Two Novel Pathogenic Variants of L1CAM Gene in Two Fetuses with Isolated X‑Linked Hydrocephaly: a Case Report
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

MASA Syndrome in Twin Brothers: Case Report of Sixteen-Year Clinical Follow Up
Paediatr Croat. 2014;58:286-90 PRIKAZ BOLESNIKA / CASE REPORT www.paedcro.com http://dx.doi.org/10.13112/PC.2014.50 MASA syndrome in twin brothers: case report of sixteen-year clinical follow up Matilda Kovač Šižgorić1, Zlatko Sabol1, Filip Sabol2, Tonći Grmoja3, Svjetlana Bela Klancir1, Zdravka Gjergja1, Ljiljana Kipke Sabol1 MASA syndrome (OMIM 303350) is a rare X-linked recessive neurologic disorder, also called CRASH syndrome, spastic paraplegia 1 and Gareis-Mason syndrome. The acronym MASA describes four major signs: Mental retardation, Aphasia, Shuffl ing gait and Adducted thumbs. A more suitable name for this syndrome is L1 syndrome because the disorder has been associated with mutations in the neuronal cell adhesion molecule L1 (L1CAM) gene. The syndrome has severe symptoms in males, while females are carriers because only one X chromosome is aff ected. The aim of this report is to show similarities and diff erences in clinical manifestations between twins with the L1CAM gene mutation and to emphasize the importance of genetic counseling. Our patients were dizygotic twins born prematurely at 35 weeks of gestation. Pregnancy was complicated with early bleeding and gestational diabetes. Immediately after birth, hypertonia of lower extremities was observed in both twins. Sixteen-year clinical follow up showed spastic paraparetic form with shuffl ing gait, clumsiness, delayed speech development, lower intellectual functioning at the level of mild to moderate mental retarda- tion, primary nocturnal enuresis, behavioral and sleep disorder (more pronounced in the second twin). Magnetic resonance imaging of the brain showed complete agenesis of the corpus callosum, complete lack of the anterior commissure, and internal hydrocephalus. -

Hirschsprung Disease in an Infant with L1 Syndrome
Hirschsprung Disease in an Infant with L1 Syndrome: Report of a New Case and a Novel L1CAM Variant Teresa Andreone1 1Saint Louis University Care - The Physicians of Saint Louis University October 27, 2020 Abstract L1 syndrome is an X-linked disorder manifesting with congenital hydrocephalus, adducted thumbs and spasticity. There are rare cases of L1 syndrome and coincident Hirschsprung disease, with mutations in the L1CAM gene thought to underlie both. We present a novel pathogenic L1CAM variant in someone with L1 syndrome and Hirschsprung disease. Introduction The L1CAM gene encodes the membrane glycoprotein L1CAM, a calcium-independent cellular adhesion molecule involved in neuronal development. The L1CAM cell adhesion molecule is found on the X chromo- some in humans (and other mammals) and has a 1253 amino acid protein sequence. The extracellular portion is comprised of six immunoglobulin domains followed by five fibronectin type III domains which are con- nected to a small intracellular domain by a transmembrane helix (Figure 1). Mutations in theL1CAM gene cause L1 syndrome, which encompasses a spectrum of disease that includes four major X-linked conditions: X-linked congenital hydrocephalus due to stenosis of the aqueduct of Sylvius (HSAS; OMIM #307000); men- tal retardation, aphasia, shuffling gait and adducted thumbs syndrome (MASA; OMIM #303350); X-linked complicated hereditary spastic paraplegia type 1 (SPG1; OMIM#303350); and X-linked complicated agene- sis of the corpus callosum (OMIM #304100)1. More than 220 disease-causing variants in the L1CAM gene have been identified as causing the four major phenotypes of L1 syndrome2. Additionally, there are reports suggesting that additional mutations in L1CAM can cause mild behavioral and intellectual impairment3. -

