Open Access Article Under the CC by License (
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
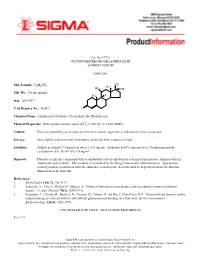
Fluoxymesterone-Dea Schedule Iii Androfluorene
Cat. No. F7751 FLUOXYMESTERONE--DEA SCHEDULE III ANDROFLUORENE Androgen. OH Mol. Formula: C20H29FO3 HO H3C CH3 Mol. Wt.: 336.45 (anhyd.) F H3C m.p.: 288-290°C CAS Registry No.: 76-43-7 O Chemical Name: 4-Androsten-9a-fluoro-17a-methyl-11b,17b-diol-3-one 22 Physical Properties: White photosensitive solid. [a] D = +102.34° (c = 0.47, EtOH). Caution: Due care should be exercised to prevent skin contact, ingestion or inhalation of this compound. Storage: Store tightly sealed at room temperature, protected from exposure to light. Solubility: Soluble in ethanol (7.3 mg/ml) or water (< 0.5 mg/ml). Solubility in 45% aqueous (w/v) 2-hydroxypropyl-b- cyclodextrin (Cat. No. H-107): 6.4 mg/ml. Disposal: Dissolve or mix the compound with a combustible solvent and burn in a chemical incinerator equipped with an afterburner and scrubber. This product is controlled by the Drug Enforcement Administration. Appropriate security must be maintained until the substance is destroyed. Records must be kept which detail the ultimate disposition of the material. References: 1. Merck Index 11th Ed., No. 4113. 2. Saborido, A., Vila, J., Molano, F., Megias, A. “Effect of steroids on mitochondria and sarcotubular system of skeletal muscle.” J. Appl. Physiol. 70(3), 1038 (1991). 3. Fernandez, L., Chirino, R., Boada, L.D., Navarro, D., Cabrera, N., del Rio, I., Diaz-Chico, B.N. “Stanozolol and danazol, unlike natural androgens, interact with the low affinity glucocorticoid-binding sites from male rat liver microsomes.” Endocrinology 134(3), 1401 (1994). CONTROLLED SUBSTANCE - DEA LICENSE REQUIRED (III) Rev. -

)&F1y3x PHARMACEUTICAL APPENDIX to THE
)&f1y3X PHARMACEUTICAL APPENDIX TO THE HARMONIZED TARIFF SCHEDULE )&f1y3X PHARMACEUTICAL APPENDIX TO THE TARIFF SCHEDULE 3 Table 1. This table enumerates products described by International Non-proprietary Names (INN) which shall be entered free of duty under general note 13 to the tariff schedule. The Chemical Abstracts Service (CAS) registry numbers also set forth in this table are included to assist in the identification of the products concerned. For purposes of the tariff schedule, any references to a product enumerated in this table includes such product by whatever name known. Product CAS No. Product CAS No. ABAMECTIN 65195-55-3 ACTODIGIN 36983-69-4 ABANOQUIL 90402-40-7 ADAFENOXATE 82168-26-1 ABCIXIMAB 143653-53-6 ADAMEXINE 54785-02-3 ABECARNIL 111841-85-1 ADAPALENE 106685-40-9 ABITESARTAN 137882-98-5 ADAPROLOL 101479-70-3 ABLUKAST 96566-25-5 ADATANSERIN 127266-56-2 ABUNIDAZOLE 91017-58-2 ADEFOVIR 106941-25-7 ACADESINE 2627-69-2 ADELMIDROL 1675-66-7 ACAMPROSATE 77337-76-9 ADEMETIONINE 17176-17-9 ACAPRAZINE 55485-20-6 ADENOSINE PHOSPHATE 61-19-8 ACARBOSE 56180-94-0 ADIBENDAN 100510-33-6 ACEBROCHOL 514-50-1 ADICILLIN 525-94-0 ACEBURIC ACID 26976-72-7 ADIMOLOL 78459-19-5 ACEBUTOLOL 37517-30-9 ADINAZOLAM 37115-32-5 ACECAINIDE 32795-44-1 ADIPHENINE 64-95-9 ACECARBROMAL 77-66-7 ADIPIODONE 606-17-7 ACECLIDINE 827-61-2 ADITEREN 56066-19-4 ACECLOFENAC 89796-99-6 ADITOPRIM 56066-63-8 ACEDAPSONE 77-46-3 ADOSOPINE 88124-26-9 ACEDIASULFONE SODIUM 127-60-6 ADOZELESIN 110314-48-2 ACEDOBEN 556-08-1 ADRAFINIL 63547-13-7 ACEFLURANOL 80595-73-9 ADRENALONE -

