Interplay Between Cellular and Molecular Mechanisms Underlying Inflammatory Bowel Diseases Development—A Focus on Ulcerative Colitis
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Autophagy: from Basic Science to Clinical Application
nature publishing group REVIEW See COMMENTARY page XX Autophagy: from basic science to clinical application J Va n L i m b e r g e n 1 , 2 , 3 , C S t e v e n s 4 , E R N i m m o 1 , D C W i l s o n 2 , 3 a n d J S a t s a n g i 1 Autophagy is a cellular pathway involved in protein and organelle degradation, which is likely to represent an innate adaptation to starvation. In times of nutrient deficiency, the cell can self-digest and recycle some nonessential components through nonselective autophagy, thus sustaining minimal growth requirements until a food source becomes available. Over recent years, autophagy has been implicated in an increasing number of clinical scenarios, notably infectious diseases, cancer, neurodegenerative diseases, and autoimmunity. The recent identification of the importance of autophagy genes in the genetic susceptibility to Crohn ’ s disease suggests that a selective autophagic response may play a crucial role in the pathogenesis of common complex immune-mediated diseases. In this review, we discuss the autophagic mechanisms, their molecular regulation, and summarize their clinical relevance. This progress has led to great interest in the therapeutic potential of manipulation of both selective and nonselective autophagy in established disease. INTRODUCTION The ability to adapt to environmental change is essential for sur- Autophagy encompasses several distinct processes involving vival. This is true for the organism as a whole and for individual the delivery of portions of the cytoplasm to the lysosome for cells alike. -

Deficiency in Class III PI3-Kinase Confers Postnatal Lethality with IBD
ARTICLE DOI: 10.1038/s41467-018-05105-8 OPEN Deficiency in class III PI3-kinase confers postnatal lethality with IBD-like features in zebrafish Shaoyang Zhao1,2,3, Jianhong Xia2,3, Xiuhua Wu2,3, Leilei Zhang2,3, Pengtao Wang2,3, Haiyun Wang2,3, Heying Li2, Xiaoshan Wang 2, Yan Chen 2, Jean Agnetti2, Yinxiong Li 2, Duanqing Pei2,3 & Xiaodong Shu2,3 The class III PI3-kinase (PIK3C3) is an enzyme responsible for the generation of phospha- tidylinositol 3-phosphate (PI3P), a critical component of vesicular membrane. Here, we report 1234567890():,; that PIK3C3 deficiency in zebrafish results in intestinal injury and inflammation. In pik3c3 mutants, gut tube forms but fails to be maintained. Gene expression analysis reveals that barrier-function-related inflammatory bowel disease (IBD) susceptibility genes (e-cadherin, hnf4a, ttc7a) are suppressed, while inflammatory response genes are stimulated in the mutants. Histological analysis shows neutrophil infiltration into mutant intestinal epithelium and the clearance of gut microbiota. Yet, gut microorganisms appear dispensable as mutants cultured under germ-free condition have similar intestinal defects. Mechanistically, we show that PIK3C3 deficiency suppresses the formation of PI3P and disrupts the polarized dis- tribution of cell-junction proteins in intestinal epithelial cells. These results not only reveal a role of PIK3C3 in gut homeostasis, but also provide a zebrafish IBD model. 1 School of Life Sciences, University of Science and Technology of China, 230027 Hefei, Anhui, China. 2 CAS Key Laboratory of Regenerative Biology, Guangzhou Institute of Biomedicine and Health-Guangzhou Medical University Joint School of Biological Sciences, South China Institute for Stem Cell Biology and Regenerative Medicine, Guangzhou Institutes of Biomedicine and Health, Chinese Academy of Sciences, 510530 Guangzhou, China. -

