Endoscopic Colostomy with Percutaneous Colopexy
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Laparoscopic Gastropexy As a Preventative Measure for Gastric Dilation Volvulus in Canines
Laparoscopic Gastropexy as a Preventative Measure for Gastric Dilation Volvulus in Canines By: Erin O’Brien Advisors: Dr. Kimberly Boswell Board Certified Surgeon Southwest Michigan Animal Emergency Hospital Kalamazoo, MI Dr. Diane R. Kiino Ph.D. Kalamazoo College Health Science A paper submitted in partial fulfillment of the requirements for the degree of Bachelor of Arts at Kalamazoo College. 2010 ii ACKNOWLEDGEMENTS Over the summer I was able to intern at the Southwest Michigan Animal Emergency Hospital in Kalamazoo, MI. It was there that I was exposed to the emergency setting in veterinary medicine but also had the chance to observe surgeries done by Board Certified Surgeon, Dr. Kimberly Boswell. I would like to thank the entire staff at SWMAEH for teaching me a tremendous amount about veterinary medicine and allowing me to get as much hands on experience as possible. It was such a privilege to complete my internship at a hospital where I was able to learn so much about veterinary medicine in only ten weeks. I would also like to thank Dr. Boswell in particular, it was a gastropexy surgery I saw her perform during my internship that inspired the topic of this paper. Additionally I would like to acknowledge my advisor Dr. Diane Kiino for providing the direction I needed in choosing my paper topic. iii ABSTRACT Gastric Dilation Volvulus (GDV) is a fatal condition in canines especially those that are large or giant breeds. GDV results from the stomach distending and twisting on itself which when left untreated causes shock and ultimately death. The only method of prevention for GDV is a gastropexy, a surgical procedure that sutures the stomach to the abdominal wall to prevent volvulus or twisting. -

Small Bowel Obstruction After Laparoscopic Roux-En-Y Gastric Bypass Presenting As Acute Pancreatitis: a Case Report
Netherlands Journal of Critical Care Submitted January 2018; Accepted April 2018 CASE REPORT Small bowel obstruction after laparoscopic Roux-en-Y gastric bypass presenting as acute pancreatitis: a case report N. Henning1, R.K. Linskens2, E.E.M. Schepers-van der Sterren3, B. Speelberg1 Department of 1Intensive Care, 2Gastroenterology and Hepatology, and 3Surgery, Sint Anna Hospital, Geldrop, the Netherlands. Correspondence N. Henning - [email protected] Keywords - Roux-en-Y, gastric bypass, pancreatitis, pancreatic enzymes, small bowel obstruction, biliopancreatic limb obstruction. Abstract Small bowel obstruction is a common and potentially life-threatening bowel obstruction within this complication after laparoscopic Roux-en-Y gastric bypass surgery. population, because misdiagnosis We describe a 30-year-old woman who previously underwent can have disastrous outcomes.[1,3-5,7] gastric bypass surgery. She was admitted to the emergency In this report we describe the department with epigastric pain and elevated serum lipase levels. difficulty of diagnosing small Conservative treatment was started for acute pancreatitis, but she bowel obstruction in post- showed rapid clinical deterioration due to uncontrollable pain and LRYGB patients and why frequent excessive vomiting. An abdominal computed tomography elevated pancreatic enzymes scan revealed small bowel obstruction and surgeons performed can indicate an obstruction in an exploratory laparotomy with adhesiolysis. Our patient quickly these patients. The purpose of improved after surgery and could be discharged home. This case this manuscript is to emphasise report emphasises that in post-bypass patients with elevated Figure 1. Roux-en-Y gastric bypass that in post-bypass patients with pancreatic enzymes, small bowel obstruction should be considered ©Ethicon, Inc. -

