Downloaded from Bioscientifica.Com at 09/25/2021 05:16:42PM Via Free Access
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Fluoxymesterone-Dea Schedule Iii Androfluorene
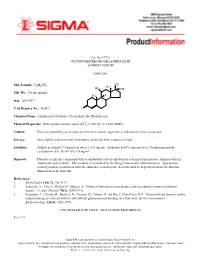
Cat. No. F7751 FLUOXYMESTERONE--DEA SCHEDULE III ANDROFLUORENE Androgen. OH Mol. Formula: C20H29FO3 HO H3C CH3 Mol. Wt.: 336.45 (anhyd.) F H3C m.p.: 288-290°C CAS Registry No.: 76-43-7 O Chemical Name: 4-Androsten-9a-fluoro-17a-methyl-11b,17b-diol-3-one 22 Physical Properties: White photosensitive solid. [a] D = +102.34° (c = 0.47, EtOH). Caution: Due care should be exercised to prevent skin contact, ingestion or inhalation of this compound. Storage: Store tightly sealed at room temperature, protected from exposure to light. Solubility: Soluble in ethanol (7.3 mg/ml) or water (< 0.5 mg/ml). Solubility in 45% aqueous (w/v) 2-hydroxypropyl-b- cyclodextrin (Cat. No. H-107): 6.4 mg/ml. Disposal: Dissolve or mix the compound with a combustible solvent and burn in a chemical incinerator equipped with an afterburner and scrubber. This product is controlled by the Drug Enforcement Administration. Appropriate security must be maintained until the substance is destroyed. Records must be kept which detail the ultimate disposition of the material. References: 1. Merck Index 11th Ed., No. 4113. 2. Saborido, A., Vila, J., Molano, F., Megias, A. “Effect of steroids on mitochondria and sarcotubular system of skeletal muscle.” J. Appl. Physiol. 70(3), 1038 (1991). 3. Fernandez, L., Chirino, R., Boada, L.D., Navarro, D., Cabrera, N., del Rio, I., Diaz-Chico, B.N. “Stanozolol and danazol, unlike natural androgens, interact with the low affinity glucocorticoid-binding sites from male rat liver microsomes.” Endocrinology 134(3), 1401 (1994). CONTROLLED SUBSTANCE - DEA LICENSE REQUIRED (III) Rev. -

)&F1y3x PHARMACEUTICAL APPENDIX to THE
)&f1y3X PHARMACEUTICAL APPENDIX TO THE HARMONIZED TARIFF SCHEDULE )&f1y3X PHARMACEUTICAL APPENDIX TO THE TARIFF SCHEDULE 3 Table 1. This table enumerates products described by International Non-proprietary Names (INN) which shall be entered free of duty under general note 13 to the tariff schedule. The Chemical Abstracts Service (CAS) registry numbers also set forth in this table are included to assist in the identification of the products concerned. For purposes of the tariff schedule, any references to a product enumerated in this table includes such product by whatever name known. Product CAS No. Product CAS No. ABAMECTIN 65195-55-3 ACTODIGIN 36983-69-4 ABANOQUIL 90402-40-7 ADAFENOXATE 82168-26-1 ABCIXIMAB 143653-53-6 ADAMEXINE 54785-02-3 ABECARNIL 111841-85-1 ADAPALENE 106685-40-9 ABITESARTAN 137882-98-5 ADAPROLOL 101479-70-3 ABLUKAST 96566-25-5 ADATANSERIN 127266-56-2 ABUNIDAZOLE 91017-58-2 ADEFOVIR 106941-25-7 ACADESINE 2627-69-2 ADELMIDROL 1675-66-7 ACAMPROSATE 77337-76-9 ADEMETIONINE 17176-17-9 ACAPRAZINE 55485-20-6 ADENOSINE PHOSPHATE 61-19-8 ACARBOSE 56180-94-0 ADIBENDAN 100510-33-6 ACEBROCHOL 514-50-1 ADICILLIN 525-94-0 ACEBURIC ACID 26976-72-7 ADIMOLOL 78459-19-5 ACEBUTOLOL 37517-30-9 ADINAZOLAM 37115-32-5 ACECAINIDE 32795-44-1 ADIPHENINE 64-95-9 ACECARBROMAL 77-66-7 ADIPIODONE 606-17-7 ACECLIDINE 827-61-2 ADITEREN 56066-19-4 ACECLOFENAC 89796-99-6 ADITOPRIM 56066-63-8 ACEDAPSONE 77-46-3 ADOSOPINE 88124-26-9 ACEDIASULFONE SODIUM 127-60-6 ADOZELESIN 110314-48-2 ACEDOBEN 556-08-1 ADRAFINIL 63547-13-7 ACEFLURANOL 80595-73-9 ADRENALONE -

