Current Challenges in Pharmacovigilance: Pragmatic Approches
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

OCCUPATIONAL MEDICINE PROGRAM HANDBOOK October 2005
U.S. DEPARTMENT OF THE INTERIOR OFFICE OF OCCUPATIONAL HEALTH AND SAFETY OCCUPATIONAL MEDICINE PROGRAM HANDBOOK October 2005 This Occupational Medicine Program Handbook was prepared by the U.S. Department of the Interior’s Office of Occupational Health and Safety, in consultation with the U.S. Office of Personnel Management and the U.S. Public Health Service’s Federal Occupational Health service. This edition of the Handbook represents the continuing efforts of the contributing agencies to improve occupational health services for DOI employees. It reflects the comments and suggestions offered by users over the years since it was first introduced, and addresses the findings, concerns, and recommendations summarized in the final report of a program review completed in 1994 by representatives of the Uniformed Services University of the Health Sciences. That report, entitled “A Review of the Occupational Health Program of the United States Department of the Interior,” was prepared by Margaret A.K. Ryan, M.D., M.P.H., Gail Gullickson, M.D., M.P.H., W. Garry Rudolph, M.D., M.P.H., and Elizabeth Odell. The report led to the establishment of the Department’s Occupational Health Reinvention Working Group, composed of representatives from the DOI bureaus and operating divisions. The recommendations from the Reinvention Working Group final report, published in May of 1996, were addressed and are reflected in what became this Handbook. First published in 1997, the Handbook underwent a major update in July, 2000. This 2005 version of the Handbook incorporates the updates and enhancements that have been made in DOI policies and occupational medicine practice since the last edition. -

Drug Safety in Translational Paediatric Research: Practical Points to Consider for Paediatric Safety Profiling and Protocol Development: a Scoping Review
pharmaceutics Review Drug Safety in Translational Paediatric Research: Practical Points to Consider for Paediatric Safety Profiling and Protocol Development: A Scoping Review Beate Aurich 1 and Evelyne Jacqz-Aigrain 1,2,* 1 Department of Pharmacology, Saint-Louis Hospital, 75010 Paris, France; [email protected] 2 Paris University, 75010 Paris, France * Correspondence: [email protected] Abstract: Translational paediatric drug development includes the exchange between basic, clinical and population-based research to improve the health of children. This includes the assessment of treatment related risks and their management. The objectives of this scoping review were to search and summarise the literature for practical guidance on how to establish a paediatric safety specification and its integration into a paediatric protocol. PubMed, Embase, Web of Science, and websites of regulatory authorities and learned societies were searched (up to 31 December 2020). Retrieved citations were screened and full texts reviewed where applicable. A total of 3480 publica- tions were retrieved. No article was identified providing practical guidance. An introduction to the practical aspects of paediatric safety profiling and protocol development is provided by combining health authority and learned society guidelines with the specifics of paediatric research. The paedi- atric safety specification informs paediatric protocol development by, for example, highlighting the Citation: Aurich, B.; Jacqz-Aigrain, E. need for a pharmacokinetic study prior to a paediatric trial. It also informs safety related protocol Drug Safety in Translational Paediatric Research: Practical Points sections such as exclusion criteria, safety monitoring and risk management. In conclusion, safety to Consider for Paediatric Safety related protocol sections require an understanding of the paediatric safety specification. -
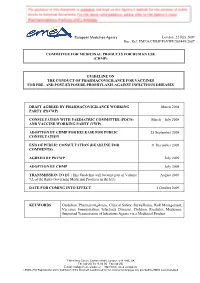
Guideline on the Conduct of Pharmacovigilance for Vaccines for Pre- and Post-Exposure Prophylaxis Against Infectious Diseases
European Medicines Agency London, 22 July 2009 Doc. Ref. EMEA/CHMP/PhVWP/503449/2007 COMMITTEE FOR MEDICINAL PRODUCTS FOR HUMAN USE (CHMP) GUIDELINE ON THE CONDUCT OF PHARMACOVIGILANCE FOR VACCINES FOR PRE- AND POST-EXPOSURE PROPHYLAXIS AGAINST INFECTIOUS DISEASES DRAFT AGREED BY PHARMACOVIGILANCE WORKING March 2008 PARTY (PhVWP) CONSULTATION WITH PAEDIATRIC COMMITTEE (PDCO) March – July 2008 AND VACCINE WORKING PARTY (VWP) ADOPTION BY CHMP FOR RELEASE FOR PUBLIC 25 September 2008 CONSULTATION END OF PUBLIC CONSULTATION (DEADLINE FOR 31 December 2008 COMMENTS) AGREED BY PhVWP July 2009 ADOPTION BY CHMP July 2009 TRANSMISSION TO EC (This Guideline will become part of Volume August 2009 9A of the Rules Governing Medicinal Products in the EU). DATE FOR COMING INTO EFFECT 1 October 2009 KEYWORDS Guideline, Pharmacovigilance, Clinical Safety, Surveillance, Risk Management, Vaccines, Immunisation, Infectious Diseases, Children, Paediatric Medicines, Suspected Transmission of Infectious Agents via a Medicinal Product 7 Westferry Circus, Canary Wharf, London, E14 4HB, UK Tel. (44-20) 74 18 84 00 Fax (44-20) E-mail: [email protected] http://www.emea.europa.eu ©EMEA 2009 Reproduction and/or distribution of this document is authorised for non commercial purposes only provided the EMEA is acknowledged GUIDELINE ON THE CONDUCT OF PHARMACOVIGILANCE FOR VACCINES FOR PRE- AND POST-EXPOSURE PROPHYLAXIS AGAINST INFECTIOUS DISEASES TABLE OF CONTENTS EXECUTIVE SUMMARY_______________________________________________________ 3 1. Introduction ____________________________________________________________ -