Laparoscopic Fundoplication with Double Sided Posterior Gastropexy: a Different Surgical Technique
View metadata, citation and similar papers at core.ac.uk ORIGINAL RESEARCH brought to you by CORE provided by Elsevier - Publisher Connector International Journal of Surgery 10 (2012) 532e536 Contents lists available at SciVerse ScienceDirect International Journal of Surgery journal homepage: www.theijs.com Original research Laparoscopic fundoplication with double sided posterior gastropexy: A different surgical technique Fahri Yetis¸ira,*, A. Ebru Salman b,Dogukan Durak a, Mehmet Kiliç c a Ataturk Research and Training Hospital, General Surgery Department, Turkey b Ataturk Research and Training Hospital, Anesthesiology and Reanimation Department, Turkey c Yildirim Beyazit University, General Surgery Department, Turkey article info abstract Article history: Background: Laparoscopic Nissen Fundoplication has become the gold standard surgical procedure for Received 18 April 2012 management of gastroesophageal reflux disease. Nissen fundoplication provides an effective barrier Received in revised form against reflux. The aim of this study was to evaluate early postoperative outcomes of a different surgical 3 August 2012 technique, laparoscopic fundoplication with double sided posterior gastropexy. Accepted 6 August 2012 Methods: Data of 46 patients who underwent laparoscopic fundoplication with double sided posterior Available online 21 August 2012 gastropexy between February 2010 and December 2011 were collected. Surgically, after Nissen fundoplication was completed, 2e4 sutures were passed through the uppermost parts of the posterior Keywords: Gastropexy and anterior wall of the gastric wrap and then passed gently 1 cm above the celiac artery from the denser fi Nissen fundoplication bers of uppermost part of the arcuate ligament. Demographic data, preoperative and postoperative Gastroesophageal reflux assesments of sympthomatic and functional outcomes of patients were recorded. -

Modified Heller´S Esophageal Myotomy Associated with Dor's
Crimson Publishers Research Article Wings to the Research Modified Heller´s Esophageal Myotomy Associated with Dor’s Fundoplication A Surgical Alternative for the Treatment of Dolico Megaesophagus Fernando Athayde Veloso Madureira*, Francisco Alberto Vela Cabrera, Vernaza ISSN: 2637-7632 Monsalve M, Moreno Cando J, Charuri Furtado L and Isis Wanderley De Sena Schramm Department of General Surgery, Brazil Abstracts The most performed surgery for the treatment of achalasia is Heller´s esophageal myotomy associated or no with anti-reflux fundoplication. We propose in cases of advanced megaesophagus, specifically in the dolico megaesophagus, a technical variation. The aim of this study was to describe Heller´s myotomy modified by Madureira associated with Dor´s fundoplication as an alternative for the treatment of dolico megaesophagus,Materials and methods: assessing its effectiveness at through dysphagia scores and quality of life questionnaires. *Corresponding author: proposes the dissection ofTechnical the esophagus Note describing intrathoracic, the withsurgical circumferential procedure and release presenting of it, in the the results most of three patients with advanced dolico megaesophagus, operated from 2014 to 2017. The technique A. V. Madureira F, MsC, Phd. Americas Medical City Department of General extensive possible by trans hiatal route. Then the esophagus is retracted and fixed circumferentially in the Surgery, Full Professor of General pillars of the diaphragm with six or seven point. The goal is at least on the third part of the esophagus, to achieveResults: its broad mobilization and rectification of it; then is added a traditional Heller myotomy. Submission:Surgery At UNIRIO and PUC- Rio, Brazil Published: The mean dysphagia score in pre-op was 10points and in the post- op was 1.3 points (maximum October 09, 2019 of 10 points being observed each between the pre and postoperative 8.67 points, 86.7%) The mean October 24, 2019 hospitalization time was one day. -
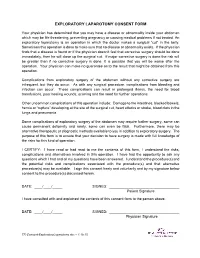
Exploratory Laparotomy.Docx
EXPLORATORY LAPAROTOMY CONSENT FORM Your physician has determined that you may have a disease or abnormality inside your abdomen which may be life threatening, preventing pregnancy or causing medical problems if not treated. An exploratory laparotomy is an operation in which the doctor makes a surgical “cut” in the belly. Sometimes this operation is done to make sure that no disease or abnormality exists. If the physician finds that a disease is found or if the physician doesn’t feel that corrective surgery should be done immediately, then he will close up the surgical cut. If major corrective surgery is done the risk will be greater than if no corrective surgery is done. It is possible that you will be worse after the operation. Your physician can make no guarantee as to the result that might be obtained from this operation. Complications from exploratory surgery of the abdomen without any corrective surgery are infrequent, but they do occur. As with any surgical procedure, complications from bleeding and infection can occur. These complications can result in prolonged illness, the need for blood transfusions, poor healing wounds, scarring and the need for further operations. Other uncommon complications of this operation include: Damage to the intestines, blocked bowels, hernia or “rupture” developing at the site of the surgical cut, heart attacks or stroke, blood clots in the lungs and pneumonia. Some complications of exploratory surgery of the abdomen may require further surgery, some can cause permanent deformity and rarely, some can even be fatal. Furthermore, there may be alternative therapeutic or diagnostic methods available to you in addition to exploratory surgery. -

