.2.2-OR] Ehealth DSI – Master Value Set](https://docslib.b-cdn.net/cover/8870/ehealth-dsi-ehdsi-v2-2-2-or-ehealth-dsi-master-value-set-1028870.webp)
Ehealth DSI [Ehdsi V2.2.2-OR] Ehealth DSI – Master Value Set
MTC eHealth DSI [eHDSI v2.2.2-OR] eHealth DSI – Master Value Set Catalogue Responsible : eHDSI Solution Provider PublishDate : Wed Nov 08 16:16:10 CET 2017 © eHealth DSI eHDSI Solution Provider v2.2.2-OR Wed Nov 08 16:16:10 CET 2017 Page 1 of 490 MTC Table of Contents epSOSActiveIngredient 4 epSOSAdministrativeGender 148 epSOSAdverseEventType 149 epSOSAllergenNoDrugs 150 epSOSBloodGroup 155 epSOSBloodPressure 156 epSOSCodeNoMedication 157 epSOSCodeProb 158 epSOSConfidentiality 159 epSOSCountry 160 epSOSDisplayLabel 167 epSOSDocumentCode 170 epSOSDoseForm 171 epSOSHealthcareProfessionalRoles 184 epSOSIllnessesandDisorders 186 epSOSLanguage 448 epSOSMedicalDevices 458 epSOSNullFavor 461 epSOSPackage 462 © eHealth DSI eHDSI Solution Provider v2.2.2-OR Wed Nov 08 16:16:10 CET 2017 Page 2 of 490 MTC epSOSPersonalRelationship 464 epSOSPregnancyInformation 466 epSOSProcedures 467 epSOSReactionAllergy 470 epSOSResolutionOutcome 472 epSOSRoleClass 473 epSOSRouteofAdministration 474 epSOSSections 477 epSOSSeverity 478 epSOSSocialHistory 479 epSOSStatusCode 480 epSOSSubstitutionCode 481 epSOSTelecomAddress 482 epSOSTimingEvent 483 epSOSUnits 484 epSOSUnknownInformation 487 epSOSVaccine 488 © eHealth DSI eHDSI Solution Provider v2.2.2-OR Wed Nov 08 16:16:10 CET 2017 Page 3 of 490 MTC epSOSActiveIngredient epSOSActiveIngredient Value Set ID 1.3.6.1.4.1.12559.11.10.1.3.1.42.24 TRANSLATIONS Code System ID Code System Version Concept Code Description (FSN) 2.16.840.1.113883.6.73 2017-01 A ALIMENTARY TRACT AND METABOLISM 2.16.840.1.113883.6.73 2017-01 -
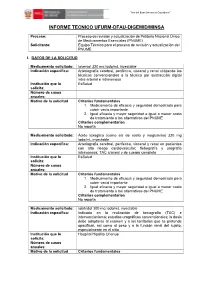
Informe Tecnico Ufurm-Dfau-Digemid/Minsa
“Año del Buen Servicio al Ciudadano” ” INFORME TECNICO UFURM-DFAU-DIGEMID/MINSA Proceso: Proceso de revisión y actualización de Petitorio Nacional Único de Medicamentos Esenciales (PNUME) Solicitante: Equipo Técnico para el proceso de revisión y actualización del PNUME I. DATOS DE LA SOLICITUD Medicamento solicitado: Ioversol 320 mg Iodo/mL inyectable Indicación específica: Arteriografía cerebral, periférica, visceral y renal utilizando las técnicas convencionales o la técnica por sustracción digital intra-arterial e intravenosa Institución que lo EsSalud solicita: Número de casos anuales: Motivo de la solicitud Criterios fundamentales 1. Medicamento de eficacia y seguridad demostrada para cubrir vacío importante. 2. Igual eficacia y mayor seguridad e igual o menor costo de tratamiento a las alternativas del PNUME Criterios complementarios No reporta Medicamento solicitado: Ácido ioxaglico (como sal de sodio y meglumina) 320 mg Iodo/mL inyectable Indicación específica: Arteriografia cerebral, periferica, visceral y renal en pacientes con alto riesgo cardiovascular; flebografía y urografía intravenosa; TAC craneal y de cuerpo completo Institución que lo EsSalud solicita: Número de casos anuales: Motivo de la solicitud Criterios fundamentales 1. Medicamento de eficacia y seguridad demostrada para cubrir vació importante. 2. Igual eficacia y mayor seguridad e igual o menor costo de tratamiento a las alternativas del PNUME Criterios complementarios No reporta Medicamento solicitado: Iobitridol 300 mg Iodo/mL inyectable Indicación específica: Indicado en la realización de tomografía (TAC) e intervencionismo; estudios urográficos convencionales; la dosis debe adaptarse al examen y a los territorios que se pretende opacificar, asi como al peso y a la función renal del sujeto, especialmente en el niño Institución que lo Hospital Hipólito Unanue solicita: Número de casos anuales: Motivo de la solicitud Criterios fundamentales “Año del Buen Servicio al Ciudadano” ” 1. -