Xxviiith Belgian Week of Gastroenterology 2016 All Abstracts Belgian Association for the Study of the Liver (BASL)
XXVIIIth Belgian Week of Gastroenterology 2016 All Abstracts Belgian Association for the Study of the Liver (BASL) A01 Light-to-moderate alcohol intake increases the risk of hepatocellular carcinoma in patients with HCV-related compensated cirrhosis: a prospective study H. VANDENBULCKE (1), C. MORENO (2), I. COLLE (3), J. KNEBEL (4), S. FRANCQUE (5), T. SERSTÉ (6), C. GEORGE (7), C. DE GALOCSY (8), W. LALEMAN (9), J. DELWAIDE (10), H. ORLENT (11), L. LASSER (12), E. TRÉPO (2), H. VAN VLIERBERGHE (3), P. MICHIELSEN (5), M. VAN GOSSUM (6), M. DE VOS (1), A. MAROT (13), C. DOERIG (13), M. ADLER (2), J. HENRION (1), P. DELTENRE (13) / [1] Hôpital de Jolimont, Haine-Saint-Paul, Belgium, Departement of Gastroenterology and Hepatology, [2] Erasme Hospital, Brussels, Belgium, Department of Gastroenterology, Hepatopancreatology and Digestive Oncology, [3] Ghent University, Ghent, Belgium, Departement of Gastroenterology and Hepatology, [4] Centre Hospitalier Universitaire Vaudois, Lausanne, Switzerland, Division of Radiology, [5] Antwerp University Hospital, Edegem, Belgium, Departement of Gastroenterology and Hepatology, [6] CHU Saint-Pierre, Brussels, Belgium, Departement of Gastroenterology and Hepatology, [7] AZ Groeninge, Kortrijk, Belgium, Departement of Gastroenterology and Hepatology, [8] Hôp. Iris Sud Bracops, Bruxelles, Belgium, Departement of Gastroenterology and Hepatology, [9] KU, Leuven, Belgium, Departement of Gastroenterology and Hepatology, [10] CHU Liege, Liège, Belgium, Departement of Gastroenterology and Hepatology, [11] AZ St. Jan Brugge AV, Brugge, Belgium, Departement of Gastroenterology and Hepatology, [12] CHU Brugmann, , Belgium, Departement of Gastroenterology and Hepatology, [13] Centre Hospitalier Universitaire Vaudois, Lausanne, Switzerland, Division of Gastroenterology and Hepatology Introduction: Whether light-to-moderate alcohol intake increases the risk of complications in patients with HCV-related cirrhosis remains unclear. -

Ifng-Induced Irgm1 Promotes Tumorigenesis of Melanoma Via Dual Regulation of Apoptosis and Bif-1-Dependent Autophagy
Oncogene (2015) 34, 5363–5371 © 2015 Macmillan Publishers Limited All rights reserved 0950-9232/15 www.nature.com/onc ORIGINAL ARTICLE IFNg-induced Irgm1 promotes tumorigenesis of melanoma via dual regulation of apoptosis and Bif-1-dependent autophagy H Dong1,2,5, L Tian1,5,RLi3,CPei1,YFu1, X Dong1, F Xia1, C Wang1,WLi1, X Guo1,CGu1,BLi1, A Liu4, H Ren1, C Wang2 and H Xu1 Interferon gamma (IFNg) has been known as the regulator for both tumor immune surveillance and tumorgenesis. However, mechanisms underlying the resistance of tumor cell to IFNg have yet been fully understood. In the current study, we showed that immunity-related GTPase family member 1 (mouse: Irgm1; human: IRGM) is essential for IFNg-mediated regulation of tumor cell growth in melanoma. IRGM/Irgm1 was highly expressed in human and mouse melanoma. IFNg and starvation synergistically induced Irgm1 expression in melanoma B16 cells. In vivo, injection of Irgm1-siRNA-treated cells significantly reduced the number of tumor nodules and prolonged the mice survival. In vitro, knockdown endogenous or IFNg-induced Irgm1 significantly decreases the proliferation and increases apoptosis of B16 cells. In addition, suppressing Irgm1 decreased the IFNg/starvation-induced autophagy, while overexpressing Irgm1 significantly increased autophagy and rescued starvation-challenged cells. Moreover, IFNg and starvation-induced the co-localization of Irgm1 with Bax-interacting factor 1 (Bif-1). Knockdown of Bif-1 decreased Irgm1-mediated tumor cell autophagy. Taken together, these data reveal an Irgm1-dependent mechanism that promotes the tumorigenesis of melanoma via dual regulation of apoptosis and Bif-1-dependent autophagy. -