The Short Esophagus—Lengthening Techniques
10 Review Article Page 1 of 10 The short esophagus—lengthening techniques Reginald C. W. Bell, Katherine Freeman Institute of Esophageal and Reflux Surgery, Englewood, CO, USA Contributions: (I) Conception and design: RCW Bell; (II) Administrative support: RCW Bell; (III) Provision of the article study materials or patients: RCW Bell; (IV) Collection and assembly of data: RCW Bell; (V) Data analysis and interpretation: RCW Bell; (VI) Manuscript writing: All authors; (VII) Final approval of manuscript: All authors. Correspondence to: Reginald C. W. Bell. Institute of Esophageal and Reflux Surgery, 499 E Hampden Ave., Suite 400, Englewood, CO 80113, USA. Email: [email protected]. Abstract: Conditions resulting in esophageal damage and hiatal hernia may pull the esophagogastric junction up into the mediastinum. During surgery to treat gastroesophageal reflux or hiatal hernia, routine mobilization of the esophagus may not bring the esophagogastric junction sufficiently below the diaphragm to provide adequate repair of the hernia or to enable adequate control of gastroesophageal reflux. This ‘short esophagus’ was first described in 1900, gained attention in the 1950 where various methods to treat it were developed, and remains a potential challenge for the contemporary foregut surgeon. Despite frequent discussion in current literature of the need to obtain ‘3 or more centimeters of intra-abdominal esophageal length’, the normal anatomy of the phrenoesophageal membrane, the manner in which length of the mobilized esophagus is measured, as well as the degree to which additional length is required by the bulk of an antireflux procedure are rarely discussed. Understanding of these issues as well as the extent to which esophageal shortening is due to factors such as congenital abnormality, transmural fibrosis, fibrosis limited to the esophageal adventitia, and mediastinal fixation are needed to apply precise surgical technique. -
![Spleen Rupture Complicating Upper Endoscopy in the Medical Literature [3–5]](https://docslib.b-cdn.net/cover/3489/spleen-rupture-complicating-upper-endoscopy-in-the-medical-literature-3-5-863489.webp)
Spleen Rupture Complicating Upper Endoscopy in the Medical Literature [3–5]
E206 UCTN – Unusual cases and technical notes following gastroscopy [3]. To our knowl- edge, only few cases have been reported Spleen rupture complicating upper endoscopy in the medical literature [3–5]. We think that the excessive stretching of spleno-diaphragmatic ligaments and of spleno-peritoneal lateral attachments Fig. 1 Computed during endoscopy and possibly the loca- tomography (CT) scan of abdomen in an 81- tion of most of the stomach in the thoracic year-old woman with cavity had contributed to the spleen rup- generalized weakness, ture [5,6]. Rapid diagnosis in the presence persistent nausea, and of suggestive symptoms of hemodynamic difficulty swallowing, instability and abdominal pain following showing hemoperito- upper endoscopy is life-saving. neum, subcapsular spleen hematoma, and blood around the liver. Endoscopy_UCTN_Code_CPL_1AH_2AJ Competing interests: None F. Jabr1, N. Skeik2 1 Hospital Medicine, Horizon Medical Center, Tennessee, USA 2 Vascular Medicine, Abott Northwestern An 81-year-old woman with history of peritoneum with subcapsular hematoma Hospital, Minneapolis, USA chronic lymphocytic leukemia and recent on the spleen (●" Fig. 1). The patient was diagnosis of Clostridium difficile colitis, diagnosed as having splenic rupture. Ex- and maintained on oral vancomycin, pre- ploratory laparotomy showed large he- References sented for generalized weakness, persis- moperitoneum (about 1500 mL blood), 1 Lopez-Tomassetti Fernandez EM, Delgado Plasencia L, Arteaga González IJ et al. Atrau- tent nausea, and a long history of difficulty subcapsular hematoma of the lateral in- matic rupture of the spleen: experience of swallowing (food hangs in her chest and ferior portion of the spleen, as well as a 10 cases. -