Guidance for Industry E2E Pharmacovigilance Planning
Guidance for Industry E2E Pharmacovigilance Planning U.S. Department of Health and Human Services Food and Drug Administration Center for Drug Evaluation and Research (CDER) Center for Biologics Evaluation and Research (CBER) April 2005 ICH Guidance for Industry E2E Pharmacovigilance Planning Additional copies are available from: Office of Training and Communication Division of Drug Information, HFD-240 Center for Drug Evaluation and Research Food and Drug Administration 5600 Fishers Lane Rockville, MD 20857 (Tel) 301-827-4573 http://www.fda.gov/cder/guidance/index.htm Office of Communication, Training and Manufacturers Assistance, HFM-40 Center for Biologics Evaluation and Research Food and Drug Administration 1401 Rockville Pike, Rockville, MD 20852-1448 http://www.fda.gov/cber/guidelines.htm. (Tel) Voice Information System at 800-835-4709 or 301-827-1800 U.S. Department of Health and Human Services Food and Drug Administration Center for Drug Evaluation and Research (CDER) Center for Biologics Evaluation and Research (CBER) April 2005 ICH Contains Nonbinding Recommendations TABLE OF CONTENTS I. INTRODUCTION (1, 1.1) ................................................................................................... 1 A. Background (1.2) ..................................................................................................................2 B. Scope of the Guidance (1.3)...................................................................................................2 II. SAFETY SPECIFICATION (2) ..................................................................................... -

Role and Value of the Corporate Medical Director
ACOEM GUIDANCE STATEMENT Role and Value of the Corporate Medical Director J. Brent Pawlecki, MD, MMM, Wayne N. Burton, MD, Cherryl Christensen, DO, MS, K. Andrew Crighton, MD, Richard Heron, MB, ChB, FRCP, T. Warner Hudson, MD, Pamela A. Hymel, MD, MPH, and David Roomes, FFOM, FACOEM, ACOEM Corporate Medical Directors Section Task Force accreditation in occupational medicine or the more preferred double The role of the corporate medical director (CMD) has evolved over the last certification in occupational medicine, and another board such as 300 years since Ramazzini first identified diseases of Italian workers in the 01/04/2019 on BhDMf5ePHKav1zEoum1tQfN4a+kJLhEZgbsIHo4XMi0hCywCX1AWnYQp/IlQrHD3VFjldD2uL9p7SMbj5XQFggscApMlmW/UgXNoK/5MD7Gq31Q2YQqh0A== by https://journals.lww.com/joem from Downloaded Downloaded internal medicine or family medicine. Further qualifications such as a early 1700s. Since then, there has been a gradual blurring of the boundaries master of public health or masters-level degree in environmental between private and workplace health concerns. Today’s CMD must have health, business administration, or law are highly desirable, including from intimate knowledge of their corporation’s industry and the businesses that knowledge of epidemiology, biostatistics, population health manage- https://journals.lww.com/joem they support, particularly the occupational and environmental programs that ment, business management, and regulatory aspects of employee comply with all local, state, and/or national standards and regulations. health. CMDs should also remain active in their relevant professional Leading companies not only measure compliance with such standards but health organizations to demonstrate that they are remaining current in also may hold programs to their own internal corporate global standards even medicine. -

