Version 9.0 October 2017
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Interbiotech Entecavir
InterBioTech FT-XLS250 Entecavir Product Description Catalog #: XLS250, 5mg XLS251, 10mg XLS252, 50mg XLS253, 100mg AXAIV0, 1ml 10mM in DMSO. Catalog #: Name: Entecavir, Monohydrate Syn: BMS200475 monohydrate; SQ34676 monohydrate CAS : 209216-23-9 MW : 295.29 Formula : C12H17N5O4 Properties : DMSO : ≥ 50 mg/mL (169.33 mM) H2O : 2.8 mg/mL (9.48 mM) >99.5% Storage: Powder: -20°C (long term; possible at +4°C (2 years) (M) Also available: In solvent: -80°C (6 months) -20°C (1 month) Entecavir free form #RO893P/Q/R (Syn.: BMS200475; SQ34676) CAS No. : 142217-69-4; MW: 277.2 For Research Use Only Introduction Entecavir monohydrate (BMS200475 monohydrate; SQ34676 monohydrate) is a potent and selective inhibitor of HBV, with an EC50 of 3.75 nM in HepG2 cell. IC50 & Target EC50:3.75 nM (anti-HBV, HepG2 cell)[1] In Vitro *Solubility : DMSO : ≥ 50 mg/mL (169.33 mM) H2O : 2.8 mg/mL (9.48 mM; Need ultrasonic and warming) *Preparation : 1mM = 1mg in 3.3865 mL Entecavir monohydrate (BMS200475 monohydrate; SQ34676 monohydrate) has a EC50 of 3.75 nM against HBV. It is incorporated into the protein primer of HBV and subsequently inhibits the priming step of the reverse transcriptase. The antiviral activity of BMS-200475 is significantly less against the other RNA and DNA viruses[1]. Entecavir monohydrate is more readily phosphorylated to its active metabolites than other deoxyguanosine analogs (penciclovir, ganciclovir, lobucavir, and aciclovir) or lamivudine. The intracellular half-life of entecavir is 15 h[2]. P.1 InterBioTech FT-XLS250 In Vivo *Preparation : 1. Add each solvent one by one: 10% DMSO 40% PEG300 5% Tween-80 45% saline Solubility: ≥ 3 mg/mL (10.16 mM); Clear solution 2. -

COVID-19) Pandemic on National Antimicrobial Consumption in Jordan
antibiotics Article An Assessment of the Impact of Coronavirus Disease (COVID-19) Pandemic on National Antimicrobial Consumption in Jordan Sayer Al-Azzam 1, Nizar Mahmoud Mhaidat 1, Hayaa A. Banat 2, Mohammad Alfaour 2, Dana Samih Ahmad 2, Arno Muller 3, Adi Al-Nuseirat 4 , Elizabeth A. Lattyak 5, Barbara R. Conway 6,7 and Mamoon A. Aldeyab 6,* 1 Clinical Pharmacy Department, Jordan University of Science and Technology, Irbid 22110, Jordan; [email protected] (S.A.-A.); [email protected] (N.M.M.) 2 Jordan Food and Drug Administration (JFDA), Amman 11181, Jordan; [email protected] (H.A.B.); [email protected] (M.A.); [email protected] (D.S.A.) 3 Antimicrobial Resistance Division, World Health Organization, Avenue Appia 20, 1211 Geneva, Switzerland; [email protected] 4 World Health Organization Regional Office for the Eastern Mediterranean, Cairo 11371, Egypt; [email protected] 5 Scientific Computing Associates Corp., River Forest, IL 60305, USA; [email protected] 6 Department of Pharmacy, School of Applied Sciences, University of Huddersfield, Huddersfield HD1 3DH, UK; [email protected] 7 Institute of Skin Integrity and Infection Prevention, University of Huddersfield, Huddersfield HD1 3DH, UK * Correspondence: [email protected] Citation: Al-Azzam, S.; Mhaidat, N.M.; Banat, H.A.; Alfaour, M.; Abstract: Coronavirus disease 2019 (COVID-19) has overlapping clinical characteristics with bacterial Ahmad, D.S.; Muller, A.; Al-Nuseirat, respiratory tract infection, leading to the prescription of potentially unnecessary antibiotics. This A.; Lattyak, E.A.; Conway, B.R.; study aimed at measuring changes and patterns of national antimicrobial use for one year preceding Aldeyab, M.A. -

Analysis of Mutations Leading to Para-Aminosalicylic Acid Resistance in Mycobacterium Tuberculosis