Abdominal Exploratory and Closure
Abdominal exploratory and closure 10.1 Diagnostic procedures 10.1.1 Paracentesis 10.1.1.1 Paracentesis technique 10.1.2 Enterocentesis 10.1.2.1 Enterocentesis technique 10.2 Opening of the abdominal cavity 10.2.1 Introduction 10.2.2 Position of the animal 10.2.3 Location of incision 10.2.4 Type of incision 10.2.4.1 Through-and-through incision 10.2.4.2 Complete grid Incision 10.2.4.3 Partial grid incision 10.2.5 Laparotomy in the bovine 10.2.5.1 Indications 10.2.5.2 Through-and-through incision 10.2.5.3 Partial grid incision 10.2.5.4 Complete grid incision 10.2.6 Laparotomy in small ruminants Chapter 10 10.2.7 Laparotomy in the horse 10.2.7.1 Indications 10.2.7.2 The median coeliotomy 10.2.7.3 The paramedian laparotomy 10.2.8 Coeliotomy in the dog and the cat 10.2.8.1 Indications 10.2.8.2 The median coeliotomy 10.2.8.3 The flank or paracostal incision 10.3 Minimally invasive techniques 10.4 Abdominal procedures 10.4.1 The rumen (bovine, small ruminants) 10.4.1.1 Introduction 10.4.1.2 Rumenotomy 10.4.2 The abomasum (bovine) 10.4.3 The stomach (horse, dog and cat) 10.4.3.1 Introduction 10.4.3.2 Gastrotomy in the dog and the cat 10.4.4 The small- and large intestines 10.4.4.1 Introduction 10.4.4.1.1 Simple mechanical ileus 10.4.4.1.2 Strangulating ileus 10.4.4.1.3 Paralytic ileus 10.4.4.2 Diagnostics 10.4.4.3 Therapy 10.4.4.3.1 Enterotomy 10.4.4.3.2 Enterectomy 10.4.5 The bladder 10.4.5.1 Introduction 10.4.5.2 Urolithiasis in bovine and equine 10.4.5.3 Cystotomy in the horse 10.4.5.3.1 Laparocystotomy 10.4.5.3.2 Pararectal cystotomy 10.4.5.4 Urolithiasis in the dog and the cat 10.4.5.5 Cystotomy in the dog and the cat 10.4.6 The uterus 10.4.6.1 Opening and closing of the uterus 10.4.6.2 Ovariectomy and ovariohysterectomy in dog and cat Chapter 10 176 Chapter 10 Abdominal exploratory and closure 10.1 Diagnostic procedures 10.1.1 Paracentesis paracentesis Paracentesis is the puncturing of the abdominal cavity. -

Advances in Flexible Endoscopy
Advances in Flexible Endoscopy Anant Radhakrishnan, DVM KEYWORDS Flexible endoscopy Minimally invasive procedures Gastroduodenoscopy Minimally invasive surgery KEY POINTS Although some therapeutic uses exist, flexible endoscopy is primarily used as a diagnostic tool. Several novel flexible endoscopic procedures have been studied recently and show prom- ise in veterinary medicine. These procedures provide the clinician with increased diagnostic capability. As the demand for minimally invasive procedures continues to increase, flexible endos- copy is being more readily investigated for therapeutic uses. The utility of flexible endoscopy in small animal practice should increase in the future with development of the advanced procedures summarized herein. INTRODUCTION The demand for minimally invasive therapeutic measures continues to increase in hu- man and veterinary medicine. Pet owners are increasingly aware of technology and diagnostic options and often desire the same care for their pet that they may receive if hospitalized. Certain diseases, such as neoplasia, hepatobiliary disease, pancreatic disease, and gastric dilatation–volvulus, can have significant morbidity associated with them such that aggressive, invasive measures may be deemed unacceptable. Even less severe chronic illnesses such as inflammatory bowel disease can be asso- ciated with frustration for the pet owner such that more immediate and detailed infor- mation regarding their pet’s disease may prove to be beneficial. Minimally invasive procedures that can increase diagnostic and therapeutic capability with reduced pa- tient morbidity will be in demand and are therefore an area of active investigation. The author has nothing to disclose. Department of Internal Medicine, Bluegrass Veterinary Specialists 1 Animal Emergency, 1591 Winchester Road, Suite 106, Lexington, KY 40505, USA E-mail address: [email protected] Vet Clin Small Anim 46 (2016) 85–112 http://dx.doi.org/10.1016/j.cvsm.2015.08.003 vetsmall.theclinics.com 0195-5616/16/$ – see front matter Ó 2016 Elsevier Inc. -