Standards, Principles and Approaches in Occupational Health Services
STANDARDS, PRINCIPLES AND APPROACHES IN OCCUPATIONAL HEALTH SERVICES Jorma Rantanen, Igor A. Fedotov This article is based on the standards, principles and approaches embodied in the ILO Occupational Health Services Convention, 1985 (No. 161) and its accompanying Recommendation (No. 171); ILO Occupational Safety and Health Convention, 1981 (No. 155) and its accompanying Recommendation (No. 164); and the Working Document of the Twelfth Session of the Joint ILO/WHO Committee on Occupational Health, 5-7 April 1995. The ILO Occupational Health Services Convention (No. 161) defines “occupational health services” as services entrusted with essentially preventive functions and responsible for advising the employer, the workers and their representatives in the undertaking on the requirements for establishing and maintaining a safe and healthy working environment which will facilitate optimal physical and mental health in relation to work and the adaptation of work to the capabilities of workers in the light of their state of physical and mental health. Provision of occupational health services means carrying out activities in the workplace with the aim of protecting and promoting workers’ safety, health and well-being, as well as improving working conditions and the working environment. These services are provided by occupational health professionals functioning individually or as part of special service units of the enterprise or of external services. Occupational health practice is broader and consists not only of the activities performed by the occupational health service. It is multidisciplinary and multisectoral activity involving in addition to occupational health and safety professionals other specialists both in the enterprise and outside, as well as competent authorities, the employers, workers and their representatives. -

Ecological Impacts of Veterinary Pharmaceuticals: More Transparency – Better Protection of the Environment
Ecological Impacts of Veterinary Pharmaceuticals: More Transparency – Better Protection of the Environment Avoiding Environmental Pollution from Veterinary Pharmaceuticals To reduce the contamination of air, soil, and bodies of pharmaceuticals more stringently, monitoring systematically water caused by veterinary medicinal products used in their occurrence in the environment, converting animal hus- agriculture and livestock farming, effective measures bandry practices to preserve animals’ health with a minimal must be taken throughout the entire life cycle of these use of antibiotics, and enforcing legal regulations to ensure products – from production and authorisation to appli- implementation of all the measures outlined here. cation and disposal. In the context of the revision of veterinary medicinal products All stakeholders – whether they are farmers, veterinarians, legislation that is currently underway, this background paper consumers, or political decision makers – are called upon focuses on three measures that would contribute to mak- to contribute to reducing contamination of the environment ing information on the occurrence of veterinary drugs in the caused by pharmaceutical residues and to improving pro- environment and their eco-toxicological effects more widely tection of the environment and human health. Appropriate available and enhance protection of the environment from measures include establishing “clean” production plants, contamination with veterinary pharmaceuticals. developing pharmaceuticals with reduced environmental -

