Osteopathic Journal Feb 2006 6
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

General Pathomorpholog.Pdf
Ukrаiniаn Medicаl Stomаtologicаl Аcаdemy THE DEPАRTАMENT OF PАTHOLOGICАL АNАTOMY WITH SECTIONSL COURSE MАNUАL for the foreign students GENERАL PАTHOMORPHOLOGY Poltаvа-2020 УДК:616-091(075.8) ББК:52.5я73 COMPILERS: PROFESSOR I. STАRCHENKO ASSOCIATIVE PROFESSOR O. PRYLUTSKYI АSSISTАNT A. ZADVORNOVA ASSISTANT D. NIKOLENKO Рекомендовано Вченою радою Української медичної стоматологічної академії як навчальний посібник для іноземних студентів – здобувачів вищої освіти ступеня магістра, які навчаються за спеціальністю 221 «Стоматологія» у закладах вищої освіти МОЗ України (протокол №8 від 11.03.2020р) Reviewers Romanuk A. - MD, Professor, Head of the Department of Pathological Anatomy, Sumy State University. Sitnikova V. - MD, Professor of Department of Normal and Pathological Clinical Anatomy Odessa National Medical University. Yeroshenko G. - MD, Professor, Department of Histology, Cytology and Embryology Ukrainian Medical Dental Academy. A teaching manual in English, developed at the Department of Pathological Anatomy with a section course UMSA by Professor Starchenko II, Associative Professor Prylutsky OK, Assistant Zadvornova AP, Assistant Nikolenko DE. The manual presents the content and basic questions of the topic, practical skills in sufficient volume for each class to be mastered by students, algorithms for describing macro- and micropreparations, situational tasks. The formulation of tests, their number and variable level of difficulty, sufficient volume for each topic allows to recommend them as preparation for students to take the licensed integrated exam "STEP-1". 2 Contents p. 1 Introduction to pathomorphology. Subject matter and tasks of 5 pathomorphology. Main stages of development of pathomorphology. Methods of pathanatomical diagnostics. Methods of pathomorphological research. 2 Morphological changes of cells as response to stressor and toxic damage 8 (parenchimatouse / intracellular dystrophies). -

Unusual Multiple Cutaneous Retiform Hemangioendothelioma on Forearm
Clinical and Diagnostic Pathology Research Article Unusual multiple cutaneous retiform hemangioendothelioma on forearm and neck misdiagnosed as angiosarcoma with metastasis Bin-cai Pan1, Chun-hua Wang1, Gui-fang Huang1, Xiao-ying Tian2 and Zhi Li3* 1Department of Pathology, Guangdong Tongjiang Hospital, Nanguo East Road, Shunde district, Foshan 528300, China 2School of Chinese Medicine, Hong Kong Baptist University 7, Baptist University Road, Kowloon Tong, Hong Kong, China 3Department of Pathology, The First Affiliated Hospital, Sun Yat-sen university.58, Zhongshan Road II,Guangzhou 510080, China Abstract Retiform hemangioendothelioma (RH) is extremely rare, and often involves the skin and subcutaneous tissues of distal extremities in young adults or children. Since its first description by Calonje in 1994, only a few primary multiple cases have been described in the literature. We present a case of unusual primary multiple RH on forearm and neck occurring in a 56 years old female patient. The patient presented with a slow-growing cutaneous plaque-like lesion on her left forearm, followed by another lesion at the site of neck for several years. In the skin biopsy examination, a diagnosis of angiosarcoma with cutaneous metastasis was made based on multiple lesions at different anatomic sites and vasoformative growth pattern with anastomosing channels under the microscopy. However, postoperative histological diagnosis of the lesion was primary multiple RH by thoroughly microscopical inspection and the presence of thin-walled interconnecting vascular channels arranged in a retiform pattern and absence of lymph node metastasis. Despite wide surgical excision with tumor-free margin, the tumor recurred at the neck 3 months after surgery. -

