Treating Pain in Diabetic Neuropathy: Current and Developmental Drugs
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Summary Analgesics Dec2019
Status as of December 31, 2019 UPDATE STATUS: N = New, A = Advanced, C = Changed, S = Same (No Change), D = Discontinued Update Emerging treatments for acute and chronic pain Development Status, Route, Contact information Status Agent Description / Mechanism of Opioid Function / Target Indication / Other Comments Sponsor / Originator Status Route URL Action (Y/No) 2019 UPDATES / CONTINUING PRODUCTS FROM 2018 Small molecule, inhibition of 1% diacerein TWi Biotechnology / caspase-1, block activation of 1 (AC-203 / caspase-1 inhibitor Inherited Epidermolysis Bullosa Castle Creek Phase 2 No Topical www.twibiotech.com NLRP3 inflamasomes; reduced CCP-020) Pharmaceuticals IL-1beta and IL-18 Small molecule; topical NSAID Frontier 2 AB001 NSAID formulation (nondisclosed active Chronic low back pain Phase 2 No Topical www.frontierbiotech.com/en/products/1.html Biotechnologies ingredient) Small molecule; oral uricosuric / anti-inflammatory agent + febuxostat (xanthine oxidase Gout in patients taking urate- Uricosuric + 3 AC-201 CR inhibitor); inhibition of NLRP3 lowering therapy; Gout; TWi Biotechnology Phase 2 No Oral www.twibiotech.com/rAndD_11 xanthine oxidase inflammasome assembly, reduced Epidermolysis Bullosa Simplex (EBS) production of caspase-1 and cytokine IL-1Beta www.arraybiopharma.com/our-science/our-pipeline AK-1830 Small molecule; tropomyosin Array BioPharma / 4 TrkA Pain, inflammation Phase 1 No Oral www.asahi- A (ARRY-954) receptor kinase A (TrkA) inhibitor Asahi Kasei Pharma kasei.co.jp/asahi/en/news/2016/e160401_2.html www.neurosmedical.com/clinical-research; -

About Pain Pharmacology: What Pain Physicians Should Know Kyung-Hoon Kim1, Hyo-Jung Seo1, Salahadin Abdi2, and Billy Huh2
Korean J Pain 2020;33(2):108-120 https://doi.org/10.3344/kjp.2020.33.2.108 pISSN 2005-9159 eISSN 2093-0569 Review Article All about pain pharmacology: what pain physicians should know Kyung-Hoon Kim1, Hyo-Jung Seo1, Salahadin Abdi2, and Billy Huh2 1Department of Anesthesia and Pain Medicine, School of Medicine, Pusan National University, Yangsan, Korea 2Department of Pain Medicine, The University of Texas MD Anderson Cancer Center, Houston, TX, USA Received February 8, 2020 Revised March 12, 2020 From the perspective of the definition of pain, pain can be divided into emotional Accepted March 13, 2020 and sensory components, which originate from potential and actual tissue dam- age, respectively. The pharmacologic treatment of the emotional pain component Correspondence includes antianxiety drugs, antidepressants, and antipsychotics. The anti-anxiety Kyung-Hoon Kim drugs have anti-anxious, sedative, and somnolent effects. The antipsychotics are Department of Anesthesia and Pain effective in patients with positive symptoms of psychosis. On the other hand, the Medicine, Pusan National University sensory pain component can be divided into nociceptive and neuropathic pain. Yangsan Hospital, 20 Geumo-ro, Non-steroidal anti-inflammatory drugs (NSAIDs) and opioids are usually applied for Mulgeum-eup, Yangsan 50612, Korea Tel: +82-55-360-1422 somatic and visceral nociceptive pain, respectively; anticonvulsants and antide- Fax: +82-55-360-2149 pressants are administered for the treatment of neuropathic pain with positive and E-mail: [email protected] negative symptoms, respectively. The NSAIDs, which inhibit the cyclo-oxygenase pathway, exhibit anti-inflammatory, antipyretic, and analgesic effects; however, they have a therapeutic ceiling. -