Approach to a Patient with Hemiplegia and Monoplegia
CHAPTER Approach to a Patient with Hemiplegia and Monoplegia 27 Sudhir Kumar, Subhash Kaul INTRODUCTION 4. Injury to multiple cervical nerve roots. Monoplegia and hemiplegia are common neurological 5. Functional or psychogenic. symptoms in patients presenting to the emergency department as well as outpatient department. Insidious onset, gradually progressive monoplegia affecting lower limb can be caused by the following Monoplegia refers to weakness of one limb (either arm or conditions: leg) and hemiplegia refers to weakness of one arm and leg on the same side of body (either left or right side). 1. Tumor of the contralateral frontal lobe. There are a variety of underlying causes for monoplegia 2. Tumor of spinal cord at thoracic or lumbar level. and hemiplegia. The causes differ in different age groups. 3. Chronic infection of brain (frontal lobe) or spinal The causes also differ depending on the onset, progression cord (thoracic or lumbar level), such as tuberculous. and duration of weakness. Therefore, one needs to adopt a systematic approach during history taking and 4. Lumbosacral-plexopathy, due to diabetes mellitus. examination in order to arrive at the correct diagnosis. Insidious onset, gradually progressive monoplegia, Appropriate investigations after these would confirm the affecting upper limb, can be caused by one of the following diagnosis. conditions: The aim of this chapter is to systematically look at the 1. Tumor of the contralateral parietal lobe. differential diagnosis of monoplegia and hemiplegia and outline the approach needed to pinpoint the exact 2. Compressive lesion (tumor, large disc, etc) in underlying cause. cervical cord region. 3. Chronic infection of the brain (parietal lobe) or APPROACH TO THE DIAGNOSIS OF MONOPLEGIA spinal cord (cervical region), such as tuberculous. -

2021 Onsite Employee Health Clinics Summit
2021 Onsite Employee Health Clinics Summit The Leading Forum on Building & Expanding On-Site Health Clinics – Incorporating Strategies that Reduce Costs, Ensure Employee Satisfaction and Positively Impact Patient Behavior January 28 – 29, 2021 • DoubleTree Resort by Hilton Paradise Valley • Scottsdale, AZ List of Past Attendees Title Company Director, Human Resources City of Douglasville, Georgia CAO Phil Long Dealerships Managing Director H4D Administrator Decorator Industries Vice President of Sales CareATC Account Executive Merck & Co., Inc. Operations Manager Healthcare Solutions Center, LLC CEO Northwind Pharmaceuticals Business Strategist Occupational Health Solutions COO Northwind Pharmaceuticals Wellness Coordinator City of Phoenix Vice President Business Development ChristianaCare National Association of Worksite Health Executive Director Centers Sr Director, Human Resources Tucson Electric Power President Health Cost & Risk Management LLC VP, Operations Premise Health Director, Employee Benefits & Well-being Herman Miller, Inc. Regional Director North Ms. Medical Clinics Director Wellness Programs Tahoe Forest Hospital VP HR & Risk Management Phil Long Dealerships Director of Clinic Operations Baylor Scott & White CEO Moss CM National Director-Employers Amgen SR. VP Human Resources and Foundation La Posada Acting CEO Southern Indian Health Council VP, Operations Premise Health Associate OMERS Private Equity Manager Stanford Healthcare New Business Development Manager Roche Diabetes Care Chief Executive Officer Premise Health -

Myelopathy—Paresis and Paralysis in Cats
Myelopathy—Paresis and Paralysis in Cats (Disorder of the Spinal Cord Leading to Weakness and Paralysis in Cats) Basics OVERVIEW • “Myelopathy”—any disorder or disease affecting the spinal cord; a myelopathy can cause weakness or partial paralysis (known as “paresis”) or complete loss of voluntary movements (known as “paralysis”) • Paresis or paralysis may affect all four limbs (known as “tetraparesis” or “tetraplegia,” respectively), may affect only the rear legs (known as “paraparesis” or “paraplegia,” respectively), the front and rear leg on the same side (known as “hemiparesis” or “hemiplegia,” respectively) or only one limb (known as “monoparesis” or “monoplegia,” respectively) • Paresis and paralysis also can be caused by disorders of the nerves and/or muscles to the legs (known as “peripheral neuromuscular disorders”) • The spine is composed of multiple bones with disks (intervertebral disks) located in between adjacent bones (vertebrae); the disks act as shock absorbers and allow movement of the spine; the vertebrae are named according to their location—cervical vertebrae are located in the neck and are numbered as cervical vertebrae one through seven or C1–C7; thoracic vertebrae are located from the area of the shoulders to the end of the ribs and are numbered as thoracic vertebrae one through thirteen or T1–T13; lumbar vertebrae start at the end of the ribs and continue to the pelvis and are numbered as lumbar vertebrae one through seven or L1–L7; the remaining vertebrae are the sacral and coccygeal (tail) vertebrae • The brain -