University of Groningen Genetics of L1 Syndrome Vos, Yvonne Johanna
University of Groningen Genetics of L1 syndrome Vos, Yvonne Johanna IMPORTANT NOTE: You are advised to consult the publisher's version (publisher's PDF) if you wish to cite from it. Please check the document version below. Document Version Publisher's PDF, also known as Version of record Publication date: 2010 Link to publication in University of Groningen/UMCG research database Citation for published version (APA): Vos, Y. J. (2010). Genetics of L1 syndrome. [S.n.]. Copyright Other than for strictly personal use, it is not permitted to download or to forward/distribute the text or part of it without the consent of the author(s) and/or copyright holder(s), unless the work is under an open content license (like Creative Commons). Take-down policy If you believe that this document breaches copyright please contact us providing details, and we will remove access to the work immediately and investigate your claim. Downloaded from the University of Groningen/UMCG research database (Pure): http://www.rug.nl/research/portal. For technical reasons the number of authors shown on this cover page is limited to 10 maximum. Download date: 26-09-2021 Genetics Ll Syndr Yvonne Vos , ' Genetics of Ll syndrome Yvonne Johanna Vos Vos, Yvonne J Genetics of Ll syndrome Proefschrift Groningen ISBN: 978-90-367-4471-3 © Copyright 2010 Y.J. Vos All rights are reserved. No part of this publication may be reproduced, stored in a retrieval system, or transmittedin any form or by any means, without permission of the author. Cover: Bob Vos Lay-out: Helga de Graaf, Studio Eye Candy, Groningen (www.proefschrift.info) Printed by lpskamp Drukkers, Enschede Stellingen behorende bij het proefschrift Genetics of Ll syndrome -·-····· ---· ·· -�--;. -

The University of Chicago Genetic Services Laboratories
The University of Chicago Genetic Services Laboratories 5841 South Maryland Avenue, Room G701/MC0077, Chicago, IL 60637 Toll Free: 888.824.3637 | Local: 773.834.0555 | Fax: 773-702-9130 [email protected] | dnatesting.uchicago.edu | CLIA#: 14D0917593 | CAP#: 18827-49 QUICK GUIDE TO GENETIC TESTING TEST DISORDER CPT TAT COST Aceruloplasminemia testing CP sequencing 81406 4 weeks $2,200 Aceruloplasminemia CP deletion/duplication 81405 4 weeks $1,000 Albinism testing Albinism Sequencing Panel (20 genes sequencing)** 81407 8 weeks $3,500 Albinism Deletion/Duplication Panel (20 genes deletion/duplication analysis) 81407 6 weeks $2,500 Alstrom syndrome testing ALMS1 sequencing 81406 4 weeks $1,700 Alstrom syndrome ALMS1 deletion/duplication 81405 4 weeks $1,000 Alternating Hemiplegia of Childhood testing ATP1A3 sequencing Alternating hemiplegia of childhood 81406 4 weeks $2,025 Angelman syndrome MS-MLPA (detects methylation and deletions in 15q11- 81331 4 weeks $525 13) UPD 15 testing (requires samples from both parents 81402 4 weeks $540 also) Angelman syndrome Imprinting center deletion analysis 81403 4 weeks $450 UBE3A sequencing 81406 4 weeks $1,500 UBE3A deletion/duplication 81405 4 weeks $1,000 SLC9A6 sequencing 81406 4 weeks $1,500 X-linked Angelman-like syndrome SLC9A6 deletion/duplication 81405 4 weeks $1,000 Angelman Syndrome Tier 2 Panel ( MECP2,TCF4, SLC9A6 and UBE3A sequencing and 81479 4 weeks $4,400 deletion/duplication) Rett/Angelman Syndrome Sequencing Panel (21 genes sequencing)** 81407 8 weeks $4,400 Rett/Angelman -

Inheritest 500 PLUS
Inheritest® 500 PLUS 525 genes Specimen ID: 00000000010 Container ID: H0651 Control ID: Acct #: LCA-BN Phone: SAMPLE REPORT, F-630049 Patient Details Specimen Details Physician Details DOB: 01/01/1991 Date Collected: 08/05/2019 12:00 (Local) Ordering: Age (yyy/mm/dd): 028/07/04 Date Received: 08/06/2019 Referring: Gender: Female Date Entered: 08/06/2019 ID: Patient ID: 00000000010 Date Reported: 08/21/2019 15:29 (Local) NPI: Ethnicity: Unknown Specimen Type: Blood Lab ID: MNEGA Indication: Carrier screening Genetic Counselor: None SUMMARY: POSITIVE POSITIVE RESULTS DISORDER (GENE) RESULTS INTERPRETATION Spinal muscular atrophy AT RISK AT RISK to be a silent carrier (2+0). For ethnic-specific risk (SMN1) 2 copies of SMN1; positive for revisions see Methods/Limitations. Genetic counseling is NMID: NM_000344 c.*3+80T>G SNP recommended. Risk: AT INCREASED RISK FOR AFFECTED PREGNANCY. See Additional Clinical Information. NEGATIVE RESULTS DISORDER (GENE) RESULTS INTERPRETATION Cystic fibrosis NEGATIVE This result reduces, but does not eliminate the risk to be a (CFTR) carrier. NMID: NM_000492 Risk: NOT at an increased risk for an affected pregnancy. Fragile X syndrome NEGATIVE: Not a carrier of a fragile X expansion. (FMR1) 29 and 36 repeats NMID: NM_002024 Risk: NOT at an increased risk for an affected pregnancy. ALL OTHER DISORDERS NEGATIVE This result reduces, but does not eliminate the risk to be a carrier. Risk: The individual is NOT at an increased risk for having a pregnancy that is affected with one of the disorders covered by this test. For partner's gene-specific risks, visit www.integratedgenetics.com. -