Autophagy, Unfolded Protein Response, and Neuropilin-1 Cross-Talk in SARS-Cov-2 Infection: What Can Be Learned from Other Coronaviruses
International Journal of Molecular Sciences Review Autophagy, Unfolded Protein Response, and Neuropilin-1 Cross-Talk in SARS-CoV-2 Infection: What Can Be Learned from Other Coronaviruses Morvarid Siri 1 , Sanaz Dastghaib 2 , Mozhdeh Zamani 1 , Nasim Rahmani-Kukia 3 , Kiarash Roustai Geraylow 4 , Shima Fakher 3, Fatemeh Keshvarzi 3, Parvaneh Mehrbod 5 , Mazaher Ahmadi 6 , Pooneh Mokarram 1,3,* , Kevin M. Coombs 7 and Saeid Ghavami 1,8,9,* 1 Autophagy Research Center, Shiraz University of Medical Sciences, Shiraz 7134845794, Iran; [email protected] (M.S.); [email protected] (M.Z.) 2 Endocrinology and Metabolism Research Center, Shiraz University of Medical Sciences, Shiraz 7193635899, Iran; [email protected] 3 Department of Biochemistry, Shiraz University of Medical Sciences, Shiraz 7134845794, Iran; [email protected] (N.R.-K.); [email protected] (S.F.); [email protected] (F.K.) 4 Student Research Committee, Semnan University of Medical Sciences, Semnan 3514799422, Iran; [email protected] 5 Influenza and Respiratory Viruses Department, Pasteur Institute of Iran, Tehran 1316943551, Iran; [email protected] 6 Faculty of Chemistry, Bu-Ali Sina University, Hamedan 6517838695, Iran; [email protected] 7 Department of Medical Microbiology and Infectious Diseases, Rady Faculty of Health Sciences, Max Rady Citation: Siri, M.; Dastghaib, S.; College of Medicine, University of Manitoba, Winnipeg, MB R3E 0J9, Canada; [email protected] Zamani, M.; Rahmani-Kukia, N.; 8 Department of Human Anatomy and Cell Science, Rady Faculty of Health Sciences, Max Rady College Geraylow, K.R.; Fakher, S.; Keshvarzi, of Medicine, University of Manitoba, Winnipeg, MB R3E 0J9, Canada F.; Mehrbod, P.; Ahmadi, M.; 9 Faculty of Medicine, Katowice School of Technology, 40-555 Katowice, Poland Mokarram, P.; et al. -

Supp Table 6.Pdf
Supplementary Table 6. Processes associated to the 2037 SCL candidate target genes ID Symbol Entrez Gene Name Process NM_178114 AMIGO2 adhesion molecule with Ig-like domain 2 adhesion NM_033474 ARVCF armadillo repeat gene deletes in velocardiofacial syndrome adhesion NM_027060 BTBD9 BTB (POZ) domain containing 9 adhesion NM_001039149 CD226 CD226 molecule adhesion NM_010581 CD47 CD47 molecule adhesion NM_023370 CDH23 cadherin-like 23 adhesion NM_207298 CERCAM cerebral endothelial cell adhesion molecule adhesion NM_021719 CLDN15 claudin 15 adhesion NM_009902 CLDN3 claudin 3 adhesion NM_008779 CNTN3 contactin 3 (plasmacytoma associated) adhesion NM_015734 COL5A1 collagen, type V, alpha 1 adhesion NM_007803 CTTN cortactin adhesion NM_009142 CX3CL1 chemokine (C-X3-C motif) ligand 1 adhesion NM_031174 DSCAM Down syndrome cell adhesion molecule adhesion NM_145158 EMILIN2 elastin microfibril interfacer 2 adhesion NM_001081286 FAT1 FAT tumor suppressor homolog 1 (Drosophila) adhesion NM_001080814 FAT3 FAT tumor suppressor homolog 3 (Drosophila) adhesion NM_153795 FERMT3 fermitin family homolog 3 (Drosophila) adhesion NM_010494 ICAM2 intercellular adhesion molecule 2 adhesion NM_023892 ICAM4 (includes EG:3386) intercellular adhesion molecule 4 (Landsteiner-Wiener blood group)adhesion NM_001001979 MEGF10 multiple EGF-like-domains 10 adhesion NM_172522 MEGF11 multiple EGF-like-domains 11 adhesion NM_010739 MUC13 mucin 13, cell surface associated adhesion NM_013610 NINJ1 ninjurin 1 adhesion NM_016718 NINJ2 ninjurin 2 adhesion NM_172932 NLGN3 neuroligin -