Absence of Neurobehavioral Disturbance in a Focal Lesion of the Left Paracentral Lobule
Behavioural Neurology (1992), 5,189-191 ICASE REPORTI Absence of neurobehavioral disturbance in a focal lesion of the left paracentral lobule T. Imamura and K. Tsuburaya Department of Neurology, Tohoku Kohseinenkin Hospital, Sendai, Japan Correspondence to: T. Imamura, Department of Neurology, Institute of Brain Diseases, Tohoku University School of Medicine, 1-1, Seiryo-machi, Aoba-Ku, Sendai 980, Japan The case of a right-handed woman with an infarcation confined to the left paracentral lobule and sparing the supplementary motor area (SMA) is reported. She presented with a right leg monoplegia and displayed no mutism. The absence of any associ ated neurobehavioral disturbances (mutism, forced grasping, reduced spontaneous arm activity or aphasia raises the possi bility that the left SMA has discrete neurobehavioral functions. Keywords: Medial frontal lobe - Precentral gyrus - Supplementary motor area - Transcortical motor aphasia INTRODUCTION Various kinds of neurobehavioral disturbances associated medial part of the left precentral gyrus, which is adjacent with left medial frontal lesions involving the supplemen to the SMA, to evaluate its possible neurobehavioral tary motor area (SMA) have been reported. Aphasia due to functions. damage of the left medial frontal lobe is characterized by an initial period of mutism followed by a stage of CASE REPORT decreased verbal output and spontaneous initiation with normal articulation (Stuss and Benson, 1986). Forced A 73-year-old right-handed woman with a history of grasping, compulsive manipulation of tools and decreased hypertension and diabetes mellitus suddenly developed a spontaneous limb movements have also been described gait disturbance. On examination, 24 h later, she was alert (Wise, 1984; Feinberg et al., 1992). -

ICD9 & ICD10 Neuromuscular Codes
ICD-9-CM and ICD-10-CM NEUROMUSCULAR DIAGNOSIS CODES ICD-9-CM ICD-10-CM Focal Neuropathy Mononeuropathy G56.00 Carpal tunnel syndrome, unspecified Carpal tunnel syndrome 354.00 G56.00 upper limb Other lesions of median nerve, Other median nerve lesion 354.10 G56.10 unspecified upper limb Lesion of ulnar nerve, unspecified Lesion of ulnar nerve 354.20 G56.20 upper limb Lesion of radial nerve, unspecified Lesion of radial nerve 354.30 G56.30 upper limb Lesion of sciatic nerve, unspecified Sciatic nerve lesion (Piriformis syndrome) 355.00 G57.00 lower limb Meralgia paresthetica, unspecified Meralgia paresthetica 355.10 G57.10 lower limb Lesion of lateral popiteal nerve, Peroneal nerve (lesion of lateral popiteal nerve) 355.30 G57.30 unspecified lower limb Tarsal tunnel syndrome, unspecified Tarsal tunnel syndrome 355.50 G57.50 lower limb Plexus Brachial plexus lesion 353.00 Brachial plexus disorders G54.0 Brachial neuralgia (or radiculitis NOS) 723.40 Radiculopathy, cervical region M54.12 Radiculopathy, cervicothoracic region M54.13 Thoracic outlet syndrome (Thoracic root Thoracic root disorders, not elsewhere 353.00 G54.3 lesions, not elsewhere classified) classified Lumbosacral plexus lesion 353.10 Lumbosacral plexus disorders G54.1 Neuralgic amyotrophy 353.50 Neuralgic amyotrophy G54.5 Root Cervical radiculopathy (Intervertebral disc Cervical disc disorder with myelopathy, 722.71 M50.00 disorder with myelopathy, cervical region) unspecified cervical region Lumbosacral root lesions (Degeneration of Other intervertebral disc degeneration,