Exploratory Laparotomy Following Penetrating Abdominal Injuries: a Cohort Study from a Referral Hospital in Erbil, Kurdistan Region in Iraq
Exploratory laparotomy following penetrating abdominal injuries: a cohort study from a referral hospital in Erbil, Kurdistan region in Iraq Research protocol 1 November 2017 FINAL version Table of Contents Protocol Details .............................................................................................................. 3 Signatures of all Investigators Involved in the Study .................................................... 4 Summary ........................................................................................................................ 5 List of Abbreviations ..................................................................................................... 6 List of Definitions .......................................................................................................... 7 Background .................................................................................................................... 8 Justification .................................................................................................................... 9 Aim of Study .................................................................................................................. 9 Investigation Plan ......................................................................................................... 10 Study Population .......................................................................................................... 10 Data ............................................................................................................................. -

Digestive Endoscopy in Five Decades
■ COLLEGE LECTURES Digestive endoscopy in five decades Peter B Cotton ABSTRACT – The world of gastroenterology scopy. So-called semi-flexible gastroscopes were changed forever when flexible endoscopes cumbersome and used infrequently by only a few became available in the 1960s. Diagnostic and enthusiasts. therapeutic techniques proliferated and entered the mainstream of medicine, not without some Diagnostic endoscopy controversy. Success resulted in a huge service demand, with the need to train more endo- The first truly flexible gastroscope was developed in 1 This paper is scopists and to organise large endoscopy units the USA, following pioneering work on fibre-optic 2 based on the Lilly and teams of staff. The British health service light transmission in the UK by Harold Hopkins. Lecture given at struggled with insufficient numbers of consul- However, commercial production of endoscopes was the Royal College tants, other staff and resources, and British rapidly dominated by Japanese companies, building of Physicians on endoscopy fell behind that of most other devel- on their earlier expertise with intragastric cameras. 12 April 2005 by oped countries. This situation is now being My involvement began in 1968, whilst doing bench Peter B Cotton addressed aggressively, with many local and research with Dr Brian Creamer at St Thomas’ MD FRCP FRCS, national initiatives aimed at improving access and Hospital, London. An expert in coeliac disease (and Medical Director, choice, and at promoting and documenting jejunal biopsy), he opined that gastroscopy might Digestive Disease quality. Many more consultants are needed and become useful and legitimate only if it became pos- Center, Medical some should be relieved of their internal medi- sible to take target biopsy specimens – since no one University of South Carolina, cine commitment to focus on their specialist seriously believed what endoscopists said that they Charleston, USA skills. -

Duodenal Perforation Caused by Eyeglass Temples: a Case Report
Case Report Annals of Clinical Case Reports Published: 27 Jan, 2020 Duodenal Perforation Caused by Eyeglass Temples: A Case Report Zhiyong Dong1#, Wenhui Chen1#, Jin Gong1, Juncan Zhang1, Hina Mohsin2 and Cunchuan Wang1* 1Department of Gastrointestinal Surgery, The First Affiliated Hospital of Jinan University, China 2Department of Neurology, California University of Science and Medicine, USA #These authors contributed equally to this work Abstract Background: While some foreign bodies in the digestive system can be egested spontaneously or after ingesting lubricants, generally long, large, sharp, irregularly shaped, hardened and/or toxic foreign bodies frequently remain in the digestive system. These foreign bodies may cause obstruction or damage the gastrointestinal mucosa leading to bleeding, perforation, and/or acute peritonitis, and may even cause local abscess, fistula formation, or organ damage. Case Report: A 30-year-old Chinese man was presented with acute abdominal pain while intoxicated with alcohol and swallowed two eyeglass temples. Conservative measures including ingesting lubricants to egest the foreign bodies failed. He underwent two exploratory laparotomy that showed a duodenal perforation and eventually the two eyeglass temples retrieved. Conclusion: This is the first report describing a patient who had swallowed eyeglass temples. Patients who swallow such objects must be promptly examined and diagnosed by ultrasound, X-ray, and/or CT, and foreign bodies removed by laparoscopy or laparotomy. Keywords: Duodenal perforation; Foreign body; Exploratory laparotomy OPEN ACCESS Introduction *Correspondence: Cunchuan Wang, Department of The effects of foreign bodies in the digestive system depend on their texture, shape, size, toxicity, Gastrointestinal Surgery, The First retention site, and duration [1]. Report of foreign bodies includes dentures, glass beads, coins, pens, Affiliated Hospital of Jinan University, fish bones [2].