Identifying RNA-Protein Interaction Sites Throughout Eukaryotic Transcriptomes
University of Pennsylvania ScholarlyCommons Publicly Accessible Penn Dissertations 2015 Identifying RNA-Protein Interaction Sites Throughout Eukaryotic Transcriptomes Ian M. Silverman University of Pennsylvania, [email protected] Follow this and additional works at: https://repository.upenn.edu/edissertations Part of the Bioinformatics Commons, Biology Commons, and the Genetics Commons Recommended Citation Silverman, Ian M., "Identifying RNA-Protein Interaction Sites Throughout Eukaryotic Transcriptomes" (2015). Publicly Accessible Penn Dissertations. 2016. https://repository.upenn.edu/edissertations/2016 This paper is posted at ScholarlyCommons. https://repository.upenn.edu/edissertations/2016 For more information, please contact [email protected]. Identifying RNA-Protein Interaction Sites Throughout Eukaryotic Transcriptomes Abstract Gene expression is regulated at both the transcriptional and post-transcriptional levels. While transcription controls only the rate of RNA production, numerous and diverse mechanisms regulate the processing, stability and translation of RNAs at the post-transcriptional level. At the heart of this regulation are RNA-binding proteins (RBPs) and their RNA targets. Thousands of RBPs are encoded in mammalian genomes, each with hundreds to thousands of RNA targets. Therefore, cataloging these interactions represents a significant challenge. Recent advances in high-throughput sequencing technologies have greatly expanded the toolkit that researchers have to probe RNA-protein interactions, but these technologies are still in their infancy and thus new methods and applications are required to move our understanding forward. We developed a novel, high-throughput approach to globally identify regions of RNAs that interact with proteins throughout a transcriptome of interest. We applied this technique to human HeLa cells and provide evidence that our approach captures both known and novel RNA-protein interaction sites. -

Inflammatory Bowel Disease
LINKÖPING UNIVERSITY MEDICAL DISSERTIONS No. 1231 Interindividual differences in thiopurine metabolism - studies with focus on inflammatory bowel disease Sofie Haglund Division of Gastroenterology and Hepatology Department of Clinical and Experimental Medicine Faculty of Health Sciences, Linköping University SE-581 85 Linköping, Sweden Linköping 2011 Sofie Haglund, 2011 Published articles and figures have been reprinted with the permission of the copyright holders: Paper I. © American Association for Clinical Chemistry. Paper II. © John Wiley and Sons. Paper III. © Wolters Kluwer Health. Figure 4. © Wolters Kluwer Health. Figure 6. © QIAGEN. All rights reserved. www.qiagen.com. Figure 7. © Copyright 2006 Life Technologies Corporation. All rights reserved. www.lifetechnologies.com. None of the entities identified support or endorse or accept liability in any way for the information that is used or the manner in which it is used. Figure 9. © Elsevier. Printed in Sweden by LiU-Tryck, Linköping, Sweden, 2011 ISBN 978-91-7393-213-4 ISSN 0345-0082 I see trees of green, red roses too see them bloom for me and you And I say to myself - What wonderful world I see skies of blue and clouds of white Bright sunny days, dark sacred nights And I think to myself - What a wonderful world Louis Armstrong Talent wins games, but teamwork and intelligence win championships Michael Jordan Contents CONTENTS ABSTRACT ...................................................................................................................1 POPULÄRVETENSKAPLIG SAMMANFATTNING -