Alphabetical Listing of ATC Drugs & Codes
Alphabetical Listing of ATC drugs & codes. Introduction This file is an alphabetical listing of ATC codes as supplied to us in November 1999. It is supplied free as a service to those who care about good medicine use by mSupply support. To get an overview of the ATC system, use the “ATC categories.pdf” document also alvailable from www.msupply.org.nz Thanks to the WHO collaborating centre for Drug Statistics & Methodology, Norway, for supplying the raw data. I have intentionally supplied these files as PDFs so that they are not quite so easily manipulated and redistributed. I am told there is no copyright on the files, but it still seems polite to ask before using other people’s work, so please contact <[email protected]> for permission before asking us for text files. mSupply support also distributes mSupply software for inventory control, which has an inbuilt system for reporting on medicine usage using the ATC system You can download a full working version from www.msupply.org.nz Craig Drown, mSupply Support <[email protected]> April 2000 A (2-benzhydryloxyethyl)diethyl-methylammonium iodide A03AB16 0.3 g O 2-(4-chlorphenoxy)-ethanol D01AE06 4-dimethylaminophenol V03AB27 Abciximab B01AC13 25 mg P Absorbable gelatin sponge B02BC01 Acadesine C01EB13 Acamprosate V03AA03 2 g O Acarbose A10BF01 0.3 g O Acebutolol C07AB04 0.4 g O,P Acebutolol and thiazides C07BB04 Aceclidine S01EB08 Aceclidine, combinations S01EB58 Aceclofenac M01AB16 0.2 g O Acefylline piperazine R03DA09 Acemetacin M01AB11 Acenocoumarol B01AA07 5 mg O Acepromazine N05AA04 -
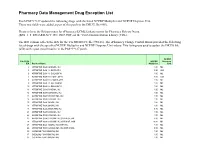
Pharmacy Data Management Drug Exception List
Pharmacy Data Management Drug Exception List Patch PSS*1*127 updated the following drugs with the listed NCPDP Multiplier and NCPDP Dispense Unit. These two fields were added as part of this patch to the DRUG file (#50). Please refer to the Release notes for ePharmacy/ECME Enhancements for Pharmacy Release Notes (BPS_1_5_EPHARMACY_RN_0907.PDF) on the VistA Documentation Library (VDL). The IEN column reflects the IEN for the VA PRODUCT file (#50.68). The ePharmacy Change Control Board provided the following list of drugs with the specified NCPDP Multiplier and NCPDP Dispense Unit values. This listing was used to update the DRUG file (#50) with a post install routine in the PSS*1*127 patch. NCPDP File 50.68 NCPDP Dispense IEN Product Name Multiplier Unit 2 ATROPINE SO4 0.4MG/ML INJ 1.00 ML 3 ATROPINE SO4 1% OINT,OPH 3.50 GM 6 ATROPINE SO4 1% SOLN,OPH 1.00 ML 7 ATROPINE SO4 0.5% OINT,OPH 3.50 GM 8 ATROPINE SO4 0.5% SOLN,OPH 1.00 ML 9 ATROPINE SO4 3% SOLN,OPH 1.00 ML 10 ATROPINE SO4 2% SOLN,OPH 1.00 ML 11 ATROPINE SO4 0.1MG/ML INJ 1.00 ML 12 ATROPINE SO4 0.05MG/ML INJ 1.00 ML 13 ATROPINE SO4 0.4MG/0.5ML INJ 1.00 ML 14 ATROPINE SO4 0.5MG/ML INJ 1.00 ML 15 ATROPINE SO4 1MG/ML INJ 1.00 ML 16 ATROPINE SO4 2MG/ML INJ 1.00 ML 18 ATROPINE SO4 2MG/0.7ML INJ 0.70 ML 21 ATROPINE SO4 0.3MG/ML INJ 1.00 ML 22 ATROPINE SO4 0.8MG/ML INJ 1.00 ML 23 ATROPINE SO4 0.1MG/ML INJ,SYRINGE,5ML 5.00 ML 24 ATROPINE SO4 0.1MG/ML INJ,SYRINGE,10ML 10.00 ML 25 ATROPINE SO4 1MG/ML INJ,AMP,1ML 1.00 ML 26 ATROPINE SO4 0.2MG/0.5ML INJ,AMP,0.5ML 0.50 ML 30 CODEINE PO4 30MG/ML -