Classification Decisions Taken by the Harmonized System Committee from the 47Th to 60Th Sessions (2011
CLASSIFICATION DECISIONS TAKEN BY THE HARMONIZED SYSTEM COMMITTEE FROM THE 47TH TO 60TH SESSIONS (2011 - 2018) WORLD CUSTOMS ORGANIZATION Rue du Marché 30 B-1210 Brussels Belgium November 2011 Copyright © 2011 World Customs Organization. All rights reserved. Requests and inquiries concerning translation, reproduction and adaptation rights should be addressed to [email protected]. D/2011/0448/25 The following list contains the classification decisions (other than those subject to a reservation) taken by the Harmonized System Committee ( 47th Session – March 2011) on specific products, together with their related Harmonized System code numbers and, in certain cases, the classification rationale. Advice Parties seeking to import or export merchandise covered by a decision are advised to verify the implementation of the decision by the importing or exporting country, as the case may be. HS codes Classification No Product description Classification considered rationale 1. Preparation, in the form of a powder, consisting of 92 % sugar, 6 % 2106.90 GRIs 1 and 6 black currant powder, anticaking agent, citric acid and black currant flavouring, put up for retail sale in 32-gram sachets, intended to be consumed as a beverage after mixing with hot water. 2. Vanutide cridificar (INN List 100). 3002.20 3. Certain INN products. Chapters 28, 29 (See “INN List 101” at the end of this publication.) and 30 4. Certain INN products. Chapters 13, 29 (See “INN List 102” at the end of this publication.) and 30 5. Certain INN products. Chapters 28, 29, (See “INN List 103” at the end of this publication.) 30, 35 and 39 6. Re-classification of INN products. -

(ESRA) Congress 2018: E-Poster Viewing Abstracts
ABSTRACTS Abstracts and Highlight Papers of the 37th Annual European Society of Regional Anaesthesia & Pain Therapy (ESRA) 09/12/2018 on 1ojZViL9JnKxduCRhL/CcUAdyL6WwH5REYdVcwxqSc9xlxx/plvdjx0D6qkdcm/unXYqc/pwzsZMkY20jLisd3HCPQMoaMFxd03QOXvy15geUE+CR4J9Wp+ug9E5C+r4spJuQLeaJ8i4wLCpNFrgQgvjevOlNs34 by https://journals.lww.com/rapm from Downloaded Congress 2018: E-Poster Viewing Abstracts Downloaded Background and Aims: Deviation of the spinal needle leads to technical dif- from ESRA8-0027 ficulties and can cause neurological complications. The aims of this study are, https://journals.lww.com/rapm E-POSTER VIEWING first, to verify in clinical conditions the results from in vitro studies that the de- viation of the cutting type spinal needle depends on the mutual position of the CENTRAL NERVE BLOCKS bevels (its own and that of the introducer); and second, to compare the incidence of paresthesia with two accesses - median or paramedian. ≥ COMPARING RESISTANCE TO WATER FLOW BETWEEN Methods: 210 patients, aged 18 years, presented for elective surgery were in- TWO SPINAL NEEDLES cluded in a prospective randomised study. Spinal anesthesia