Determination of 17 Hormone Residues in Milk by Ultra-High-Performance Liquid Chromatography and Triple Quadrupole Mass Spectrom
No. LCMSMS-065E Liquid Chromatography Mass Spectrometry Determination of 17 Hormone Residues in Milk by Ultra-High-Performance Liquid Chromatography and Triple Quadrupole No. LCMSMS-65E Mass Spectrometry This application news presents a method for the determination of 17 hormone residues in milk using Shimadzu Ultra-High-Performance Liquid Chromatograph (UHPLC) LC-30A and Triple Quadrupole Mass Spectrometer LCMS- 8040. After sample pretreatment, the compounds in the milk matrix were separated using UPLC LC-30A and analyzed via Triple Quadrupole Mass Spectrometer LCMS-8040. All 17 hormones displayed good linearity within their respective concentration range, with correlation coefficient in the range of 0.9974 and 0.9999. The RSD% of retention time and peak area of 17 hormones at the low-, mid- and high- concentrations were in the range of 0.0102-0.161% and 0.563-6.55% respectively, indicating good instrument precision. Method validation was conducted and the matrix spike recovery of milk ranged between 61.00-110.9%. The limit of quantitation was 0.14-0.975 g/kg, and it meets the requirement for detection of hormones in milk. Keywords: Hormones; Milk; Solid phase extraction; Ultra performance liquid chromatograph; Triple quadrupole mass spectrometry ■ Introduction Since 2008’s melamine-tainted milk scandal, the With reference to China’s national standard GB/T adulteration of milk powder has become a major 21981-2008 "Hormone Multi-Residue Detection food safety concern. In recent years, another case of Method for Animal-derived Food - LC-MS Method", dairy product safety is suspected to cause "infant a method utilizing solid phase extraction, ultra- sexual precocity" (also known as precocious puberty) performance liquid chromatography and triple and has become another major issue challenging the quadrupole mass spectrometry was developed for dairy industry in China. -

INTEGRIS Formulary July 2017
INTEGRIS Formulary July 2017 Foreword FORMULARY EXCLUDED THERAPEUTIC DRUG This document represents the efforts of the MedImpact Healthcare Systems THERAPEUTIC DRUGS CLASS Pharmacy and Therapeutics (P & T) and Formulary Committees to provide ALTERNATIVES physicians and pharmacists with a method to evaluate the safety, efficacy and cost- clindamycin/tretinoin, ACNE AGENTS, effectiveness of commercially available drug products. A structured approach to the VELTIN drug selection process is essential in ensuring continuing patient access to rational ZIANA TOPICAL drug therapies. The ultimate goal of the MedPerform Formulary is to provide a morphine sulfate ER process and framework to support the dynamic evolution of this document to guide tablets, oxycodone ANALGESICS, KADIAN prescribing decisions that reflect the most current clinical consensus associated ER, NUCYNTA, NARCOTICS with drug therapy decisions. NUCYNTA ER ANALGESICS, This is accomplished through the auspices of the MedImpact P & T and Formulary BELBUCA BUTRANS PATCH Committees. These committees meet quarterly and more often as warranted to NARCOTICS ensure clinical relevancy of the Formulary. To accommodate changes to this ABSTRAL, document, updates are made accessible as necessary. FENTORA, fentanyl citrate ANALGESICS, LAZANDA, lozenge NARCOTICS As you use this Formulary, you are encouraged to review the information and ONSOLIS, provide your input and comments to the MedImpact P & T and Formulary SUBSYS Committees. immediate-release GRALISE ANTICONVULSANTS The MedImpact P & T -