www.nature.com/scientificreports OPEN Analysis of mutations leading to para-aminosalicylic acid resistance in Mycobacterium tuberculosis Received: 9 April 2019 Bharati Pandey1, Sonam Grover2, Jagdeep Kaur1 & Abhinav Grover3 Accepted: 31 July 2019 Thymidylate synthase A (ThyA) is the key enzyme involved in the folate pathway in Mycobacterium Published: xx xx xxxx tuberculosis. Mutation of key residues of ThyA enzyme which are involved in interaction with substrate 2′-deoxyuridine-5′-monophosphate (dUMP), cofactor 5,10-methylenetetrahydrofolate (MTHF), and catalytic site have caused para-aminosalicylic acid (PAS) resistance in TB patients. Focusing on R127L, L143P, C146R, L172P, A182P, and V261G mutations, including wild-type, we performed long molecular dynamics (MD) simulations in explicit solvent to investigate the molecular principles underlying PAS resistance due to missense mutations. We found that these mutations lead to (i) extensive changes in the dUMP and MTHF binding sites, (ii) weak interaction of ThyA enzyme with dUMP and MTHF by inducing conformational changes in the structure, (iii) loss of the hydrogen bond and other atomic interactions and (iv) enhanced movement of protein atoms indicated by principal component analysis (PCA). In this study, MD simulations framework has provided considerable insight into mutation induced conformational changes in the ThyA enzyme of Mycobacterium. Antimicrobial resistance (AMR) threatens the efective treatment of tuberculosis (TB) caused by the bacteria Mycobacterium tuberculosis (Mtb) and has become a serious threat to global public health1. In 2017, there were reports of 5,58000 new TB cases with resistance to rifampicin (frst line drug), of which 82% have developed multidrug-resistant tuberculosis (MDR-TB)2. AMR has been reported to be one of the top health threats globally, so there is an urgent need to proactively address the problem by identifying new drug targets and understanding the drug resistance mechanism3,4. -

Antimicrobial Resistance Benchmark 2020 Antimicrobial Resistance Benchmark 2020
First independent framework for assessing pharmaceutical company action Antimicrobial Resistance Benchmark 2020 Antimicrobial Resistance Benchmark 2020 ACKNOWLEDGEMENTS The Access to Medicine Foundation would like to thank the following people and organisations for their contributions to this report.1 FUNDERS The Antimicrobial Resistance Benchmark research programme is made possible with financial support from UK AID and the Dutch Ministry of Health, Welfare and Sport. Expert Review Committee Research Team Reviewers Hans Hogerzeil - Chair Gabrielle Breugelmans Christine Årdal Gregory Frank Fatema Rafiqi Karen Gallant Nina Grundmann Adrián Alonso Ruiz Hans Hogerzeil Magdalena Kettis Ruth Baron Hitesh Hurkchand Joakim Larsson Dulce Calçada Joakim Larsson Marc Mendelson Moska Hellamand Marc Mendelson Margareth Ndomondo-Sigonda Kevin Outterson Katarina Nedog Sarah Paulin (Observer) Editorial Team Andrew Singer Anna Massey Deirdre Cogan ACCESS TO MEDICINE FOUNDATION Rachel Jones The Access to Medicine Foundation is an independent Emma Ross non-profit organisation based in the Netherlands. It aims to advance access to medicine in low- and middle-income Additional contributors countries by stimulating and guiding the pharmaceutical Thomas Collin-Lefebvre industry to play a greater role in improving access to Alex Kong medicine. Nestor Papanikolaou Address Contact Naritaweg 227-A For more information about this publication, please contact 1043 CB, Amsterdam Jayasree K. Iyer, Executive Director The Netherlands [email protected] +31 (0) 20 215 35 35 www.amrbenchmark.org 1 This acknowledgement is not intended to imply that the individuals and institutions referred to above endorse About the cover: Young woman from the Antimicrobial Resistance Benchmark methodology, Brazil, where 40%-60% of infections are analyses or results. -