Tumors and Tumor-Like Lesions of Blood Vessels 16 F.Ramon
16_DeSchepper_Tumors_and 15.09.2005 13:27 Uhr Seite 263 Chapter Tumors and Tumor-like Lesions of Blood Vessels 16 F.Ramon Contents 42]. There are two major classification schemes for vas- cular tumors. That of Enzinger et al. [12] relies on 16.1 Introduction . 263 pathological criteria and includes clinical and radiolog- 16.2 Definition and Classification . 264 ical features when appropriate. On the other hand, the 16.2.1 Benign Vascular Tumors . 264 classification of Mulliken and Glowacki [42] is based on 16.2.1.1 Classification of Mulliken . 264 endothelial growth characteristics and distinguishes 16.2.1.2 Classification of Enzinger . 264 16.2.1.3 WHO Classification . 265 hemangiomas from vascular malformations. The latter 16.2.2 Vascular Tumors of Borderline classification shows good correlation with the clinical or Intermediate Malignancy . 265 picture and imaging findings. 16.2.3 Malignant Vascular Tumors . 265 Hemangiomas are characterized by a phase of prolif- 16.2.4 Glomus Tumor . 266 eration and a stationary period, followed by involution. 16.2.5 Hemangiopericytoma . 266 Vascular malformations are no real tumors and can be 16.3 Incidence and Clinical Behavior . 266 divided into low- or high-flow lesions [65]. 16.3.1 Benign Vascular Tumors . 266 Cutaneous and subcutaneous lesions are usually 16.3.2 Angiomatous Syndromes . 267 easily diagnosed and present no significant diagnostic 16.3.3 Hemangioendothelioma . 267 problems. On the other hand, hemangiomas or vascular 16.3.4 Angiosarcomas . 268 16.3.5 Glomus Tumor . 268 malformations that arise in deep soft tissue must be dif- 16.3.6 Hemangiopericytoma . -

Lymphangioma Circumscriptum of the Vulva- a Case Series Dermatology Section
DOI: 10.7860/JCDR/2021/47435.14553 Case Series Lymphangioma Circumscriptum of the Vulva- A Case Series Dermatology Section RASHMI S MAHAJAN1, YOGESH S MARFATIA2, ATMAKALYANI R SHAH3, KISHAN R NINAMA4 ABSTRACT Vulval dermatoses pose a diagnostic and therapeutic challenge for the dermatologists. Lymphangioma Circumscriptum (LC) is a form of lymphangioma affecting the skin and subcutaneous tissues that is characterised by benign dilation of lymphatic channels. This uncommon condition is known to occur over the chest, mouth, axilla, tongue, and rarely in the vulva. In this series, authors present three cases of LC of vulva in women between the age group of 45 to 60 years with late-onset fluid-filled lesions over the vulva. The first case had history of hysterectomy prior to onset of lesions, the second case had a spontaneous onset of lesions while the third was a suspected case of pelvic tuberculosis with secondary lymphangioma. Keywords: Lymphangiectasia, Vulvar, Vulval epithelium INTRODUCTION Disorders of vulval epithelium are a confusing spectrum of disorders. They are broadly classified as-1) Inflammatory, 2) Ulcerative and Bullous, 3) Infections, 4) Benign tumours and 5) Malignancies. It is essential to know the exact aetiology to plan successful therapy. LC is a benign lymphatic malformation characterised by dilation of lymphatic vessels in the skin and subcutaneous tissue with lesions erupting locally as isolated or grouped translucid, thin-walled vesicles filled with a clear liquid [1]. These pathological lymphatic malformations have no communication with the normal lymphatics [2]. The precise cause of LC is not established. It could be congenital or acquired as a result of damage to the lymphatic vessels secondary to various aetiologies. -

Review Cutaneous Patterns Are Often the Only Clue to a a R T I C L E Complex Underlying Vascular Pathology
pp11 - 46 ABstract Review Cutaneous patterns are often the only clue to a A R T I C L E complex underlying vascular pathology. Reticulate pattern is probably one of the most important DERMATOLOGICAL dermatological signs of venous or arterial pathology involving the cutaneous microvasculature and its MANIFESTATIONS OF VENOUS presence may be the only sign of an important underlying pathology. Vascular malformations such DISEASE. PART II: Reticulate as cutis marmorata congenita telangiectasia, benign forms of livedo reticularis, and sinister conditions eruptions such as Sneddon’s syndrome can all present with a reticulate eruption. The literature dealing with this KUROSH PARSI MBBS, MSc (Med), FACP, FACD subject is confusing and full of inaccuracies. Terms Departments of Dermatology, St. Vincent’s Hospital & such as livedo reticularis, livedo racemosa, cutis Sydney Children’s Hospital, Sydney, Australia marmorata and retiform purpura have all been used to describe the same or entirely different conditions. To our knowledge, there are no published systematic reviews of reticulate eruptions in the medical Introduction literature. he reticulate pattern is probably one of the most This article is the second in a series of papers important dermatological signs that signifies the describing the dermatological manifestations of involvement of the underlying vascular networks venous disease. Given the wide scope of phlebology T and its overlap with many other specialties, this review and the cutaneous vasculature. It is seen in benign forms was divided into multiple instalments. We dedicated of livedo reticularis and in more sinister conditions such this instalment to demystifying the reticulate as Sneddon’s syndrome. There is considerable confusion pattern. -

