Plasma Steroid Profiling and Response to Trophins to Illustrate Intra
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Tayside, Angus and Perthshire Fibromyalgia Support Group Scotland
Tayside, Angus and Perthshire Angus Long Term Conditions Support Fibromyalgia Support Group Scotland Groups Offer help and support to people suffering from fibromyalgia. This help and support also extends to Have 4 groups of friendly people who meet monthly at family and friends of sufferers and people who various locations within Angus and offer support to people would like more information on fibromyalgia. who suffer from any form of Long Term Condition or for ANGUS Directory They meet every first Saturday of every month at carers of someone with a Long Term Condition as well as Ninewells Hospital, Dundee. These meetings are each other, light refreshments are provided. to Local held on Level 7, Promenade Area starting at 11am For more information visit www.altcsg.org.uk or e-mail: Self Help Groups and finish at 1pm. [email protected] For more information contact TAP FM Support Group, PO Box 10183, Dundee DD4 8WT, visit www.tapfm.co.uk or e-mail - [email protected] . Multiple Sclerosis Society Angus Branch For information about, or assistance about the Angus Gatepost Branch please call 0845 900 57 60 between 9am - 8pm or e-mail Brian Robson at mailto:[email protected] GATEPOST is run by Scottish farming charity RSABI and offers a helpline service to anyone who works on the land in Scotland, and also their families. Myalgic Encephalomyelitis/Chronic They offer a friendly, listening ear and a sounding post for Fatigue Syndrome (ME/CFS) you at difficult times, whatever the reason. If you’re The aims of the support group are to give support to worried, stressed, or feeling isolated, they can help. -

Tayside Pain Service South Block, Level 6 NHS Tayside Ninewells Hospital Dundee DD1 9SY
Tayside Pain Service South Block, Level 6 NHS Tayside Ninewells Hospital Dundee DD1 9SY 01382 425612 www.nhstayside.scot.nhs.uk As a result of the Covid-19 coronavirus pandemic all non-urgent work within the NHS has stopped. All the medical, nursing and administrative staff working in our pain clinics are now required to support colleagues in the front line to provide life-saving treatments. At this point in time, we are unsure when normal services will be resumed but we will be guided by the Scottish Government. In the meantime, please continue to stay active whilst ensuring that you are following the guidance on preventing the spread of Covid-19. The following information may be helpful to let you manage your pain better: Pain Association Scotland will be setting up an on-line service that will have video link connection so that they can continue to deliver education and support. Further info available on support currently available will be on their website: https://painassociation.co.uk/ The following websites and videos may also be of use: www.chronicpaininfo.org www.painconcern.co.uk http://my.livewellwithpain.co.uk https://www.paintoolkit.org/resources/for-patients https://www.youtube.com/user/HunterBrainman/videos Once on the HunterBrainman videos page, choose the video clips below: • Understanding Pain in less than 5 minutes • Understanding Pain: Brainman Chooses There are many versions in different languages. Your mental health If you feel your pain condition is causing very high levels of distress please consider: www.moodjuice.scot.nhs.uk Breathing space 0800838587 Samaritans 08457909090 TAYSIDE PAIN SERVICE . -

12:34 Pm 12:34 Pm
www.dundee.com 12:34 PM 12:34 PM Download FREE for your Guide to Dundee One City, Many Discoveries www.dundee.com Words people most associate with Dundee: www.dundee.com Dundee is home to one of the most significant biomedical and life sciences communities in the UK outwith Oxford and Cambridge. Dundee has one of the highest student population ratios in the UK. At 1:5 with 50,000 studying within 30 minutes of the city. www.dundee.com Dundee was named the Global video game hits UK’s first UNESCO City Lemmings and Grand of Design by the United Theft Auto were created Nations in 2014. in Dundee. www.dundee.com The City of Design desig- nation has previously been HMS Unicorn is one of the oldest ships afloat in the world. Dundee boasts two 5-star award winning visitor attractions, namely Discovery Point and Scotland’s Jute Museum @ Verdant Works. In addition, other attractions include HMS Unicorn, Dundee Science Centre and Mills Observatory. www.dundee.com a few Broughty Castle Scotland’s Jute Museum Museum @ Verdant 01382 436916 Works 01382 309060 D’Arcy Thompson Zoology Museum HMS Frigate 01382 384310 Unicorn 01382 200900 The Population Tayside Medical of Dundee is History Museum Dundee Science currently 148,710 01382 384310 Centre with approximately 01382 228800 306,300 people RRS Discovery/ living within a 30 Discovery Point minute drive time. 01382 309060 www.dundee.com “Dundee is a little pot of gold at the end of the A92” - The Guardian Dundee is a cultural hive - both historical and contemporary. -