Recommended Comparator Products: Medicines for Hepatitis B and C
Guidance Document WHO/PQT: medicines 10 December 2019 Recommended comparator products: Medicines for Hepatitis B and C Comparator products should be purchased from a well regulated market with stringent regulatory authority1. Recommended comparator product Invited medicinal products (Strength, Manufacturer) Hepatitis C Single Ingredient Daclatasvir tablet, 60mg, 30mg Daclatasvir 30 mg and 60 mg tablet, Mylan Laboratories Ltd3 Dasabuvir tablet, 250mg Exviera 250 mg tablet, AbbVie Inc. Viekirax copackaged, 250 mg tablet (+12.5mg/75mg/50mg tablet), AbbVie Inc. Ledipasvir tablet, 90mg No comparator available Ribavirin capsule, 200mg, 400mg, 600 mg Rebetol, 200 mg capsule, MSD Ribavirin syrup, 40mg/ml (oral) Rebetol solution, 40mg/ml, MSD Sofosbuvir tablet 400mg Sovaldi, 400 mg tablet, Gilead Sciences Velpatasvir tablet, 100mg No comparator available Fixed-dose combination (FDC) Ombitasvir/Paritaprevir/Ritonavir, tablet Viekirax, 12.5mg/75mg/50mg tablet, AbbVie Inc. 12.5mg/75mg/50mg, 25mg/150mg/100mg Technivie, 12.5mg/75mg/50mg tablet, AbbVie Inc., US2 Sofosbuvir/ Daclatasvir, tablet 400mg/30mg The individual comparators should be used. Sofosbuvir/ Daclatasvir, tablet 400mg/60mg The individual comparators should be used. 1 A regulatory authority that is: a) a member of ICH prior to 23 October 2015, namely: the US Food and Drug Administration, the European Commission and the Ministry of Health, Labour and Welfare of Japan also represented by the Pharmaceuticals and Medical Devices Agency; or b) an ICH observer prior to 23 October 2015, namely: the European Free Trade Association, as represented by Swissmedic and Health Canada; or c) a regulatory authority associated with an ICH member through a legally-binding, mutual recognition agreement prior to 23 October 2015, namely: Australia, Iceland, Liechtenstein and Norway. -

Updated WHO MDR-TB Treatment Guidelines and the Use of New Drugs in Children
Updated WHO MDR-TB treatment guidelines and the use of new drugs in children Annual meeting of the Childhood TB subgroup Liverpool, UK, 26 October 2016 Dr Malgosia Grzemska WHO/HQ, Global TB Programme Outline • Latest epidemiological data • Existing guidelines • 2016 update of the DR-TB treatment guidelines • New recommendations for treatment of RR-TB and MDR- TB in children • Delamanid guideline for use in children and adolescents • Research gaps • Conclusions The Global Burden of TB - 2015 Estimated number Estimated number of cases of deaths 10,4 million 1.8 million* All forms of TB • 1 million Children (10%) • 210,000 children (170,000 HIV negative and 40,000 HIV- positive) HIV-associated TB 1.2 million (11%) 390,000 Multidrug-resistant TB 480,000 190,000 +100,000 RR cases Childhood TB: MDRTB estimates Dodd P., Sismanidis B., Seddon J., Lancet Inf Dis, 21 June 2016: Global burden of drug-resistant tuberculosis in children: a mathematical modelling study • It is estimated that over 67 million children are infected with TB and therefore at risk of developing disease in the future; – 5 mln with INH resistance; 2 mln with MDR; 100,000 with XDR • Every year 25,000 children develop MDRTB and 1200 XDR TB MDR-TB in children • MDR-TB in children is mainly the result of transmission of a strain of M. tuberculosis that is MDR from an adult source case , and therefore often not suspected unless a history of contact with an adult pulmonary MDR-TB case is known. • Referral to a specialist is advised for treatment. -