Description and Clinical Validation of a Real-Time AI Diagnostic Companion for Fetal Ultrasound Examination
medRxiv preprint doi: https://doi.org/10.1101/2021.05.25.21257630; this version posted July 10, 2021. The copyright holder for this preprint (which was not certified by peer review) is the author/funder, who has granted medRxiv a license to display the preprint in perpetuity. All rights reserved. No reuse allowed without permission. Description and clinical validation of a real-time AI diagnostic companion for fetal ultrasound examination Julien J. STIRNEMANN1, Remi BESSON5, Emmanuel SPAGGIARI1,4, Sandra ROJO5, Frederic LOGE5, Helene PEYRO-SAINT-PAUL5, Stephanie ALLASSONNIERE2,3, Erwan LE PENNEC3,6, Yves VILLE1 1. Obstetrics and maternal-fetal medicine, Necker - Enfants Malades Hospital, AP-HP and EA7328 université de Paris, IMAGINE Institute 2. School of Medicine, université de Paris, INRIA EPI HEKA, INSERM UMR1138, Sorbonne université 3. Center for Applied Mathematics, Ecole Polytechnique. Institut Polytechnique de Paris 4. Department of Histology-Embryology and Cytogenetics, Unit of Embryo & Fetal Pathology, Necker-Enfants Malades Hospital, AP-HP and Paris Descartes University; INSERM UMR 1163, IMAGINE Institute. 5. SONIO SAS, 24 rue du Faubourg Saint-Jacques, 75014 Paris. 6. Xpop, INRIA Saclay Conflict of interest: JS, RB, ES, SA, ELP and YV are co-founders of the SONIO company. SR, FL and HPSP are employed by the SONIO company. Funding: None IRB : CERAPHP.5 #00011928 Correspondence: Pr Julien STIRNEMANN Maternité, Hôpital Necker Enfants Malades, 149 rue de Sevres 75015 Paris email: [email protected] phone: +33171196218 NOTE: This preprint reports new research that has not been certified by peer review and should not be used to guide clinical practice. medRxiv preprint doi: https://doi.org/10.1101/2021.05.25.21257630; this version posted July 10, 2021. -
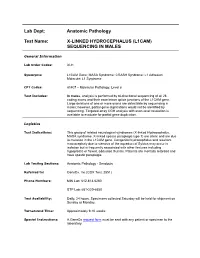
X-Linked Hydrocephalus (L1cam) Sequencing in Males
Lab Dept: Anatomic Pathology Test Name: X-LINKED HYDROCEPHALUS (L1CAM) SEQUENCING IN MALES General Information Lab Order Codes: XLH Synonyms: L1CAM Gene; MASA Syndrome; CRASH Syndrome; L1 Adhesion Molecule; L1 Syndrome CPT Codes: 81407 – Molecular Pathology, Level 8 Test Includes: In males, analysis is performed by bi-directional sequencing of all 28 coding exons and their exon/intron splice junctions of the L1CAM gene. Large deletions of one or more exons are detectable by sequencing in males; however, partial gene duplications would not be identified by sequencing. Targeted array CGH analysis with exon-level resolution is available to evaluate for partial gene duplication. Logistics Test Indications: This group of related neurological syndromes (X-linked Hydrocephalus, MASA syndrome, X-linked spastic paraplegia type 1) are allelic and are due to mutation in the L1CAM gene. Congenital hydrocephalus and resultant macrocephaly due to stenosis of the aqueduct of Sylvius may occur in isolation but is frequently associated with other features including hypoplastic or flexed, adducted thumbs. Patients are mentally retarded and have spastic paraplegia. Lab Testing Sections: Anatomic Pathology - Sendouts Referred to: GeneDx, Inc.(GDX Test: 2551) Phone Numbers: MIN Lab: 612-813-6280 STP Lab: 651-220-6550 Test Availability: Daily, 24 hours. Specimens collected Saturday will be held for shipment on Sunday or Monday. Turnaround Time: Approximately 9-10 weeks Special Instructions: A GeneDx request form must be sent with any patient or specimen to the laboratory. Specimen Specimen Type: Whole blood Container: Lavender top (EDTA) tube Draw Volume: 2 - 5 mL (Minimum: 1 mL) blood Processed Volume: Same as Draw Volume Collection: Routine blood collection Special Processing: Lab Staff: Send whole blood in original collection container, including signed consent form and requisition, with a cool pack in warm weather, via overnight or second-day courier so that the sample will arrive at GeneDx, Monday through Saturday. -