Determination of 17 Hormone Residues in Milk by Ultra-High-Performance Liquid Chromatography and Triple Quadrupole Mass Spectrom
No. LCMSMS-065E Liquid Chromatography Mass Spectrometry Determination of 17 Hormone Residues in Milk by Ultra-High-Performance Liquid Chromatography and Triple Quadrupole No. LCMSMS-65E Mass Spectrometry This application news presents a method for the determination of 17 hormone residues in milk using Shimadzu Ultra-High-Performance Liquid Chromatograph (UHPLC) LC-30A and Triple Quadrupole Mass Spectrometer LCMS- 8040. After sample pretreatment, the compounds in the milk matrix were separated using UPLC LC-30A and analyzed via Triple Quadrupole Mass Spectrometer LCMS-8040. All 17 hormones displayed good linearity within their respective concentration range, with correlation coefficient in the range of 0.9974 and 0.9999. The RSD% of retention time and peak area of 17 hormones at the low-, mid- and high- concentrations were in the range of 0.0102-0.161% and 0.563-6.55% respectively, indicating good instrument precision. Method validation was conducted and the matrix spike recovery of milk ranged between 61.00-110.9%. The limit of quantitation was 0.14-0.975 g/kg, and it meets the requirement for detection of hormones in milk. Keywords: Hormones; Milk; Solid phase extraction; Ultra performance liquid chromatograph; Triple quadrupole mass spectrometry ■ Introduction Since 2008’s melamine-tainted milk scandal, the With reference to China’s national standard GB/T adulteration of milk powder has become a major 21981-2008 "Hormone Multi-Residue Detection food safety concern. In recent years, another case of Method for Animal-derived Food - LC-MS Method", dairy product safety is suspected to cause "infant a method utilizing solid phase extraction, ultra- sexual precocity" (also known as precocious puberty) performance liquid chromatography and triple and has become another major issue challenging the quadrupole mass spectrometry was developed for dairy industry in China. -

INTEGRIS Formulary July 2017
INTEGRIS Formulary July 2017 Foreword FORMULARY EXCLUDED THERAPEUTIC DRUG This document represents the efforts of the MedImpact Healthcare Systems THERAPEUTIC DRUGS CLASS Pharmacy and Therapeutics (P & T) and Formulary Committees to provide ALTERNATIVES physicians and pharmacists with a method to evaluate the safety, efficacy and cost- clindamycin/tretinoin, ACNE AGENTS, effectiveness of commercially available drug products. A structured approach to the VELTIN drug selection process is essential in ensuring continuing patient access to rational ZIANA TOPICAL drug therapies. The ultimate goal of the MedPerform Formulary is to provide a morphine sulfate ER process and framework to support the dynamic evolution of this document to guide tablets, oxycodone ANALGESICS, KADIAN prescribing decisions that reflect the most current clinical consensus associated ER, NUCYNTA, NARCOTICS with drug therapy decisions. NUCYNTA ER ANALGESICS, This is accomplished through the auspices of the MedImpact P & T and Formulary BELBUCA BUTRANS PATCH Committees. These committees meet quarterly and more often as warranted to NARCOTICS ensure clinical relevancy of the Formulary. To accommodate changes to this ABSTRAL, document, updates are made accessible as necessary. FENTORA, fentanyl citrate ANALGESICS, LAZANDA, lozenge NARCOTICS As you use this Formulary, you are encouraged to review the information and ONSOLIS, provide your input and comments to the MedImpact P & T and Formulary SUBSYS Committees. immediate-release GRALISE ANTICONVULSANTS The MedImpact P & T -