Cutaneous Manifestations of Newborns in Omdurman Maternity Hospital
ﺑﺴﻢ اﷲ اﻟﺮﺣﻤﻦ اﻟﺮﺣﻴﻢ Cutaneous Manifestations of Newborns in Omdurman Maternity Hospital A thesis submitted in the partial fulfillment of the degree of clinical MD in pediatrics and child health University of Khartoum By DR. AMNA ABDEL KHALIG MOHAMED ATTAR MBBS University of Khartoum Supervisor PROF. SALAH AHMED IBRAHIM MD, FRCP, FRCPCH Department of Pediatrics and Child Health University of Khartoum University of Khartoum The Graduate College Medical and Health Studies Board 2008 Dedication I dedicate my study to the Department of Pediatrics University of Khartoum hoping to be a true addition to neonatal care practice in Sudan. i Acknowledgment I would like to express my gratitude to my supervisor Prof. Salah Ahmed Ibrahim, Professor of Peadiatric and Child Health, who encouraged me throughout the study and provided me with advice and support. I am also grateful to Dr. Osman Suleiman Al-Khalifa, the Dermatologist for his support at the start of the study. Special thanks to the staff at Omdurman Maternity Hospital for their support. I am also grateful to all mothers and newborns without their participation and cooperation this study could not be possible. Love and appreciation to my family for their support, drive and kindness. ii Table of contents Dedication i Acknowledgement ii Table of contents iii English Abstract vii Arabic abstract ix List of abbreviations xi List of tables xiii List of figures xiv Chapter One: Introduction & Literature Review 1.1 The skin of NB 1 1.2 Traumatic lesions 5 1.3 Desquamation 8 1.4 Lanugo hair 9 1.5 -

Eyelid Conjunctival Tumors
EYELID &CONJUNCTIVAL TUMORS PHOTOGRAPHIC ATLAS Dr. Olivier Galatoire Dr. Christine Levy-Gabriel Dr. Mathieu Zmuda EYELID & CONJUNCTIVAL TUMORS 4 EYELID & CONJUNCTIVAL TUMORS Dear readers, All rights of translation, adaptation, or reproduction by any means are reserved in all countries. The reproduction or representation, in whole or in part and by any means, of any of the pages published in the present book without the prior written consent of the publisher, is prohibited and illegal and would constitute an infringement. Only reproductions strictly reserved for the private use of the copier and not intended for collective use, and short analyses and quotations justified by the illustrative or scientific nature of the work in which they are incorporated, are authorized (Law of March 11, 1957 art. 40 and 41 and Criminal Code art. 425). EYELID & CONJUNCTIVAL TUMORS EYELID & CONJUNCTIVAL TUMORS 5 6 EYELID & CONJUNCTIVAL TUMORS Foreword Dr. Serge Morax I am honored to introduce this Photographic Atlas of palpebral and conjunctival tumors,which is the culmination of the close collaboration between Drs. Olivier Galatoire and Mathieu Zmuda of the A. de Rothschild Ophthalmological Foundation and Dr. Christine Levy-Gabriel of the Curie Institute. The subject is now of unquestionable importance and evidently of great interest to Ophthalmologists, whether they are orbital- palpebral specialists or not. Indeed, errors or delays in the diagnosis of tumor pathologies are relatively common and the consequences can be serious in the case of malignant tumors, especially carcinomas. Swift diagnosis and anatomopathological confirmation will lead to a treatment, discussed in multidisciplinary team meetings, ranging from surgery to radiotherapy. -

Reconstructive
RECONSTRUCTIVE Differential Diagnosis of Lower Extremity Enlargement in Pediatric Patients Referred with a Diagnosis of Lymphedema Carolyn C. Schook, B.A. Background: There are many causes for a large lower limb in the pediatric age John B. Mulliken, M.D. group. These children are often mislabeled as having lymphedema, and incor- Steven J. Fishman, M.D. rect diagnosis can lead to improper treatment. The purpose of this study was to Ahmad I. Alomari, M.D. determine the differential diagnosis in pediatric patients referred for lower Frederick D. Grant, M.D. extremity “lymphedema” and to clarify management. Arin K. Greene, M.D., Methods: The authors’ Vascular Anomalies Center database was reviewed be- M.M.Sc. tween 1999 and 2010 for patients referred with a diagnosis of lymphedema of Boston, Mass. the lower extremity. Records were studied to determine the correct cause for the enlarged extremity. Alternative diagnoses, sex, age of onset, and imaging studies were also analyzed. Results: A referral diagnosis of lower extremity lymphedema was given to 170 children; however, the condition was confirmed in only 72.9 percent of patients. Forty-six children (27.1 percent) had another disorder: microcystic/macrocystic lymphatic malformation (19.6 percent), noneponymous combined vascular malformation (13.0 percent), capillary malformation (10.9 percent), Klippel- Trenaunay syndrome (10.9 percent), hemihypertrophy (8.7 percent), posttrau- matic swelling (8.7 percent), Parkes Weber syndrome (6.5 percent), lipedema (6.5 percent), venous malformation (4.3 percent), rheumatologic disorder (4.3 percent), infantile hemangioma (2.2 percent), kaposiform hemangioendothe- lioma (2.2 percent), or lipofibromatosis (2.2 percent). -