Anabolic Steroids/Androgens Pa Summary
ANABOLIC STEROIDS/ANDROGENS PA SUMMARY PREFERRED Anadrol-50, Danazol, Fluoxymesterone, Methitest, Oxandrolone, Testosterone Cypionate Injection, Testosterone Enanthate Injection NON-PREFERRED Android, Testred LENGTH OF AUTHORIZATION: Varies NOTE: All preferred and non-preferred agents require prior authorization. See PA criteria labeled “Topical Testosterone” for Androderm, Androgel, Striant, and Testim. The criteria details below are for the outpatient pharmacy program. If an injectable medication is being administered in a physician’s office then the criteria information below does not apply. Instead, the physician’s office must bill this drug through the DCH physician’s injectable program and not the outpatient pharmacy program. Information regarding the physician’s injectable program can be located at www.mmis.georgia.gov. PA CRITERIA: For Anadrol-50 Approvable for the following diagnoses: anemia caused by deficient red blood cell production, acquired or congenital aplastic anemia, myelofibrosis, hypoplastic anemia due to administration of myelotoxic drugs Also approvable for HIV or AIDS wasting when significant weight loss is documented in members currently receiving nutritional support For Danazol Approvable for the following diagnoses: endometriosis, fibrocystic breast disease, hereditary angioedema For Fluoxymesterone, Methyltestosterone (Android, Methitest, Testred), Testosterone Cypionate or Enanthate Injection Approvable in male members 12 years of age or older for the following diagnoses: primary hypogonadism, secondary -

Printed Formulary Catalog Basic
Scripps Health Formulary July 2016 Foreword Pharmacy and Therapeutics Committee. MedImpact approves such multi- This document represents the efforts of the MedImpact Healthcare Systems source drugs for addition to the MAC list based on the following criteria: Pharmacy and Therapeutics (P & T) and Formulary Committees to provide physicians A multi-source drug product manufactured by at least one (1) nationally and pharmacists with a method to evaluate the safety, efficacy and cost-effectiveness marketed company. of commercially available drug products. A structured approach to the drug selection At least one (1) of the generic manufacturer’s products must have an “A” process is essential in ensuring continuing patient access to rational drug therapies. rating or the generic product has been determined to be unassociated with The ultimate goal of the Portfolio Formulary is to provide a process and framework to efficacy, safety or bioequivalency concerns by the MedImpact P & T support the dynamic evolution of this document to guide prescribing decisions that Committee. reflect the most current clinical consensus associated with drug therapy decisions. Drug product will be approved for generic substitution by the MedImpact P & T Committee. This is accomplished through the auspices of the MedImpact P & T and Formulary Committees. These committees meet quarterly and more often as warranted to ensure This list is reviewed and updated periodically based on the clinical literature and clinical relevancy of the Formulary. To accommodate changes to this document, pharmacokinetic characteristics of currently available versions of these drug updates are made accessible as necessary. products. As you use this Formulary, you are encouraged to review the information and provide If a member or physician requests a brand name product in lieu of an approved your input and comments to the MedImpact P & T and Formulary Committees. -