The Angus Care Model
THE ANGUS CARE MODEL Let’s keep the conversation going Thank you for your interest in the development of the Angus Care Model. During week beginning 16 October 2017 people from across Angus attended drop-in information sessions held in Forfar, Carnoustie, Montrose and Arbroath. These events gave locals the chance to talk to health and social care professionals. Our conversations focused on the challenges facing services, the opportunities for change and how we can together build a future Angus Care Model that provides the best possible care to the most people possible. The majority of people (85%) who attended the meetings found them helpful and informative. Whilst a small number of people commented that they would have preferred a formal meeting, people (94%) overwhelmingly felt that they had been given an opportunity to comment and offer their opinion. When arranging future meetings we will take account of people's suggestions and improve the way we raise awareness about the meetings. We were asked to share the information that was on display. In addition to talking to staff and have many of their questions answered, we also invited people to write down questions and leave comments. We have done our best to answer as many of the questions as possible. Please take some time to consider the information contained below and get involved in the conversation by completing a short survey https://www.surveymonkey.co.uk/r/WDFV53D or by contacting us on [email protected] We look forward to continuing our conversation with you in the very near future. -

Cultural Services Annual Report 2018
Leisure & Culture Dundee is a Scottish Charitable Incorporated Organisation No. SC042421 INTRODUCTION There have been many highlights to the year for In all our service delivery we work to Dundee Cultural Services, visitor numbers are up again Partnerships Local Outcome Improvement Plan across our facilities and we maintain very high and its strategic priorities for Dundee. These are satisfaction rates. Caird Hall has seen a significant aligned to; increase in attendance figures and The McManus: • Fair Work and Enterprise Dundee’s Art Gallery and Museum has recorded its highest yearly visits. • Children and Families • Health, Care and Wellbeing There have been a few challenges during the year and credit needs to go to staff for continuing • Community Safety and Justice to deliver a close to normal programme at Mills • Building Stronger Communities Observatory while the dome mechanism awaits repair. We continue to deliver our organisational values by being committed to service quality and This report offers a summary of a year in our life. excellence while actively sharing knowledge and Our four service delivery areas are: skills. We are also committed to ensuring equality and promoting diversity. • Halls and Music Development • Fine and Applied Art Ultimately, Cultural Services aims to support and promote cultural and creative learning activities, • Museum Services working to improve people’s quality of life. • Learning and Engagement As a service area, Cultural Services focus on the following LACD charitable purposes; • To advance the arts, heritage, culture and science • To advance education • To advance health • To advance citizenship/community development, including volunteering • To relieve those in need by reason of disadvantage FACTS AND FIGURES Scotland’s stars shone brightly in the Caird Hall 2018/19 season with The Proclaimers, Nicola Benedetti and Gerry Cinnamon all staging sell out Concerts. -

Dundee's Tree & Woodland Heritage
Dundee’s Tree Woodland Heritage& 1 A Green City Introduction This short publication aims to make residents and visitors more aware of Dundee’s rich arboricultural heritage. s Trees and woods provide a unique living t s e r legacy, reflecting the evolution of the City o l f a i c over the centuries. r e m m o e c l A visit to some of the sites listed will b a n i a provide glimpses into the history t s u of Dundee, and an introduction to d s n d a some colourful characters from the e g a n past; merchants, heroes, explorers, a y m l b revolutionaries, industrialists and i s n o everyday people. Every location has its p s e own part to play in making Dundee’s m r o r d f special sense of place. e c r u o l s a i r There can be few cities in the world e t a which can boast their own unique form s m n i a t of tree. Dundee is privileged in this n o n c respect to have the Camperdown Elm, o i t a c i now widely grown around the world as l b u a cultivar. This, along with the rest of s p i h n t Dundee’s rich green legacy, is something i r e p of which Dundonians should be a e p h justifiably proud. T The banks of the Dighty Burn 2 Contents A Brief History of Dundee’s Trees and Woods 4 Early History 6 The Growth of Dundee Western City and Approaches 8 Liff and Ninewells 9 University of Dundee Botanic Garden 10 Balgay Hill Woods 11 Menzieshill and South Road Park Camperdown and Clatto Area 12 Camperdown Country Park 13 Templeton Woods 14 Clatto Country Park 15 Lansdowne and Foggyley Aconites Perth Road Around the City Centre 16 City Centre and -