Two Cases of Lymphangioma Circumscriptum Successfully Treated
Letters to the Editor REFERENCES 8. Kato N. Vertically growing ectopic nail. J Cutan Pathol 1992;19:445‑7. 9. Nath AK, Udayashankar C. Congenital onychogryphosis: Leaning Tower nail. Dermatol Online J 2011;17:9. 1. Barad P, Fernandes J, Ghodge R, Shukla P. Vertically growing Nail. 10. Zaias N. The Nail in Health and Disease. 2nd ed. Norwalk, CT: Appleton Indian Dermatol Online J 2015;6;288‑9. and Lange; 1990. p. 164. 2. Fleckman P. Structure and function of the nail unit. In: 3rd, editors. Nails: 11. Ohata C, Shirabe H, Takagi K. Onychogryphosis with granulation tissue Therapy, Diagnosis and Surgery :Saunders; 2005. p. 13‑26. of proximal nail fold. Skin Res 1996;38:626‑9. 3. Kligman AM. Why do nails grow out instead of up? Arch Dermatol 1961;84:313‑5. 4. Kikuchi I, Ogata K, Idemori M. Vertically growing ectopic nail: Nature’s Access this article online experiment on nail growth direction. J Am Acad Dermatol 1984;10:114‑6. Quick Response Code: 5. Baran R. Nail growth direction revisited. Why do nails grow out instead of up? J Am Acad Dermatol 1981;4:78‑84. 6. Grover C, Bansal S, Nanda S, Reddy BS, Kumar V. En bloc excision of Website: www.idoj.in proximal nail fold for treatment of chronic paronychia. Dermatol Surg 2006;32:393‑9. 7. Hashimoto K. Ultrastructure of the human toenail. I. Proximal nail matrix. J Invest Dermatol 1971;56:235‑46. Letter to the Editor twice per year. Nothing in particular was noted in her family Two cases of lymphangioma history or her laboratory tests. -
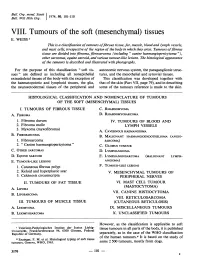
Mesenchymal) Tissues E
Bull. Org. mond. San 11974,) 50, 101-110 Bull. Wid Hith Org.j VIII. Tumours of the soft (mesenchymal) tissues E. WEISS 1 This is a classification oftumours offibrous tissue, fat, muscle, blood and lymph vessels, and mast cells, irrespective of the region of the body in which they arise. Tumours offibrous tissue are divided into fibroma, fibrosarcoma (including " canine haemangiopericytoma "), other sarcomas, equine sarcoid, and various tumour-like lesions. The histological appearance of the tamours is described and illustrated with photographs. For the purpose of this classification " soft tis- autonomic nervous system, the paraganglionic struc- sues" are defined as including all nonepithelial tures, and the mesothelial and synovial tissues. extraskeletal tissues of the body with the exception of This classification was developed together with the haematopoietic and lymphoid tissues, the glia, that of the skin (Part VII, page 79), and in describing the neuroectodermal tissues of the peripheral and some of the tumours reference is made to the skin. HISTOLOGICAL CLASSIFICATION AND NOMENCLATURE OF TUMOURS OF THE SOFT (MESENCHYMAL) TISSUES I. TUMOURS OF FIBROUS TISSUE C. RHABDOMYOMA A. FIBROMA D. RHABDOMYOSARCOMA 1. Fibroma durum IV. TUMOURS OF BLOOD AND 2. Fibroma molle LYMPH VESSELS 3. Myxoma (myxofibroma) A. CAVERNOUS HAEMANGIOMA B. FIBROSARCOMA B. MALIGNANT HAEMANGIOENDOTHELIOMA (ANGIO- 1. Fibrosarcoma SARCOMA) 2. " Canine haemangiopericytoma" C. GLOMUS TUMOUR C. OTHER SARCOMAS D. LYMPHANGIOMA D. EQUINE SARCOID E. LYMPHANGIOSARCOMA (MALIGNANT LYMPH- E. TUMOUR-LIKE LESIONS ANGIOMA) 1. Cutaneous fibrous polyp F. TUMOUR-LIKE LESIONS 2. Keloid and hyperplastic scar V. MESENCHYMAL TUMOURS OF 3. Calcinosis circumscripta PERIPHERAL NERVES II. TUMOURS OF FAT TISSUE VI. -