Role of Androgens on MCF-7 Breast Cancer Cell Growth and on the Inhibitory Effect of Letrozole
Research Article Role of Androgens on MCF-7 Breast Cancer Cell Growth and on the Inhibitory Effect of Letrozole Luciana F. Macedo, Zhiyong Guo, Syreeta L. Tilghman, Gauri J. Sabnis, Yun Qiu, and Angela Brodie Department of Pharmacology and Experimental Therapeutics, University of Maryland, Baltimore, Maryland Abstract hormone therapy and longer patient survival (14). However, the Previous work has shown that androgens inhibit breast cancer physiologic role of endogenous androgens and events following AR cells and tumor growth. On the other hand, androgens can be activation leading to inhibition of cell growth are not clearly identified in breast cancer cells. Some studies have shown that converted to mitogenic estrogens by aromatase in breast cancer cells. Here, we report that androgens, such as the androgens modulate the expression of the Bcl-2protein family in aromatizable androstenedione and the non-aromatizable breast cancer cells, and that their effect is contrary to that of 5A-dihydrotestosterone, inhibit MCF-7 cell proliferation. This estrogens (15, 16). The Bcl-2family proteins both inhibit and effect is observed only in the absence or at a low concentra- promote cell death (16, 17), and the Bcl-2protein has been tion of estrogens and is evident in cells with low aromatase extensively characterized as an inhibitor of apoptosis. activity. Growth of a new aromatase stably transfected MCF-7 Due to their adverse side effects, exogenous androgens were later cell line (Ac1) was stimulated by conversion of androstene- replaced by other better tolerated breast cancer treatment dione into estrogens and was sensitive to aromatase inhib- strategies, such as ER antagonism and aromatase inhibition. -

A Comparison of Clinical Efficacy Between a Basic Shampoo With
Original Article A Comparison of Clinical Efficacy between a Basic Shampoo with Herbal Extracts Containing Climbazole and Its Similar Sample Containing Piroctone Olamine in the Treatment of Dandruff and Seborrheic Dermatitis Hosein Rastegar, PhD1 Abstract Hamidreza Ahmadi Ashtiani, PhD Background: Dandruff especially with itching and inflammation is a Student2 common complaint among patients in the clinic and its treatment is Mohammad Baghaei, Pharm D3 much challenging. Chemical anti fungal substances used in Saeid Bokaei, PhD4 antidandruff shampoos are common treatments. The aim of this study 5 was to compare the clinical efficacy of two of these anti dandruff Amirhoushang Ehsani, MD substances, climbazole and piroctone olamine in the treatment of Pedram Noormohammadpour, MD5 dandruff and seborrheic dermatitis in shampoos with herbal extracts. 5 Sahar Azizahari, MD Methods: One hundred and twenty men with scalp dandruff of the Ramin Khanmohammad6 same severity, between 20-30 years old and in the same occupational condition in terms of sun exposure or environmental 1. Laboratory Research Centre of Food and pollution were selected and divided randomly into two 60-subject Drug, Ministry of Health and Medical groups. After each shampoo was applied 3 times a week for 5 Educations, Islamic Republic of Iran weeks one in group 1 and the other in group 2, patients were 2. Department of Clinical Biochemistry, assessed for existence of itching and redness of scalp and reduction School of Medical Science, Tarbiat-e- in dandruff and results were compared between two groups. Modarres University, Tehran, Iran and Biochemistry & Nutrition Department of Results: Itching and redness were completely cured in both groups Zanjan Medical University and Institute of after treatment. -