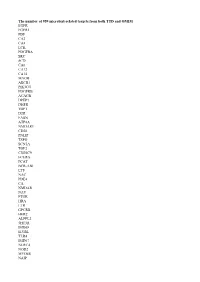
The Number of 959 Microbial-Related Targets from Both TTD and OMIM
The number of 959 microbial-related targets from both TTD and OMIM EGFR FGFR1 PDF CA2 CA4 LCK PDGFRA SRC SCD CA6 CA12 CA14 MAOB ABCB1 PIK3CG PDGFRB ACACB DPEP1 DHFR TOP1 D2R FASN ATP4A NMDAR1 CD20 PNLIP TSPO SCN5A TOP2 CYP2C9 FCERG PCAT BCR-ABI LTF NAC PDE4 CA NMDAR NAV PTGR HRA LTR GPCRB HER2 ALPPL2 5HT3R IMD68 ILVBL TLR4 IMD67 NLRC4 NOD2 MYD88 NAIP TLR2 NOD1 CF CASP1 ATG16L1 LAD TLR5 IL22 TLR9 LCN2 CFTR NLRP3 NFKB1 CAMP IMD51 IL17A IRAK4 TLR1 HIES1 HPS2 FPR1 HSD11B1 CASP4 PGLYRP1 STK4 IL17RA HECTD3 IBD1 EDAID1 CGDX SCN3 IBD10 LAD3 CFDD MVP1 C8A RAB1 IFNG ITGB2 SCARB1 MMP12 IRF8 IKBKB HIF1A IKBKG PGLYRP3 PGLYRP4 CASP12 XLA IMD50 IMD41 CVID1 IMD13 IMD23 IMD71 IMD64 CTNNB1 MMP9 LBP ELANE CXCR1 CD14 MET TNFRSF1A AHR DEFA5 ASNA1 NR1H3 FADD SCN10A IRAK3 HTRA2 IFNLR1 IRGM NEIL1 NEIL3 REG3G DOCK8 PFITS HMD CELIAC1 GSD1B ICAS SCNX SCIDX1 IMD47 HIGM2 HIGM3 SCN4 CVID3 IMD31C TIIAC IMD40 RFMN CVID13 MIRAGE HIES3 HIES4 SCN8 IMD66 IMD70 LPRS1 DNMT1 CX3CR1 TREM1 CFD SLC2A2 IL1B CBL PRKCE TF GARS1 DUSP1 SEPHS1 DJ1 RUVBL1 RIPK1 RIPK2 TRADD PADI4 IL27RA IL23A LGALS8 IL17F GFM2 ALPK1 MEFV NEIL2 DPH3 CEACAM3 NLRP6 PLEKHF1 ACOD1 INAVA DAR KIDAD VP C2D CGD4 CGD1 MKS1 PKU CDG2C CDG2F IMD61 IMD33 HIGM1 HIGM5 CRIE C5D CFHD EDAID2 IBD13 AGM6 LPRS5 AGM2 C1QD C3D CGD3 LEPD SCN5 IMD12 IMD15B IMD17 IMD19 IMD24 IMD36 SCN6 IMD55 PRAAS2 IMD57 IMD58 IMD72 T1D NAD CELIAC13 STAT3 CD44 IFNAR1 ART4 BMP5 CEACAM5 CLCN1 COL1A2 MLH1 S100A8 S100A9 IL10 DRD4 NCF4 SMO ATF3 NEDD8 COCH MTRNR1 ENG PDYN NR3C1 GFPT1 HOXB8 LYZ LAMA2 MPG MUC5AC IL12B NOS2 LEP AKT1 SPP1 PTAFR CD36 PTGER1 -

Expression Und Funktion Von Gαi-Proteinen in Entzündungszellen
Aus dem Department für Experimentelle und Klinische Pharmakologie und Toxikologie der Universität Tübingen Abteilung für Pharmakologie und Experimentelle Therapie Direktor: Professor Dr. Dr. B. Nürnberg Expression und Funktion von Gαi-Proteinen in Entzündungszellen Inaugural-Dissertation zur Erlangung des Doktorgrades der Medizin der Medizinischen Fakultät der Eberhard Karls Universität zu Tübingen vorgelegt von Ana Novakovic aus Skopje / Mazedonien 2013 Dekan: Professor Dr. I. B. Autenrieth 1. Berichterstatter: Professor Dr. Dr. B. Nürnberg 2. Berichterstatter: Professor Dr. D. Hartl Inhalt Inhalt 1 Einleitung ................................................................................................. 1 1.1 Allgemeine Prinzipien der zellulären Signaltransduktion ........................... 1 1.2 G-Protein-abhängige Signaltransduktion ................................................... 3 1.2.1 Struktur und Funktion von G-Proteinen ..................................................... 3 1.2.2 Gα-Untereinheiten ..................................................................................... 5 1.2.3 G-Untereinheiten .................................................................................... 6 1.2.4 Gαi-Familie ................................................................................................ 7 1.3 Das angeborene Immunsystem ................................................................. 8 1.3.1 Chemotaxis von Entzündungszellen am Beispiel der Migration neutrophiler Granulozyten ........................................................................ -

Emerging Mechanisms in Initiating and Terminating Autophagy Manuela Antonioli,1,2 Martina Di Rienzo,1,3 Mauro Piacentini,1,3 and Gian Maria Fimia1,4,*