Tenofovir Alafenamide Rescues Renal Tubules in Patients with Chronic Hepatitis B
life Communication Tenofovir Alafenamide Rescues Renal Tubules in Patients with Chronic Hepatitis B Tomoya Sano * , Takumi Kawaguchi , Tatsuya Ide, Keisuke Amano, Reiichiro Kuwahara, Teruko Arinaga-Hino and Takuji Torimura Division of Gastroenterology, Department of Medicine, Kurume University School of Medicine, Kurume, Fukuoka 830-0011, Japan; [email protected] (T.K.); [email protected] (T.I.); [email protected] (K.A.); [email protected] (R.K.); [email protected] (T.A.-H.); [email protected] (T.T.) * Correspondence: [email protected]; Tel.: +81-942-31-7627 Abstract: Nucles(t)ide analogs (NAs) are effective for chronic hepatitis B (CHB). NAs suppress hepatic decompensation and hepatocarcinogenesis, leading to a dramatic improvement of the natural course of patients with CHB. However, renal dysfunction is becoming an important issue for the management of CHB. Renal dysfunction develops in patients with the long-term treatment of NAs including adefovir dipivoxil and tenofovir disoproxil fumarate. Recently, several studies have reported that the newly approved tenofovir alafenamide (TAF) has a safe profile for the kidney due to greater plasma stability. In this mini-review, we discuss the effectiveness of switching to TAF for NAs-related renal tubular dysfunction in patients with CHB. Keywords: adefovir dipivoxil (ADV); Fanconi syndrome; hepatitis B virus (HBV); renal tubular Citation: Sano, T.; Kawaguchi, T.; dysfunction; tenofovir alafenamide (TAF); tenofovir disoproxil fumarate (TDF); β2-microglobulin Ide, T.; Amano, K.; Kuwahara, R.; Arinaga-Hino, T.; Torimura, T. Tenofovir Alafenamide Rescues Renal Tubules in Patients with Chronic 1. -

Rash with Entecavir - Case Report Xiong Khee Cheong1, Zhiqin Wong2*, Norazirah Md Nor3 and Bang Rom Lee4
Cheong et al. BMC Gastroenterology (2020) 20:305 https://doi.org/10.1186/s12876-020-01452-3 CASE REPORT Open Access “Black box warning” rash with entecavir - case report Xiong Khee Cheong1, Zhiqin Wong2*, Norazirah Md Nor3 and Bang Rom Lee4 Abstract Background: Hepatitis B infection is a significant worldwide health issue, predispose to the development of liver cirrhosis and hepatocellular carcinoma. Entecavir is a potent oral antiviral agent of high genetic barrier for the treatment of chronic hepatitis B infection. Cutaneous adverse reaction associated with entecavir has rarely been reported in literature. As our knowledge, this case was the first case reported on entecavir induced lichenoid drug eruption. Case presentation: 55 year old gentlemen presented with generalised pruritic erythematous rash on trunk and extremities. Six weeks prior to his consultation, antiviral agent entecavir was commenced for his chronic hepatitis B infection. Skin biopsy revealed acanthosis and focal lymphocytes with moderate perivascular lymphocyte infiltration. Skin condition recovered completely after caesation of offending drug and short course of oral corticosteroids. Conclusion: This case highlight the awareness of clinicians on the spectrum of cutaneous drug reaction related to entecavir therapy. Keywords: Drug eruption, Entecavir, Hepatitis B Background Case presentation Hepatitis B infection is a global health issue, contribut- A 55 years old gentlemen, background of chronic ing to approximately 887,000 deaths in 2015 due to he- hepatitis B (treatment naïve), was referred for 2 patocellular carcinoma and liver cirrhosis [1, 2]. weeks of generalised itchy erythematous rash. His Entecavir is a nucleoside analogue reverse transcriptase other medical illnesses were ischemic heart disease, inhibitor that is widely used in the treatment of chronic chronic kidney disease stage 3, diabetes mellitus and hepatitis B (HBV) infection. -