Results of Monitoring and Guidance Based on the Imported Foods Monitoring and Guidance Plan for FY2007
Contact Office of Imported Food Safety, Inspection and Safety Division, Department of Food Safety, Pharmaceutical and Food Safety Bureau, Ministry of Health, Labour and Welfare (extension: 2474, 2497, 2498) Results of Monitoring and Guidance Based on the Imported Foods Monitoring and Guidance Plan for FY2007 August 2008 Department of Food Safety Pharmaceutical and Food Safety Bureau Ministry of Health, Labour and Welfare Results of Monitoring and Guidance Based on the Imported Foods Monitoring and Guidance Plan for FY2007 Introduction The total number of foods, additives, equipment, containers and packages, and toys (hereinafter collectively referred to as “foods”) imported to Japan in FY2007 was about 1.80 million, with an imported weight of about 32.3 million tons. According to the Food Balance Sheet for FY 2007 by the Ministry of Agriculture, Forestry and Fisheries, the food self-sufficiency ratio in Japan (food self-sufficiency ratio based on the total caloric value supplied) was estimated at 40%, indicating that, on a calorie basis, approximately 60% of foods consumed in Japan are imported. Regarding the monitoring and guidance conducted by the national government for the purpose of ensuring the safety of foods imported to Japan (hereinafter referred to as “imported foods”), the Imported Foods Monitoring and Guidance Plan for FY2007 (hereinafter referred to as the “Plan”) was developed based on public comments and risk communications, and was conduced in line with the Guidelines for the Implementation of Monitoring and Guidance on Food Sanitation (Notification No. 301 of the Ministry of Labour, Health and Welfare, 2003) under Article 23, paragraph 1 of the Food Sanitation Law (Law No. -

The Combined Cardiac Effect of the Anabolic Steroid, Nandrolone And
ù1. v -¿. rlc) 77.- *n*hi.rnool oowol,ù*o ffi"/fu -lo *rn*(o fii'o fio¿o¿¿, /v&"ùún lonno **al cooaiæe';¿vfl"- oã. Benjamin D. Phillis, B.Sc. (Hons) Phatmacology Depattment of Clinical & Experimental Pharmacology Ftome Rd. , Medical School Noth Adelaide Univetsity ADEIAIDE SA 5OOO û.)r.'-*hr/7enveltîù Foremost, I would like to thank my two supervisors for the direction that they have given this ptojecr. To Rod, for his unfailing troubleshooting abiJity and to Jenny fot her advice and ability to add scientific rigour' Many thanks to Michael Adams for his technical assistance and especially fot performing the surgery for the ischaemia-reperfusion projects and for his willingness to work late nights and public holidays. Lastly I would like to thank my v¡ife for her extreme patience during the tumult of the last 5 years. Her love, suppoït, patience and undetstanding have been invaluable in this endeavout. Beniamin D. Phillis Octobet,2005 ADE,I-AIDE ii T*(¿t of Ao,t",tù DECI.ARATION I ACKNOWLEDGEMENTS il TABLE OF CONTENTS UI ABBREVIATIONS x ABSTRACT )ilr CÉIAPTER t-l Inttoduction 1-1 1.1 Background 1,-1, 1.2What ate anabolic stetoids? 7-1 1,3 General pharmacology of Anabolic steroids t-2 '1,-2 1.3.1 Genomic effects of anabolic steroids 1.3.2 Non-genomic effects of anabolic steroids 1-3 1.4 Clinical use of AS 1.-4 1.5 Patterns of AS abuse 1.-4 1.5.1 Steroid abuse by athletes 1.-+ 1.5.2 Stetoid abuse by sedentary teenagers r-6 1.5.3 Prevalence of abuse 1-6 1.5.4 Abuse ptevalence in Australia 1.-9 1.6 Cardiotoxicity of anabolic steroids r-9 1.6.1 Reduced cotonary flow 1.-1.1, 1,.6.2 Dtect myocatdial eff ects 1-1 5 1.6.3 Hypertension 1-21 1.7 Difficulties associated with anabolic steroid research 1.-24 1-25 1.8 The polydrug abuse Phenomenon 1.9 The pharmacology of cocaine 1-26 1.10 Pteparations 1-28 1-29 1.11 Metabolism lll 1-30 1. -