TIBS 1309 No. of Pages 14 Review Emerging Mechanisms in Initiating and Terminating Autophagy Manuela Antonioli,1,2 Martina Di Rienzo,1,3 Mauro Piacentini,1,3 and Gian Maria Fimia1,4,* Autophagy is a major degradative process activated in a rapid and transient Trends manner to cope with stress conditions. Whether autophagy is beneficial or Autophagy is a catabolic process detrimental depends upon the rate of induction and the appropriateness of essential for the basal turnover of cel- the duration. Alterations in both autophagy initiation and termination predis- lular components. In response to pose the cell to death, and affect the execution of other inducible processes stress stimuli, autophagy is rapidly induced to ensure the restoration of such as inflammation. In this review we discuss how stress signaling path- cellular homeostasis. The duration of ways dynamically control the activity of the autophagy machinery by mediat- autophagy response is also tightly fi regulated to avoid uncontrolled cell ing post-translational modi cations and regulatory protein interactions. In digestion. particular, we highlight the emerging role of TRIM and CULLIN families of ubiquitin ligases which play opposite roles in the autophagy response by Autophagy is mainly regulated at the post-translational level. Phosphoryla- promoting or inhibiting, respectively, the activity of the autophagy initiation tion and ubiquitination are the best- complex. characterized post-translational modi- fications responsible for the regulation of the autophagy core machinery -

Interferon-Gamma (IFN-Γ): Exploring Its Implications in Infectious Diseases
BioMol Concepts 2018; 9: 64–79 Review Open Access Gunjan Kak*#, Mohsin Raza#, Brijendra K Tiwari Interferon-gamma (IFN-γ): Exploring its implications in infectious diseases Journal xyz 2017; 1 (2): 122–135 https://doi.org/10.1515/bmc-2018-0007 of disease mechanisms and these aspects also manifest received February 13, 2018; accepted April 20, 2018.1 The First Decade (1964-1972) enormous therapeutic importance for the annulment of Abstract: A key player in driving cellular immunity, IFN-γ various infections and autoimmune conditions. Researchis capable Article of orchestrating numerous protective functions to heighten immune responses in infections and cancers. Keywords: Cytokine; IFN-γ; Immune Response; Infectious MaxIt Musterman, can exhibit its immunomodulatoryPaul Placeholder effects by enhancing Diseases; Mycobacteria; Host-pathogen interaction; antigen processing and presentation, increasing leukocyte Cytokine therapy. Whattrafficking, Is So inducing Different an anti-viral About state, boosting the anti- Neuroenhancement?microbial functions and affecting cellular proliferation and apoptosis. A complex interplay between immune IFN-γ: An Introduction Wascell ist activity so and anders IFN-γ through am coordinatedNeuroenhancement? integration of signals from other pathways involving cytokines The human immune system is evolved to eradicate or Pharmacologicaland Pattern Recognition and Mental Receptors Self-transformation (PRRs) such as in containEthic any pathogenic challenge and eliminate self- ComparisonInterleukin (IL)-4, TNF-α, Lipopolysaccharide (LPS), altered cancerous cells. In this regard, IFN-γ has a critical PharmakologischeType-I Interferons und(IFNs) mentale etc. leads Selbstveränderung to initiation of a imrole in recognizing and eliminating pathogens. IFN-γ, cascade of pro-inflammatory responses. Microarray data being the central effector of cell mediated immunity, can ethischen Vergleich has unraveled numerous genes whose transcriptional coordinate a plethora of anti-microbial functions.