in all patients was by performed in a lateral position with 88 mm 25G Quincke with 38 mm 20G in- 1ojZViL9JnKxduCRhL/CcUAdyL6WwH5REYdVcwxqSc9xlxx/plvdjx0D6qkdcm/unXYqc/pwzsZMkY20jLisd3HCPQMoaMFxd03QOXvy15geUE+CR4J9Wp+ug9E5C+r4spJuQLeaJ8i4wLCpNFrgQgvjevOlNs34 Al-Ani T. Queen Elizabeth University Hospital, Anaesthesia, Glasgow, United Kingdom. troducer at L2-3 or L3-4. Paresthesia and the number of attempts have been doc- Background and Aims: This study compares resistance to water flow be- umented. Patient Randomization is a web-based Mersenne Twister algorithm at  tween the newly introduced Pajunk Sprotte® NRFit 25G 90mm spinal needle a 1:1 allocation.  and our department previously used Vygon Whitacre 25G 90mm spinal needle. -
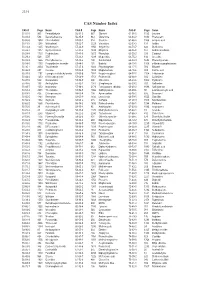
CAS Number Index
2334 CAS Number Index CAS # Page Name CAS # Page Name CAS # Page Name 50-00-0 905 Formaldehyde 56-81-5 967 Glycerol 61-90-5 1135 Leucine 50-02-2 596 Dexamethasone 56-85-9 963 Glutamine 62-44-2 1640 Phenacetin 50-06-6 1654 Phenobarbital 57-00-1 514 Creatine 62-46-4 1166 α-Lipoic acid 50-11-3 1288 Metharbital 57-22-7 2229 Vincristine 62-53-3 131 Aniline 50-12-4 1245 Mephenytoin 57-24-9 1950 Strychnine 62-73-7 626 Dichlorvos 50-23-7 1017 Hydrocortisone 57-27-2 1428 Morphine 63-05-8 127 Androstenedione 50-24-8 1739 Prednisolone 57-41-0 1672 Phenytoin 63-25-2 335 Carbaryl 50-29-3 569 DDT 57-42-1 1239 Meperidine 63-75-2 142 Arecoline 50-33-9 1666 Phenylbutazone 57-43-2 108 Amobarbital 64-04-0 1648 Phenethylamine 50-34-0 1770 Propantheline bromide 57-44-3 191 Barbital 64-13-1 1308 p-Methoxyamphetamine 50-35-1 2054 Thalidomide 57-47-6 1683 Physostigmine 64-17-5 784 Ethanol 50-36-2 497 Cocaine 57-53-4 1249 Meprobamate 64-18-6 909 Formic acid 50-37-3 1197 Lysergic acid diethylamide 57-55-6 1782 Propylene glycol 64-77-7 2104 Tolbutamide 50-44-2 1253 6-Mercaptopurine 57-66-9 1751 Probenecid 64-86-8 506 Colchicine 50-47-5 589 Desipramine 57-74-9 398 Chlordane 65-23-6 1802 Pyridoxine 50-48-6 103 Amitriptyline 57-92-1 1947 Streptomycin 65-29-2 931 Gallamine 50-49-7 1053 Imipramine 57-94-3 2179 Tubocurarine chloride 65-45-2 1888 Salicylamide 50-52-2 2071 Thioridazine 57-96-5 1966 Sulfinpyrazone 65-49-6 98 p-Aminosalicylic acid 50-53-3 426 Chlorpromazine 58-00-4 138 Apomorphine 66-76-2 632 Dicumarol 50-55-5 1841 Reserpine 58-05-9 1136 Leucovorin 66-79-5 -

Mirogabalin: Could It Be the Next Generation Gabapentin Or Pregabalin? Jae-Yeon Kim1, Salahadin Abdi2, Billy Huh2, and Kyung-Hoon Kim1
Korean J Pain 2021;34(1):4-18 https://doi.org/10.3344/kjp.2021.34.1.4 pISSN 2005-9159 eISSN 2093-0569 Review Article Mirogabalin: could it be the next generation gabapentin or pregabalin? Jae-Yeon Kim1, Salahadin Abdi2, Billy Huh2, and Kyung-Hoon Kim1 1Department of Anesthesia and Pain Medicine, Pusan National University School of Medicine, Yangsan, Korea 2Department of Pain Medicine, The University of Texas MD Anderson Cancer Center, Houston, TX, USA Received November 30, 2020 Revised December 15, 2020 Except for carbamazepine for trigeminal neuralgia, gabapentinoid anticonvulsants Accepted December 22, 2020 have been the standard for the treatment of neuropathic pain. Pregabalin, which followed gabapentin, was developed with the benefit of rapid peak blood concen- Handling Editor: Francis S. Nahm tration and better bioavailability. Mirogabalin besylate (DS-5565, Tarlige®) shows greater sustained analgesia due to a high affinity to, and slow dissociation from, the Correspondence α2δ-1 subunits in the dorsal root ganglion (DRG). Additionally, it produces a lower Kyung-Hoon Kim level of central nervous system-specific adverse drug reactions (ADRs), due to a low Pain Clinic, Pusan National University affinity to, and rapid dissociation from, the α δ-2 subunits in the cerebellum. Maxi- Yangsan Hospital, 20 Geumo-ro, 2 mum plasma concentration is achieved in less than 1 hour, compared to 1 hour Mulgeum-eup, Yangsan 50612, Korea Tel: +82-55-360-1422 for pregabalin and 3 hours for gabapentin. The plasma protein binding is relatively Fax: +82-55-360-2149 low, at less than 25%. As with all gabapentinoids, it is also largely excreted via the E-mail: [email protected] kidneys in an unchanged form, and so the administration dose should also be ad- justed according to renal function. -

Patent Application Publication ( 10 ) Pub . No . : US 2019 / 0192440 A1
US 20190192440A1 (19 ) United States (12 ) Patent Application Publication ( 10) Pub . No. : US 2019 /0192440 A1 LI (43 ) Pub . Date : Jun . 27 , 2019 ( 54 ) ORAL DRUG DOSAGE FORM COMPRISING Publication Classification DRUG IN THE FORM OF NANOPARTICLES (51 ) Int . CI. A61K 9 / 20 (2006 .01 ) ( 71 ) Applicant: Triastek , Inc. , Nanjing ( CN ) A61K 9 /00 ( 2006 . 01) A61K 31/ 192 ( 2006 .01 ) (72 ) Inventor : Xiaoling LI , Dublin , CA (US ) A61K 9 / 24 ( 2006 .01 ) ( 52 ) U . S . CI. ( 21 ) Appl. No. : 16 /289 ,499 CPC . .. .. A61K 9 /2031 (2013 . 01 ) ; A61K 9 /0065 ( 22 ) Filed : Feb . 28 , 2019 (2013 .01 ) ; A61K 9 / 209 ( 2013 .01 ) ; A61K 9 /2027 ( 2013 .01 ) ; A61K 31/ 192 ( 2013. 01 ) ; Related U . S . Application Data A61K 9 /2072 ( 2013 .01 ) (63 ) Continuation of application No. 16 /028 ,305 , filed on Jul. 5 , 2018 , now Pat . No . 10 , 258 ,575 , which is a (57 ) ABSTRACT continuation of application No . 15 / 173 ,596 , filed on The present disclosure provides a stable solid pharmaceuti Jun . 3 , 2016 . cal dosage form for oral administration . The dosage form (60 ) Provisional application No . 62 /313 ,092 , filed on Mar. includes a substrate that forms at least one compartment and 24 , 2016 , provisional application No . 62 / 296 , 087 , a drug content loaded into the compartment. The dosage filed on Feb . 17 , 2016 , provisional application No . form is so designed that the active pharmaceutical ingredient 62 / 170, 645 , filed on Jun . 3 , 2015 . of the drug content is released in a controlled manner. Patent Application Publication Jun . 27 , 2019 Sheet 1 of 20 US 2019 /0192440 A1 FIG . -

Heightened Misuse Risk and Addictive Potential of Gabapentinoids: the Fate of Effective Anxiolytics