Download CGT Exome V2.0
CGT Exome version 2. -

Preimplantation Genetic Testing (Preimplantation Genetic Diagnosis and Preimplantation Genetic Screening)
bmchp.org | 888-566-0008 wellsense.org | 877-957-1300 Medical Policy Preimplantation Genetic Testing (Preimplantation Genetic Diagnosis and Preimplantation Genetic Screening) Policy Number: OCA 3.726 Version Number: 8 Version Effective Date: 11/01/16 + Product Applicability All Plan Products Well Sense Health Plan Boston Medical Center HealthNet Plan New Hampshire Medicaid MassHealth NH Health Protection Program Qualified Health Plans/ConnectorCare/Employer Choice Direct Senior Care Options + Note: Disclaimer and audit information is located at the end of this document. Policy Summary The Plan considers preimplantation genetic diagnosis (PGD) to be medically necessary when Plan criteria are met (as specified in the Medical Policy Statement and Limitations sections of this Plan policy). Prior authorization is required for all preimplantation genetic testing, including preimplantation genetic diagnosis (PGD) and preimplantation genetic screening (PGS); the Plan considers PGS to be experimental and investigational. It will be determined during the Plan’s prior authorization process if the service is considered medically necessary for the requested indication. See the Plan policy, Medically Necessary (policy number OCA 3.14), for the product-specific definitions of medically necessary treatment. Also, see the following Plan policies for medical guidelines, applicable definitions, and prior authorization requirements for BMC HealthNet Plan members (available at www.bmchp.org): Experimental and Investigational Treatment (policy number OCA 3.12), Infertility Services (policy number OCA 3.725), and Genetic Testing Guidelines and Pharmacogenetics (policy number OCA 3.726). Preimplantation Genetic Testing (Preimplantation Genetic Diagnosis and Preimplantation Genetic Screening) + Plan refers to Boston Medical Center Health Plan, Inc. and its affiliates and subsidiaries offering health coverage plans to enrolled members. -

DISEASE GENE GHI CHÚ 1 17-Beta-Hydroxysteroid Dehydrogenase Defciency, Type HSD17B3 III 2 3-Hydroxy-3-Methylglutaryl-Coa Lyase Deficiency HMGCL
# DISEASE GENE GHI CHÚ 1 17-beta-hydroxysteroid dehydrogenase defciency, type HSD17B3 III 2 3-Hydroxy-3-methylglutaryl-CoA lyase deficiency HMGCL 3 3-hydroxyacyl-CoA dehydrogenase defciency HADH 4 3-hydroxyisobutryl-CoA hydrolase deficiency HIBCH 5 3-Ketothiolase deficiency ACAT1 6 3-methylglutaconic aciduria AUH, DNAJC19 7 46, XX sex reversal 4 NR5A1 46XY sex reversal 3 8 Aarskog-Scott syndrome FGD1 9 ABCD syndrome EDNRB 10 Achalasia-addisonianism-alacrima syndrome AAAS 11 Achondrogenesis, type IB SLC26A2 12 Acyl-CoA dehydrogenase-9 (ACAD9) Deficiency ACAD9 13 Adenosine deaminase deficiency ADA 14 Adrenal insufficiency, congenital, with 46XY sex CYP11A1 reversal, partial or complete 15 Adrenocortical insufficiency NR5A1 16 Adrenoleukodystrophy, X-linked ABCD1 17 Afibrinogenemia, congenital FGA 18 Agammaglobulinemia, X-linked 1 BTK Agammaglobulinemia and isolated hormone deficiency 19 Aicardi-Goutieres syndrome RNASEH2A, RNASEH2B, RNASEH2C, SAMHD1, TREX1 20 Allan-Herndon-Dudley syndrome SLC16A2 21 Alpers-Huttenlocher syndrome POLG 22 Alpha thalassemia HBA1, ATRX ATRX (Alpha thalassemia X- linked intellectual disability syndrome) 23 Alpha-mannosidosis MAN2B1 24 Alpha-methylacyl-CoA racemase deficiency AMACR 25 Alport syndrome COL4A3, COL4A4, COL4A5 26 Alstrom syndrome ALMS1 27 Amish infantile epilepsy syndrome ST3GAL5 28 Amyotrophic lateral sclerosis ALS2 29 Anauxetic dysplasia RMRP 30 Andermann syndrome SLC12A6 31 Androgen insensitivity syndrome AR 32 Angelman syndrome UBE3A 33 Antley-Bixler syndrome with genital anomalies and POR disordered -