Information for the User Valganciclovir <Invented Name>
Package Leaflet: Information for the user Valganciclovir <Invented Name> 450 mg film-coated tablets Valganciclovir Read all of this leaflet carefully before you start taking this medicine because it contains important information for you. Keep this leaflet. You may need to read it again. If you have any further questions, ask your doctor or pharmacist. This medicine has been prescribed for you only. Do not pass it on to others. It may harm them, even if their signs of illness are the same as yours. If you get any side effects, talk to your doctor or pharmacist. This includes any possible side effects not listed in this leaflet. See section 4. What is in this leaflet: 1. What Valganciclovir <Invented Name> is and what it is used for 2. What you need to know before you take Valganciclovir <Invented Name> 3. How to take Valganciclovir <Invented Name> 4. Possible side effects 5. How to store Valganciclovir <Invented Name> 6. Contents of the pack and other information 1. What Valganciclovir <Invented Name> is and what it is used for Valganciclovir <Invented Name> belongs to a group of medicines, which work directly to prevent the growth of viruses. In the body the active ingredient in the tablets, valganciclovir, is changed into ganciclovir. Ganciclovir prevents a virus called cytomegalovirus (CMV) from multiplying and invading healthy cells. In patients with a weakened immune system, CMV can cause an infection in the body’s organs. This can be life threatening. Valganciclovir <Invented Name> is used: for treatment of CMV-infections of the retina of the eye in patients with acquired immunodeficiency syndrome (AIDS). -
![Ehealth DSI [Ehdsi V2.2.2-OR] Ehealth DSI – Master Value Set](https://docslib.b-cdn.net/cover/8870/ehealth-dsi-ehdsi-v2-2-2-or-ehealth-dsi-master-value-set-1028870.webp)
Ehealth DSI [Ehdsi V2.2.2-OR] Ehealth DSI – Master Value Set
MTC eHealth DSI [eHDSI v2.2.2-OR] eHealth DSI – Master Value Set Catalogue Responsible : eHDSI Solution Provider PublishDate : Wed Nov 08 16:16:10 CET 2017 © eHealth DSI eHDSI Solution Provider v2.2.2-OR Wed Nov 08 16:16:10 CET 2017 Page 1 of 490 MTC Table of Contents epSOSActiveIngredient 4 epSOSAdministrativeGender 148 epSOSAdverseEventType 149 epSOSAllergenNoDrugs 150 epSOSBloodGroup 155 epSOSBloodPressure 156 epSOSCodeNoMedication 157 epSOSCodeProb 158 epSOSConfidentiality 159 epSOSCountry 160 epSOSDisplayLabel 167 epSOSDocumentCode 170 epSOSDoseForm 171 epSOSHealthcareProfessionalRoles 184 epSOSIllnessesandDisorders 186 epSOSLanguage 448 epSOSMedicalDevices 458 epSOSNullFavor 461 epSOSPackage 462 © eHealth DSI eHDSI Solution Provider v2.2.2-OR Wed Nov 08 16:16:10 CET 2017 Page 2 of 490 MTC epSOSPersonalRelationship 464 epSOSPregnancyInformation 466 epSOSProcedures 467 epSOSReactionAllergy 470 epSOSResolutionOutcome 472 epSOSRoleClass 473 epSOSRouteofAdministration 474 epSOSSections 477 epSOSSeverity 478 epSOSSocialHistory 479 epSOSStatusCode 480 epSOSSubstitutionCode 481 epSOSTelecomAddress 482 epSOSTimingEvent 483 epSOSUnits 484 epSOSUnknownInformation 487 epSOSVaccine 488 © eHealth DSI eHDSI Solution Provider v2.2.2-OR Wed Nov 08 16:16:10 CET 2017 Page 3 of 490 MTC epSOSActiveIngredient epSOSActiveIngredient Value Set ID 1.3.6.1.4.1.12559.11.10.1.3.1.42.24 TRANSLATIONS Code System ID Code System Version Concept Code Description (FSN) 2.16.840.1.113883.6.73 2017-01 A ALIMENTARY TRACT AND METABOLISM 2.16.840.1.113883.6.73 2017-01 -