DOI: 10.14744/DAJPNS.2019.00013 Dusunen Adam The Journal of Psychiatry and Neurological Sciences 2019;32:81-6 EDITORIAL Heightened misuse risk and addictive potential of gabapentinoids: the fate of effective anxiolytics Cuneyt Evren1 , Vahap Karabulut1 1Bakirkoy Training and Research Hospital for Psychiatry Neurology and Neurosurgery, Research, Treatment and Training Center for Alcohol and Substance Dependence (AMATEM), Istanbul - Turkey Gabapentin and pregabalin, two pharmacologically percent of all gabapentin use, accounting for over 90% very closely related substances, are classed as of sales (5). A diagnosis of non-neuropathic pains gabapentinoids (1). Gabapentin was synthesized in accounts for 80.4% of gabapentin and 58.3% of 1977 to create a structural analogue to gamma- pregabalin off-label prescription (6). In Turkey, aminobutyric acid (GABA) with a higher degree of gabapentin has been licensed for the treatment of lipophilia than the original neurotransmitter. In 1993, epilepsy and neuropathic pain, and pregabalin for its use in the treatment of epilepsy began. Pregabalin, epilepsy, neuropathic pain, generalized anxiety another structural analogue of GABA, was synthesized disorder, and fibromyalgia. Drugs containing in 1991; in 2004, it was introduced for the treatment of pregabalin and gabapentin as active ingredients neuropathic pain and in 2005 for the therapy of belonged to the category of controlled drugs distributed refractory epilepsy. A third member of this drug family, with a regular prescription; however, in April 2019 mirogabalin, is currently undergoing clinical trials for pregabalin was included in the category of green- the treatment of diabetic neuropathy, fibromyalgia, and colored (controlled medication) prescription (7). postherpetic neuralgia (2). The mechanism of action of gabapentinoids is not Gabapentinoids are commonly used in neurology, fully understood. -

Draft for Public Comment
Draft for Public Comment Practice guideline update: Treatment of painful diabetic polyneuropathy Report of the Guideline Subcommittee of the American Academy of Neurology Authors (Alphabetical order—final order to be determined later in the guideline development process) Carmel Armon, MD, MSc, MHS1,Vera Bril, MD2, Brian C. Callaghan, MD, MS3, Lindsay Colbert, MA4, William S. David, MD, PhD5, Mary Dolan O’Brien, MLIS6, Kenneth Fink, MD, MPH7, Gary Franklin, MD, MPH8, Gary Gronseth, MD9, John Halperin, MD10, Lawrence B. Harkless, DPM11, Leslie Levine, PhD, VMD, JD12, Nicole Licking, DO13, Bruce A. Perkins, MD, MPH14, Michael Pignone, MD15, Raymond Price, MD16, Alexander Rae-Grant, MD17, Don Smith, MD18, Scott R. Wessels, MPS, ELS6 1. Department of Neurology, Tel Aviv University Sackler School of Medicine, Israel 2. Division of Neurology, Department of Medicine, Toronto General Hospital, ON, Canada 3. Department of Neurology, University of Michigan, Ann Arbor 4. The Foundation for Peripheral Neuropathy, Buffalo Grove, IL 5. Department of Neurology, Massachusetts General Hospital, Boston 6. American Academy of Neurology, Minneapolis, MN 7. Kamehameha Schools, Honolulu, HI 8. Department of Neurology, University of Washington, Seattle, WA 9. Department of Neurology, University of Kansas Medical Center, Kansas City 10. Department of Neurosciences, Overlook Medical Center, Summit, NJ 11. Western University Health Sciences College of Podiatric Medicine, Pomona, CA 1 Draft for Public Comment 12. Neuropathy Action Foundation, Santa Ana, CA 13. New West Physicians, Golden, CO 14. Leadership Sinai Centre for Diabetes, Mount Sinai Hospital, Toronto, ON 15. Department of Medicine, The University of Texas at Austin 16. Department of Neurology, University of Pennsylvania, Philadelphia 17. -

Novi Analgetici-Što Je Trend?