Dundee Dental Hospital and School Ninewells Hospital Dundee Other Training Site(S): Edinburgh Dental Institute Royal Hospital for Children Edinburgh
Specialist Dentistry ST1 Training Programme (Pre CCST) Job Description Post Details NES Recruitment Office: [email protected] Job Title: Pre CCST Paediatric Dentistry https://www.copdend.org/wp- Person Specification: content/uploads/2019/10/2020-Person- Specification-Paediatric-Dentistry-ST4.pdf Hours of work & nature of Contract: FT Main training site: Dundee Dental Hospital and School Ninewells Hospital Dundee Other training site(s): Edinburgh Dental Institute Royal Hospital for Children Edinburgh Organisational Arrangements Training Programme Director (TPD): Dr Katharine Blain TPD contact details: [email protected] Department Telephone number 01382 635964 University: University of Dundee Degree awarded: No specification to carry out formal University qualifications but under certain circumstances the post holder may consider completion of a Masters by Research or Masters in Education or Medical Education Time commitment: Nil University base fee What will What will What will 2020/21: I pay in I pay in I pay in 1st year? 2nd year? 3rd year? Bench fees : Page | 1 Training Details (Description of post) This is a pre-CCST which will provide training enabling the post holder to take their M. Paed. Dent. examination and become a registered Specialist in Paediatric Dentistry. Following this, they could opt to apply for further training to Consultant level or to work in Specialist practice e.g. in the PDS. The post is based primarily in Dundee Dental Hospital and School with a component of training being undertaken at Tayside Children’s Hospital (part of Ninewells in Dundee) with a link to both Edinburgh Dental Institute and Royal Hospital for Children in Edinburgh (to see more complex paediatric medical cases) being included in the latter part of the programme. -
Major Service Change a Report on NHS Tayside’S Consultation on Proposals for Shaping Orthopaedic Services
Major Service Change A report on NHS Tayside’s Consultation on proposals for Shaping Orthopaedic Services December 2019 Acknowledgements The Scottish Health Council would like to thank members of the public, patients, health and social care staff, local communities and groups for generously giving us their feedback and views on the engagement and consultation process. We would also like to thank NHS Tayside for the assistance they provided to us in reviewing the engagement process. We are committed to equality and strive to comply with the Equality Act 2010. If you would like to see this report in another language or format, please contact our Equality and Diversity Advisor on 0141 225 6871. © Healthcare Improvement Scotland 2019 Published December 2019 This document is licensed under the Creative Commons Attribution- NoncommercialNoDerivatives 4.0 International Licence. This allows for the copy and redistribution of this document as long as Healthcare Improvement Scotland is fully acknowledged and given credit. The material must not be remixed, transformed or built upon in any way. To view a copy of this licence, visit https://creativecommons.org/licenses/by-nc- nd/4.0/ www.scottishhealthcouncil.org Contents 1. Executive summary ........................................................................................................ 5 2. Our quality assurance: what we look for ......................................................................... 9 3. Introduction ................................................................................................................. -
Annual Performance Report
Dundee Health and Social Care Partnership Annual Performance Report 2019 - 2020 1 l Dundee Health and Social Care Partnership l Health and Social Care Annual Performance Report 2019-20 Health and Social Care Annual Performance Report 2019-20 l Dundee Health and Social Care Partnership l 1 2 l Dundee Health and Social Care Partnership l Health and Social Care Annual Performance Report 2019-20 Contents 1. Foreword ...........................................................................................................................................5 1.0 Who We Are ...............................................................................................................................7 1.1 How we measure our performance .........................................................................................10 1.2 How we deliver services in communities .................................................................................11 1.3 How we promote equalities and human rights ........................................................................12 1.4 How we engage and communicate with our stakeholders .......................................................13 2. Our Resources .................................................................................................................................16 2.1 Where our resources come from .............................................................................................16 2.2 How we have used our resources .............................................................................................17 -
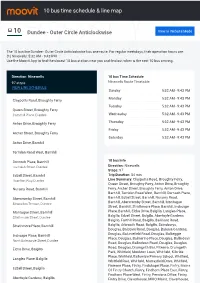
10 Bus Time Schedule & Line Route
10 bus time schedule & line map 10 Dundee - Outer Circle Anticlockwise View In Website Mode The 10 bus line Dundee - Outer Circle Anticlockwise has one route. For regular weekdays, their operation hours are: (1) Ninewells: 5:32 AM - 9:43 PM Use the Moovit App to ƒnd the closest 10 bus station near you and ƒnd out when is the next 10 bus arriving. Direction: Ninewells 10 bus Time Schedule 97 stops Ninewells Route Timetable: VIEW LINE SCHEDULE Sunday 5:32 AM - 9:43 PM Monday 5:32 AM - 9:43 PM Claypotts Road, Broughty Ferry Tuesday 5:32 AM - 9:43 PM Queen Street, Broughty Ferry Camphill Place, Dundee Wednesday 5:32 AM - 9:43 PM Anton Drive, Broughty Ferry Thursday 5:32 AM - 9:43 PM Friday 5:32 AM - 9:43 PM Archer Street, Broughty Ferry Saturday 5:32 AM - 9:43 PM Anton Drive, Barnhill Torridon Road West, Barnhill Dornoch Place, Barnhill 10 bus Info Lochalsh Street, Dundee Direction: Ninewells Stops: 97 Edzell Street, Barnhill Trip Duration: 84 min Hazelton Way, Dundee Line Summary: Claypotts Road, Broughty Ferry, Queen Street, Broughty Ferry, Anton Drive, Broughty Nursery Road, Barnhill Ferry, Archer Street, Broughty Ferry, Anton Drive, Barnhill, Torridon Road West, Barnhill, Dornoch Place, Abercromby Street, Barnhill Barnhill, Edzell Street, Barnhill, Nursery Road, Barnhill, Abercromby Street, Barnhill, Montague Stracathro Terrace, Dundee Street, Barnhill, Strathmore Place, Barnhill, Inchcape Montague Street, Barnhill Place, Barnhill, Elcho Drive, Balgillo, Langlea Place, Balgillo, Edzell Street, Balgillo, Aberfoyle Gardens, Strathmore Street, -