Anabolic Steroids/Androgens Pa Summary
ANABOLIC STEROIDS/ANDROGENS PA SUMMARY PREFERRED Anadrol-50, Danazol, Fluoxymesterone, Methitest, Oxandrolone, Testosterone Cypionate Injection, Testosterone Enanthate Injection NON-PREFERRED Android, Testred LENGTH OF AUTHORIZATION: Varies NOTE: All preferred and non-preferred agents require prior authorization. See PA criteria labeled “Topical Testosterone” for Androderm, Androgel, Striant, and Testim. The criteria details below are for the outpatient pharmacy program. If an injectable medication is being administered in a physician’s office then the criteria information below does not apply. Instead, the physician’s office must bill this drug through the DCH physician’s injectable program and not the outpatient pharmacy program. Information regarding the physician’s injectable program can be located at www.mmis.georgia.gov. PA CRITERIA: For Anadrol-50 Approvable for the following diagnoses: anemia caused by deficient red blood cell production, acquired or congenital aplastic anemia, myelofibrosis, hypoplastic anemia due to administration of myelotoxic drugs Also approvable for HIV or AIDS wasting when significant weight loss is documented in members currently receiving nutritional support For Danazol Approvable for the following diagnoses: endometriosis, fibrocystic breast disease, hereditary angioedema For Fluoxymesterone, Methyltestosterone (Android, Methitest, Testred), Testosterone Cypionate or Enanthate Injection Approvable in male members 12 years of age or older for the following diagnoses: primary hypogonadism, secondary -

Printed Formulary Catalog Basic
Scripps Health Formulary July 2016 Foreword Pharmacy and Therapeutics Committee. MedImpact approves such multi- This document represents the efforts of the MedImpact Healthcare Systems source drugs for addition to the MAC list based on the following criteria: Pharmacy and Therapeutics (P & T) and Formulary Committees to provide physicians A multi-source drug product manufactured by at least one (1) nationally and pharmacists with a method to evaluate the safety, efficacy and cost-effectiveness marketed company. of commercially available drug products. A structured approach to the drug selection At least one (1) of the generic manufacturer’s products must have an “A” process is essential in ensuring continuing patient access to rational drug therapies. rating or the generic product has been determined to be unassociated with The ultimate goal of the Portfolio Formulary is to provide a process and framework to efficacy, safety or bioequivalency concerns by the MedImpact P & T support the dynamic evolution of this document to guide prescribing decisions that Committee. reflect the most current clinical consensus associated with drug therapy decisions. Drug product will be approved for generic substitution by the MedImpact P & T Committee. This is accomplished through the auspices of the MedImpact P & T and Formulary Committees. These committees meet quarterly and more often as warranted to ensure This list is reviewed and updated periodically based on the clinical literature and clinical relevancy of the Formulary. To accommodate changes to this document, pharmacokinetic characteristics of currently available versions of these drug updates are made accessible as necessary. products. As you use this Formulary, you are encouraged to review the information and provide If a member or physician requests a brand name product in lieu of an approved your input and comments to the MedImpact P & T and Formulary Committees. -