Classification of Thyroid Tumors Benign Tumors - Adenoma 1
DERMATOPATHOLOGY PATHOLOGY OF ENDOCRINE SYSTEM Thyroid carcinoma, Hashimoto thyroiditis, Graves‘ disease, neuroendocrine tumor, Institute of Pathological Anatomy melanoma, pigmented naevus, psoriasis, eczema FM CU BA DERMATOPATHOLOGY • 10-year-old boy with a pigmented lesion on his shoulder, sharply demarcated from the surrounding skin, with a diameter of 2.3 cm, dark brown in color, without noticeable changes. CASE NO. 1 ➢Suggested examinations? ➢Your diagnosis? ➢Describe the microscopic finding. Pigmented nevus of the skin Congenital pigmented nevus of the skin PIGMENTED NEVUS • benign skin formation arising as a result of melanocyte accumulation • the most common skin lesion of the white race • most nevi form in childhood and adolescence Classification of nevi according to the position of growth in the skin • Junctional nevus - nests of melanocytes are found at the dermo-epidermal junction • Mixed nevus - nests of melanocytes are found at the junction but also in the dermis • Intradermal nevus - clusters of melanocytes are found in the upper part of the dermis WITHOUT connection with the epidermis Histological variants of pigmented nevus • Congenital nevus • Blue nevus • Halo nevus • Familial dysplastic nevus Mixed pigmented nevus Junctional pigmented nevus Intradermal pigmented nevus • 73-year-old patient was admitted to hospital for progressive weakness, shortness of breath. You notice that both the skin and the sclera are icteric. • laboratory hyperbilirubinemia, hypoalbuminemia and mineral imbalance, positive oncomarkers (S100) • abdominal ultrasound with spherical structures found in the liver parenchyma • personal medical history - malignant melanoma of the eye CASE NO. 2 30 years ago, CLL 3 years ago, now in remission ➢Suggested examinations? ➢Your diagnosis? ➢Complications? ➢Describe the microscopic finding. -

Dermatopathology
Dermatopathology Clay Cockerell • Martin C. Mihm Jr. • Brian J. Hall Cary Chisholm • Chad Jessup • Margaret Merola With contributions from: Jerad M. Gardner • Talley Whang Dermatopathology Clinicopathological Correlations Clay Cockerell Cary Chisholm Department of Dermatology Department of Pathology and Dermatopathology University of Texas Southwestern Medical Center Central Texas Pathology Laboratory Dallas , TX Waco , TX USA USA Martin C. Mihm Jr. Chad Jessup Department of Dermatology Department of Dermatology Brigham and Women’s Hospital Tufts Medical Center Boston , MA Boston , MA USA USA Brian J. Hall Margaret Merola Department of Dermatology Department of Pathology University of Texas Southwestern Medical Center Brigham and Women’s Hospital Dallas , TX Boston , MA USA USA With contributions from: Jerad M. Gardner Talley Whang Department of Pathology and Dermatology Harvard Vanguard Medical Associates University of Arkansas for Medical Sciences Boston, MA Little Rock, AR USA USA ISBN 978-1-4471-5447-1 ISBN 978-1-4471-5448-8 (eBook) DOI 10.1007/978-1-4471-5448-8 Springer London Heidelberg New York Dordrecht Library of Congress Control Number: 2013956345 © Springer-Verlag London 2014 This work is subject to copyright. All rights are reserved by the Publisher, whether the whole or part of the material is concerned, specifi cally the rights of translation, reprinting, reuse of illustrations, recitation, broadcasting, reproduction on microfi lms or in any other physical way, and transmission or information storage and retrieval, electronic adaptation, computer software, or by similar or dissimilar methodology now known or hereafter developed. Exempted from this legal reservation are brief excerpts in connection with reviews or scholarly analysis or material supplied specifi cally for the purpose of being entered and executed on a computer system, for exclusive use by the purchaser of the work.