April 2011 (PDF)
The magazine of the University of Dundee • April 11 www.dundee.ac.uk/pressoffice Adapting to a changing worldcontact•april 11 1 contents news.................. ...03 from the principal... One of the most gratifying pieces of news to have been published over the past two months involving the University of Dundee was the Times Higher Education Survey of Student Experience which came out in mid-February. According to the opinions of our students, we are ranked the fifth best institution in the UK and the top University in Scotland in terms of the quality of our student experience; a measure which includes an assessment of the subject matters.......13 teaching quality, the structure of provision, welfare support as well as social factors such as the Students’ Association and sports facilities. Whilst one should always be cautious about the weight one gives to opinion polls and league tables of this kind, Dundee has nevertheless performed consistently well in this type of survey over recent years. It is my view that this Dundee best student experience in Scotland underscores the value we place on making sure our students are at the heart of our institution, but more importantly shows that our students think so, too. The University has been ranked top in Scotland and fifth in the “DUSA play an important role in the student experience, providing a As we move through difficult times we should take not a little comfort from this performance; UK in the recently published Times Higher Education Student central hub on campus with excellent social activities and valuable it proves to some extent that we are getting things right: our teaching staff are engaged and Experience Survey. -

39 Bus Time Schedule & Line Route
39 bus time schedule & line map 39 Arbroath, Saltire Centre - Kingoodie, The Green View In Website Mode The 39 bus line (Arbroath, Saltire Centre - Kingoodie, The Green) has 5 routes. For regular weekdays, their operation hours are: (1) Arbroath: 6:00 AM - 6:39 PM (2) Arbroath: 6:05 PM - 7:05 PM (3) Dundee City Centre: 5:17 AM - 5:35 PM (4) Kingoodie: 6:42 AM - 5:05 PM (5) Ninewells: 7:40 AM Use the Moovit App to ƒnd the closest 39 bus station near you and ƒnd out when is the next 39 bus arriving. Direction: Arbroath 39 bus Time Schedule 86 stops Arbroath Route Timetable: VIEW LINE SCHEDULE Sunday Not Operational Monday 6:00 AM - 6:39 PM The Green, Kingoodie Falkland Place, Scotland Tuesday 6:00 AM - 6:39 PM Woodland Way, Kingoodie Wednesday 6:00 AM - 6:39 PM Woodland Way, Scotland Thursday 6:00 AM - 6:39 PM Carse Place, Invergowrie Friday 6:00 AM - 6:39 PM Carse Place, Scotland Saturday 7:00 AM - 6:39 PM Station Road, Invergowrie Dryburgh Terrace, Invergowrie Primary School, Invergowrie 39 bus Info Direction: Arbroath Carselea Road, Invergowrie Stops: 86 Trip Duration: 56 min Greystane Road, Invergowrie Line Summary: The Green, Kingoodie, Woodland Way, Kingoodie, Carse Place, Invergowrie, Station Riverside Drive, Technology Park Road, Invergowrie, Dryburgh Terrace, Invergowrie, Apollo Way, Scotland Primary School, Invergowrie, Carselea Road, Invergowrie, Greystane Road, Invergowrie, Riverside Explorer Road, Technology Park Drive, Technology Park, Explorer Road, Technology Park, Medi Park, Technology Park, Carseview Centre, Medi Park,