Role of Androgens on MCF-7 Breast Cancer Cell Growth and on the Inhibitory Effect of Letrozole
Research Article Role of Androgens on MCF-7 Breast Cancer Cell Growth and on the Inhibitory Effect of Letrozole Luciana F. Macedo, Zhiyong Guo, Syreeta L. Tilghman, Gauri J. Sabnis, Yun Qiu, and Angela Brodie Department of Pharmacology and Experimental Therapeutics, University of Maryland, Baltimore, Maryland Abstract hormone therapy and longer patient survival (14). However, the Previous work has shown that androgens inhibit breast cancer physiologic role of endogenous androgens and events following AR cells and tumor growth. On the other hand, androgens can be activation leading to inhibition of cell growth are not clearly identified in breast cancer cells. Some studies have shown that converted to mitogenic estrogens by aromatase in breast cancer cells. Here, we report that androgens, such as the androgens modulate the expression of the Bcl-2protein family in aromatizable androstenedione and the non-aromatizable breast cancer cells, and that their effect is contrary to that of 5A-dihydrotestosterone, inhibit MCF-7 cell proliferation. This estrogens (15, 16). The Bcl-2family proteins both inhibit and effect is observed only in the absence or at a low concentra- promote cell death (16, 17), and the Bcl-2protein has been tion of estrogens and is evident in cells with low aromatase extensively characterized as an inhibitor of apoptosis. activity. Growth of a new aromatase stably transfected MCF-7 Due to their adverse side effects, exogenous androgens were later cell line (Ac1) was stimulated by conversion of androstene- replaced by other better tolerated breast cancer treatment dione into estrogens and was sensitive to aromatase inhib- strategies, such as ER antagonism and aromatase inhibition. -

November Packet
L Buckman Dire cl Diversion Date: October 22,2018 To: Buckman Direct Diversion Board From: Michael Dozier, BDD Operations Superintendent .AAD Subject: Update on BDD Operations for the Month of October 2018 ITEM: 1. This memorandum is to update the Buckman Direct Diversion Board (BDDB) on BDD operations during the month of October 2018. The BDD diversions and deliveries have averaged, in Million Gallons Per Day (MOD) as follows: a. Raw water diversions: 5.66 MOD b. Drinking water deliveries through Booster Station 4N5A: 5.08 MOD c. Raw water delivery to Las Campanas at BS2A: 0.53 MOD d. Onsite treated and non-treated water storage: 0.05 MOD Average 2. The BDD is providing approximately 81% percent of the water supply to the City and County for the month. 3. The BDD year-to-date diversions are depicted below: Year-To-Date Comparison 350.00 , I ®.' Buckman Direct Diversion • 341 Caja del Rio Rd. • Santa Fe, NM 87506 1 4. Background Diversion tables: Buckman Direct Diversion Monthly SJC and Native Diversions Oct-18 In Acre-Feet Total SD-03418 SP-4842 SP-2847-E SP-2847-N-A All Partners SJC+ RGNative Month RG Native SJCCall SJCCall Conveyance Native LAS SJCCall COUNTY CITY LASCAMPANAS Losses Rights CAMPANAS Total JAN 380.137 77.791 0.000 302.346 302.346 0.000 3.023 FEB 336.287 66.413 0.000 269.874 169.874 0.000 2.699 MAR 362.730 266.898 0.000 95.832 95.832 0.000 0.958 APR 661.333 568.669 0.000 92.664 92.664 0.000 0.927 MAY 933.072 340.260 0.000 592.812 481.647 111.165 5.928 JUN 873.384 44.160 0.000 829.224 693.960 135.264 8.292 JUL 807.939 -