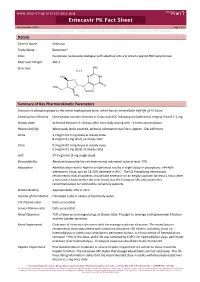
Entecavir PK Fact Sheet Reviewed March 2016 Page 1 of 2 for Personal Use Only
www.hep-druginteractions.org Entecavir PK Fact Sheet Reviewed March 2016 Page 1 of 2 For personal use only. Not for distribution. For personal use only. Not for distribution. For personal use only. Not for distribution. Details Generic Name Entecavir Trade Name Baraclude® Class Guanosine nucleoside analogue with selective antiviral activity against HBV polymerase Molecular Weight 295.3 Structure NH2 H2O HO NNH O HO N N CH2 Summary of Key Pharmacokinetic Parameters Entecavir is phosphorylated to the active triphosphate form, which has an intracellular half‐life of 15 hours. Linearity/non‐linearity Dose‐proportionate increases in Cmax and AUC following multiple doses ranging from 0.1‐1 mg. Steady state Achieved between 6‐10 days after once daily dosing with ~2 times accumulation. Plasma half life When peak levels reached, terminal elimination half life is approx. 128‐149 hours. Cmax 4.2 ng/ml (0.5 mg dose) at steady state 8.2 ng/ml (1 mg dose) at steady state Cmin 0.3 ng/ml (0.5 mg dose) at steady state 0.5 ng/ml (1 mg dose) at steady state AUC 27.9 ng.h/ml (1 mg single dose) Bioavailability Absolute bioavailability not determined; estimated to be at least 70%. Absorption Administration with a high fat or light meal results in slight delay in absorption; a 44‐46% decrease in Cmax, and an 18‐20% decrease in AUC. The US Prescribing Information recommends that all patients should take entecavir on an empty stomach (at least 2 hours after a meal and 2 hours before the next meal), but the European SPC only makes this recommendation for lamivudine‐refractory patients. -

Six-Month Response to Delamanid Treatment in MDR TB Patients
RESEARCH LETTERS antimicrobial drug prophylaxis is not known (5), and 7. Public Health Agency of Canada. Guidelines for the prevention and guidelines vary among countries. In the United Kingdom, control of invasive group A streptococcal disease. October 2006 [cited 2017 April 4th]. https://eportal.mountsinai.ca/Microbiology/ prophylaxis is recommended for exposed mothers or babies protocols/pdf/GAS%20guidelines%202006.pdf during the neonatal period, for symptomatic close contacts, 8. Direction générale de la Santé. Notification from the French High or for the entire household if there is >1 case (6). In Cana- Council for Public Hygiene (Communicable Diseases section) da, prophylaxis is recommended for persons who had close concerning conduct to be taken in cases of one or more invasive group A streptococcal disease of community origin. Session of contact with a person with a confirmed severe case dur- November 18th, 2005 [in French] [cited 2016 Dec 26]. ing a specified period (7); in France and the United States, http://www.hcsp.fr/docspdf/cshpf/a_mt_181105_streptococcus.pdf prophylaxis is recommended for close contacts with risk 9. Prevention of Invasive Group A Streptococcal Infections factors for invasive infections (8,9). In the cases we report Workshop Participants. Prevention of invasive group A streptococcal disease among household contacts of case patients here, the second case-patient did not receive prophylaxis and among postpartum and postsurgical patients: recommendations because of the short period between the 2 cases. from the Centers for Disease Control and Prevention. Clin Infect Both case-patients received NSAIDs during the onset Dis. 2002;35:950–9. Erratum in: Clin Infect Dis.