Novi analgetici-što je trend? Knežević, Luciana Master's thesis / Diplomski rad 2019 Degree Grantor / Ustanova koja je dodijelila akademski / stručni stupanj: University of Zagreb, Faculty of Pharmacy and Biochemistry / Sveučilište u Zagrebu, Farmaceutsko- biokemijski fakultet Permanent link / Trajna poveznica: https://urn.nsk.hr/urn:nbn:hr:163:173638 Rights / Prava: In copyright Download date / Datum preuzimanja: 2021-10-01 Repository / Repozitorij: Repository of Faculty of Pharmacy and Biochemistry University of Zagreb Luciana Knežević Novi analgetici - što je trend? DIPLOMSKI RAD Predan Sveučilištu u Zagrebu, Farmaceutsko-biokemijskom fakultetu Zagreb, 2019. Ovaj diplomski rad je prijavljen na kolegiju Farmakologija, Sveučilišta u Zagrebu Farmaceutsko-biokemijskog fakulteta i izrađen na Zavodu za farmakologiju pod stručnim vodstvom doc. dr. sc. Petre Turčić i suvoditeljstvom doc. dr. sc. Jasminke Peršec. Ovim putem bih se zahvalila mentorici doc. dr. sc. Petri Turčić i komentorici doc. dr. sc. Jasminki Peršec na uloženom trudu, strpljenju i pomoći prilikom pisanja diplomskoga rada. Veliko hvala mojoj obitelji koja mi je bila velika podrška i poticaj tijekom studiranja. Također, hvala mome dečku i prijateljima koji su bili uz mene i učinili mi ovaj period života posebnim. SADRŽAJ: 1. UVOD ............................................................................................................................................................ 4 1.1. DEFINICIJA BOLI............................................................................................................................... -
Modulation of NMDA Receptor Activity in Fibromyalgia
biomedicines Review Modulation of NMDA Receptor Activity in Fibromyalgia Geoffrey Littlejohn * and Emma Guymer Departments of Medicine, Monash University and Rheumatology, MonashHealth, Melbourne 3168, Australia; [email protected] * Correspondence: [email protected]; Tel.: +61-03-9594-2575 Academic Editor: Kim Lawson Received: 23 February 2017; Accepted: 7 April 2017; Published: 11 April 2017 Abstract: Activation of the N-methyl-D-aspartate receptor (NMDAR) results in increased sensitivity of spinal cord and brain pathways that process sensory information, particularly those which relate to pain. The NMDAR shows increased activity in fibromyalgia and hence modulation of the NMDAR is a target for therapeutic intervention. A literature review of interventions impacting on the NMDAR shows a number of drugs to be active on the NMDAR mechanism in fibromyalgia patients, with variable clinical effects. Low-dose intravenous ketamine and oral memantine both show clinically useful benefit in fibromyalgia. However, consideration of side-effects, logistics and cost need to be factored into management decisions regarding use of these drugs in this clinical setting. Overall benefits with current NMDAR antagonists appear modest and there is a need for better strategy trials to clarify optimal dose schedules and to delineate potential longer–term adverse events. Further investigation of the role of the NMDAR in fibromyalgia and the effect of other molecules that modulate this receptor appear important to enhance treatment targets in fibromyalgia. Keywords: fibromyalgia; drugs; NMDA receptor; ketamine; memantine 1. Introduction There are multiple pain-related mechanisms that are active in patients with fibromyalgia. The relative contribution of each mechanism appears to vary between patients. -

Stembook 2018.Pdf
The use of stems in the selection of International Nonproprietary Names (INN) for pharmaceutical substances FORMER DOCUMENT NUMBER: WHO/PHARM S/NOM 15 WHO/EMP/RHT/TSN/2018.1 © World Health Organization 2018 Some rights reserved. This work is available under the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 IGO licence (CC BY-NC-SA 3.0 IGO; https://creativecommons.org/licenses/by-nc-sa/3.0/igo). Under the terms of this licence, you may copy, redistribute and adapt the work for non-commercial purposes, provided the work is appropriately cited, as indicated below. In any use of this work, there should be no suggestion that WHO endorses any specific organization, products or services. The use of the WHO logo is not permitted. If you adapt the work, then you must license your work under the same or equivalent Creative Commons licence. If you create a translation of this work, you should add the following disclaimer along with the suggested citation: “This translation was not created by the World Health Organization (WHO). WHO is not responsible for the content or accuracy of this translation. The original English edition shall be the binding and authentic edition”. Any mediation relating to disputes arising under the licence shall be conducted in accordance with the mediation rules of the World Intellectual Property Organization. Suggested citation. The use of stems in the selection of International Nonproprietary Names (INN) for pharmaceutical substances. Geneva: World Health Organization; 2018 (WHO/EMP/RHT/TSN/2018.1). Licence: CC BY-NC-SA 3.0 IGO. Cataloguing-in-Publication (CIP) data.