Anti-Obesity Therapy: from Rainbow Pills to Polyagonists
1521-0081/70/4/712–746$35.00 https://doi.org/10.1124/pr.117.014803 PHARMACOLOGICAL REVIEWS Pharmacol Rev 70:712–746, October 2018 Copyright © 2018 The Author(s). This is an open access article distributed under the CC BY Attribution 4.0 International license. ASSOCIATE EDITOR: BIRGITTE HOLST Anti-Obesity Therapy: from Rainbow Pills to Polyagonists T. D. Müller, C. Clemmensen, B. Finan, R. D. DiMarchi, and M. H. Tschöp Institute for Diabetes and Obesity, Helmholtz Diabetes Center, Helmholtz Zentrum München, German Research Center for Environmental Health, Neuherberg, Germany (T.D.M., C.C., M.H.T.); German Center for Diabetes Research, Neuherberg, Germany (T.D.M., C.C., M.H.T.); Department of Chemistry, Indiana University, Bloomington, Indiana (B.F., R.D.D.); and Division of Metabolic Diseases, Technische Universität München, Munich, Germany (M.H.T.) Abstract ....................................................................................713 I. Introduction . ..............................................................................713 II. Bariatric Surgery: A Benchmark for Efficacy ................................................714 III. The Chronology of Modern Weight-Loss Pharmacology . .....................................715 A. Thyroid Hormones ......................................................................716 B. 2,4-Dinitrophenol .......................................................................716 C. Amphetamines. ........................................................................717 Downloaded from 1. Methamphetamine -

The Combined Cardiac Effect of the Anabolic Steroid, Nandrolone And
ù1. v -¿. rlc) 77.- *n*hi.rnool oowol,ù*o ffi"/fu -lo *rn*(o fii'o fio¿o¿¿, /v&"ùún lonno **al cooaiæe';¿vfl"- oã. Benjamin D. Phillis, B.Sc. (Hons) Phatmacology Depattment of Clinical & Experimental Pharmacology Ftome Rd. , Medical School Noth Adelaide Univetsity ADEIAIDE SA 5OOO û.)r.'-*hr/7enveltîù Foremost, I would like to thank my two supervisors for the direction that they have given this ptojecr. To Rod, for his unfailing troubleshooting abiJity and to Jenny fot her advice and ability to add scientific rigour' Many thanks to Michael Adams for his technical assistance and especially fot performing the surgery for the ischaemia-reperfusion projects and for his willingness to work late nights and public holidays. Lastly I would like to thank my v¡ife for her extreme patience during the tumult of the last 5 years. Her love, suppoït, patience and undetstanding have been invaluable in this endeavout. Beniamin D. Phillis Octobet,2005 ADE,I-AIDE ii T*(¿t of Ao,t",tù DECI.ARATION I ACKNOWLEDGEMENTS il TABLE OF CONTENTS UI ABBREVIATIONS x ABSTRACT )ilr CÉIAPTER t-l Inttoduction 1-1 1.1 Background 1,-1, 1.2What ate anabolic stetoids? 7-1 1,3 General pharmacology of Anabolic steroids t-2 '1,-2 1.3.1 Genomic effects of anabolic steroids 1.3.2 Non-genomic effects of anabolic steroids 1-3 1.4 Clinical use of AS 1.-4 1.5 Patterns of AS abuse 1.-4 1.5.1 Steroid abuse by athletes 1.-+ 1.5.2 Stetoid abuse by sedentary teenagers r-6 1.5.3 Prevalence of abuse 1-6 1.5.4 Abuse ptevalence in Australia 1.-9 1.6 Cardiotoxicity of anabolic steroids r-9 1.6.1 Reduced cotonary flow 1.-1.1, 1,.6.2 Dtect myocatdial eff ects 1-1 5 1.6.3 Hypertension 1-21 1.7 Difficulties associated with anabolic steroid research 1.-24 1-25 1.8 The polydrug abuse Phenomenon 1.9 The pharmacology of cocaine 1-26 1.10 Pteparations 1-28 1-29 1.11 Metabolism lll 1-30 1. -