Stembook 2018.Pdf
The use of stems in the selection of International Nonproprietary Names (INN) for pharmaceutical substances FORMER DOCUMENT NUMBER: WHO/PHARM S/NOM 15 WHO/EMP/RHT/TSN/2018.1 © World Health Organization 2018 Some rights reserved. This work is available under the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 IGO licence (CC BY-NC-SA 3.0 IGO; https://creativecommons.org/licenses/by-nc-sa/3.0/igo). Under the terms of this licence, you may copy, redistribute and adapt the work for non-commercial purposes, provided the work is appropriately cited, as indicated below. In any use of this work, there should be no suggestion that WHO endorses any specific organization, products or services. The use of the WHO logo is not permitted. If you adapt the work, then you must license your work under the same or equivalent Creative Commons licence. If you create a translation of this work, you should add the following disclaimer along with the suggested citation: “This translation was not created by the World Health Organization (WHO). WHO is not responsible for the content or accuracy of this translation. The original English edition shall be the binding and authentic edition”. Any mediation relating to disputes arising under the licence shall be conducted in accordance with the mediation rules of the World Intellectual Property Organization. Suggested citation. The use of stems in the selection of International Nonproprietary Names (INN) for pharmaceutical substances. Geneva: World Health Organization; 2018 (WHO/EMP/RHT/TSN/2018.1). Licence: CC BY-NC-SA 3.0 IGO. Cataloguing-in-Publication (CIP) data. -

Gadoxetic Acid (Rinn) Preparations Acide Gadoxétique; Ácido Gadoxético; Acidum Gadoxeticum; Pharmacopoeias
Gadoteric Acid/Iodamide 1481 Preparations cholangiopancreatography, and hysterosalpingography. It is also used for contrast enhancement in computed tomography. USP 31: Gadoversetamide Injection. HO It is usually available as solutions containing 54.84 to 76.78% of Proprietary Preparations (details are given in Part 3) iobitridol (equivalent to 250 to 350 mg/mL of iodine). The dose Arg.: Optimark; Austral.: Optimark; Canad.: Optimark; Cz.: Optimark; O and strength used varies depending on the procedure and route. Port.: Optimark; USA: Optimark. OH ◊ References. HO OH 1. Petersein J, et al. Results of the safety and efficacy of iobitridol in more than 61,000 patients. Eur Radiol 2003; 13: 2006–11. HO Gadoxetic Acid (rINN) Preparations Acide Gadoxétique; Ácido gadoxético; Acidum Gadoxeticum; Pharmacopoeias. In Eur. (see p.vii). Also in USNF. Proprietary Preparations (details are given in Part 3) Gd-EOB-DTPA. Dihydrogen [N-{(2S)-2-[bis(carboxymethyl)- Arg.: Xenetic; Xenetix; Austria: Xenetix; Belg.: Xenetix; Braz.: Henetix†; Ph. Eur. 6.2 (Galactose). A white or almost white, crystalline or Chile: Xenetix; Cz.: Xenetix; Denm.: Xenetix; Fin.: Xenetix; Fr.: Xenetix; amino]-3-(p-ethoxyphenyl)propyl}-N-{2-[bis(carboxymethyl)- finely granulated powder. Freely soluble or soluble in water; very Ger.: Xenetix; Gr.: Xenetix; Hung.: Xenetix; Israel: Xenetix; Ital.: amino]ethyl}glycinato(5−)]gadolinate(2−). slightly soluble in alcohol. Xenetix; Neth.: Xenetix; Norw.: Xenetix; Port.: Xenetix; Spain: Xenetix; Swed.: Xenetix; Switz.: Xenetix; Venez.: Xenetix. Гадоксетовая Кислота USNF 26 (Galactose). A white, crystalline or finely granulated powder. Soluble in water; very slightly soluble in alcohol. Store C23H30GdN3O11 = 681.7. in airtight containers. CAS — 135326-11-3 (gadoxetic acid).