Development and Validation of UV Spectroscopic Method for Estimation of Climbazole in Climbazole Shampoo
RESEARCH ARTICLE Am. J. PharmTech Res. 2020; 10(01) ISSN: 2249-3387 Journal home page: http://www.ajptr.com/ Development and Validation of UV Spectroscopic Method for Estimation of Climbazole in Climbazole Shampoo Rajashree N. Patil*1, Pratiksha A. Patil1, Swapnil R. Patil2, Amol Sawale2 1.Department of Pharmaceutical Chemistry, Arunamai College of Pharmacy, Mamurabad, North Maharashtra University, Jalgaon (MH) INDIA 425002. 2.Department of Pharmaceutics and Quality Assurance, Vidya Bharati College of Pharmacy, Amravati University, Amravati (MH) INDIA 444602. ABSTRACT To develop and validate simple, rapid, linear, accurate, precise and economical UV Spectroscopic method for estimation of Climbazole in Climbazole shampoo. The drug is freely soluble in organic solvents such as Chloroform and Methanol. The drug was identified in terms of solubility studies and on the basis of melting point done on Melting Point Apparatus of Equiptronics. It showed absorption maxima were determined in Methanol: Water (50:50). The drug obeyed the Beer’s law and showed good correlation of concentration with absorption which reflect in linearity. The UV spectroscopic method was developed for estimation of Climbazole in shampoo dosage form and also validated as per ICH guidelines. The drug is freely soluble in organic solvents such as Methanol, Chloroform. So, the Analytical Grade Methanol: Water is used as a diluent in equal proportion for method. The melting point of Climbazole was found to be 93-94˚C (uncorrected). It showed absorption maxima 256 nm in Methanol: Water (50:50). On the basis of absorption spectrum the working concentration was set on 6µg/ml (PPM). The linearity was observed between 2-10 μg/ml (PPM). -

(12) United States Patent (10) Patent No.: US 8,911,795 B2 Schmaus Et Al
US00891. 1795B2 (12) United States Patent (10) Patent No.: US 8,911,795 B2 Schmaus et al. (45) Date of Patent: *Dec. 16, 2014 (54) COMPOSITIONS COMPRISING (52) U.S. Cl. DHYDROAVENANTHRAMIDED AND CPC ............. A61O5/006 (2013.01); A61 K 2800/75 CLIMBAZOLEAS COSMETIC AND (2013.01); A61 K31/196 (2013.01); A61 K PHARMACEUTICAL COMPOSITIONS FOR 8/445 (2013.01); A61O 19/00 (2013.01) ALLEVIATING ITCHING USPC ............ 424/640; 514/188: 514/345; 514/563 (58) Field of Classification Search (75) Inventors: Gerhard Schmaus, Höxter (DE); None Joachim Röding, Badenweiler (DE) See application file for complete search history. (73) Assignee: Symrise AG, Holzminden (DE) (56) References Cited U.S. PATENT DOCUMENTS (*) Notice: Subject to any disclaimer, the term of this patent is extended or adjusted under 35 4,070,484 A 1/1978 Harita et al. 8,409,552 B2 * 4/2013 Schmaus et al. ................ 424,61 U.S.C. 154(b) by 1390 days. 2003/0161802 A1* 8, 2003 Flammer et al. ............. 424.70.1 This patent is Subject to a terminal dis 2003/0228272 Al 12/2003 Amjad et al. claimer. 2006/0089413 A1* 4/2006 Schmaus et al. .............. 514,563 (21) Appl. No.: 12/095,453 FOREIGN PATENT DOCUMENTS JP 2005187398 7/2005 (22) PCT Filed: Nov. 3, 2006 WO WO-2004O35O15 4/2004 WO WO 2004/047833 * 6, 2004 ........... A61K 31,196 (86). PCT No.: PCT/EP2006/068077 WO WO-2004O47833 6, 2004 WO WO-2006134013 12/2006 S371 (c)(1), WO WO-2006134120 12/2006 (2), (4) Date: Apr. 23, 2009 OTHER PUBLICATIONS (87) PCT Pub.