A Review of Palliative Therapies for Cancer- Associated Anorexia
58 Review Article A hunger for hunger: a review of palliative therapies for cancer- associated anorexia Daniel S. Childs1, Aminah Jatoi2 1Department of Medicine, 2Department of Oncology, Mayo Clinic, Rochester, MN, USA Contributions: (I) Conception and design: All authors; (II) Administrative support: DS Childs; (III) Provision of study materials or patients: None; (IV) Collection and assembly of data: All authors; (V) Data analysis and interpretation: All authors; (VI) Manuscript writing: All authors; (VII) Final approval of manuscript: All authors. Correspondence to: Aminah Jatoi, MD. Mayo Clinic, 200 First Street SW, Rochester, MN 55905, USA. Email: [email protected]. Abstract: Cancer-associated anorexia, or loss of appetite, is prevalent, distressing to patients and their families, and associated with poorer outcomes in patients with advanced cancer. A well-defined therapeutic strategy remains to be defined. We present here a review of appetite loss in cancer patients with a summary of how best to manage this symptom. Keywords: Loss of appetite, anorexia, appetite stimulants, cancer, nutrition Submitted Mar 05, 2018. Accepted for publication May 07, 2018. doi: 10.21037/apm.2018.05.08 View this article at: http://dx.doi.org/10.21037/apm.2018.05.08 Introduction of appetite is common among cancer patients. What are the implications of loss of appetite in patients Many patients with advanced, incurable cancer suffer with cancer? Importantly, cancer-associated loss of appetite from loss of appetite, herein referred to as anorexia. The is not a simple, isolated symptom. It often occurs in the prevalence of this symptom varies from study to study. presence of a multiplicity of other symptoms like pain, Reporting on data from the PreMiO Study that included fatigue, and weakness; however, even after accounting 1,952 cancer patients, Muscaritoli and others noted that for the effects of other variables, the presence of cancer- 40% of patients reported loss of appetite as per a validated associated anorexia was found to strongly influence patient questionnaire (1). -

WO 2012/148570 Al 1 November 2012 (01.11.2012) P O P C T
(12) INTERNATIONAL APPLICATION PUBLISHED UNDER THE PATENT COOPERATION TREATY (PCT) (19) World Intellectual Property Organization International Bureau (10) International Publication Number (43) International Publication Date WO 2012/148570 Al 1 November 2012 (01.11.2012) P O P C T (51) International Patent Classification: AO, AT, AU, AZ, BA, BB, BG, BH, BR, BW, BY, BZ, A61L 27/14 (2006.01) A61P 17/02 (2006.01) CA, CH, CL, CN, CO, CR, CU, CZ, DE, DK, DM, DO, C08L 101/16 (2006.01) DZ, EC, EE, EG, ES, FI, GB, GD, GE, GH, GM, GT, HN, HR, HU, ID, IL, IN, IS, JP, KE, KG, KM, KN, KP, KR, (21) International Application Number: KZ, LA, LC, LK, LR, LS, LT, LU, LY, MA, MD, ME, PCT/US20 12/027464 MG, MK, MN, MW, MX, MY, MZ, NA, NG, NI, NO, NZ, (22) International Filing Date: OM, PE, PG, PH, PL, PT, QA, RO, RS, RU, RW, SC, SD, 2 March 2012 (02.03.2012) SE, SG, SK, SL, SM, ST, SV, SY, TH, TJ, TM, TN, TR, TT, TZ, UA, UG, US, UZ, VC, VN, ZA, ZM, ZW. (25) Filing Language: English (84) Designated States (unless otherwise indicated, for every (26) Publication Language: English kind of regional protection available): ARIPO (BW, GH, (30) Priority Data: GM, KE, LR, LS, MW, MZ, NA, RW, SD, SL, SZ, TZ, 13/093,479 25 April 201 1 (25.04.201 1) US UG, ZM, ZW), Eurasian (AM, AZ, BY, KG, KZ, MD, RU, TJ, TM), European (AL, AT, BE, BG, CH, CY, CZ, DE, (71) Applicant (for all designated States except US): DK, EE, ES, FI, FR, GB, GR, HR, HU, IE, IS, IT, LT, LU, WARSAW ORTHOPEDIC, INC.