Preimplantation Genetic Testing (Preimplantation Genetic Diagnosis and Preimplantation Genetic Screening)
bmchp.org | 888-566-0008 wellsense.org | 877-957-1300 Medical Policy Preimplantation Genetic Testing (Preimplantation Genetic Diagnosis and Preimplantation Genetic Screening) Policy Number: OCA 3.726 Version Number: 9 Version Effective Date: 09/01/17 Product Applicability All Plan+ Products Well Sense Health Plan Boston Medical Center HealthNet Plan New Hampshire Medicaid MassHealth NH Health Protection Program Qualified Health Plans/ConnectorCare/Employer Choice Direct Senior Care Options + Note: Disclaimer and audit information is located at the end of this document. Policy Summary The Plan considers preimplantation genetic diagnosis to be medically necessary when Plan criteria are met (as specified in the Medical Policy Statement and Limitations sections of this Plan policy). Prior authorization is required for all preimplantation genetic testing, including preimplantation genetic diagnosis and preimplantation genetic screening. The Plan considers preimplantation genetic screening to be experimental and investigational. It will be determined during the Plan’s prior authorization process if the service is considered medically necessary for the requested indication. See the Plan policy, Medically Necessary (policy number OCA 3.14), for the product-specific definitions of medically necessary treatment. The Plan complies with coverage guidelines for all applicable state-mandated benefits and federally-mandated benefits that are medically necessary for the member’s condition. Review the following Plan medical policies for clinical review criteria, applicable definitions, and prior authorization requirements for BMC HealthNet Plan members (available at www.bmchp.org): Experimental and Investigational Treatment (policy Preimplantation Genetic Testing (Preimplantation Genetic Diagnosis and Preimplantation Genetic Screening) + Plan refers to Boston Medical Center Health Plan, Inc. and its affiliates and subsidiaries offering health coverage plans to enrolled members. -

HSAS(X-Linked Hydrocephalus with Stenosis of the Aqueduct of Sylvius) and Adducted Thumbs
Open Journal of Clinical & Medical Volume 1 (2015) Issue 6 Case Reports ISSN: 2379-1039 5 Week Old Boy with L1 Syndrome: HSAS(X-Linked Hydrocephalus with Stenosis of the Aqueduct of Sylvius) and Adducted Thumbs Kallol K Set, MD Children's Hospital of Michigan, Wayne State University School of Medicine, Detroit, MI, USA Email: [email protected] Introduction & Background Knowledge In each cell of our body, we have 23 pairs of chromosomes. We inherit half of our chromosomes from our mother and half from our father. Twenty-two of those pairs are the same between males and females. The last pair of chromosomes is the sex chromosomes. Males have one X and one Y chromosome; females have two X chromosomes. As the L1CAM gene is located on the X-chromosome, in females, when there is a mutation in one copy of the L1CAM gene on one of the X chromosomes, there is another copy of the gene located on the other X chromosome that can compensate for the mutated copy. No features of L1 syndrome are seen and the female is called a “carrier” of the condition. In males, there is only one copy of the L1CAM gene because there is only one X chromosome. When there is a mutation in this copy of L1CAM, no back-up copy exists and we see features of L1 syndrome. L1 syndrome can be further broken down into groups of different features that tend to be seen together e.g. X-Linked Hydrocephalus with Stenosis of the Aqueduct of Sylvius (HSAS). Image Description 5 week-old boy delivered at 38 weeks gestational age via cesarean section secondary to hydrocephalus noted on prenatal ultrasound.