Gastric Digestive Function
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

De Novo Phosphatidylcholine Synthesis in Intestinal Lipid Metabolism and Disease
De Novo Phosphatidylcholine Synthesis in Intestinal Lipid Metabolism and Disease by John Paul Kennelly A thesis submitted in partial fulfillment of the requirements for the degree of Doctor of Philosophy in Nutrition and Metabolism Department of Agricultural, Food and Nutritional Science University of Alberta © John Paul Kennelly, 2018 Abstract Phosphatidylcholine (PC), the most abundant phospholipid in eukaryotic cells, is an important component of cellular membranes and lipoprotein particles. The enzyme CTP: phosphocholine cytidylyltransferase (CT) regulates de novo PC synthesis in response to changes in membrane lipid composition in all nucleated mammalian cells. The aim of this thesis was to determine the role that CTα plays in metabolic function and immune function in the murine intestinal epithelium. Mice with intestinal epithelial cell-specific deletion of CTα (CTαIKO mice) were generated. When fed a chow diet, CTαIKO mice showed normal lipid absorption after an oil gavage despite a ~30% decrease in small intestinal PC concentrations relative to control mice. These data suggest that biliary PC can fully support chylomicron output under these conditions. However, when acutely fed a high-fat diet, CTαIKO mice showed impaired intestinal fatty acid and cholesterol uptake from the intestinal lumen into enterocytes, resulting in lower postprandial plasma triglyceride concentrations. Impaired intestinal fatty acid uptake in CTαIKO mice was linked to disruption of intestinal membrane lipid transporters (Cd36, Slc27a4 and Npc1l1) and higher postprandial plasma Glucagon-like Peptide 1 and Peptide YY. Unexpectedly, there was a shift in expression of bile acid transporters to the proximal small intestine of CTαIKO mice, which was associated with enhanced biliary bile acid, PC and cholesterol output relative to control mice. -

The Metabolic Serine Hydrolases and Their Functions in Mammalian Physiology and Disease Jonathan Z
REVIEW pubs.acs.org/CR The Metabolic Serine Hydrolases and Their Functions in Mammalian Physiology and Disease Jonathan Z. Long* and Benjamin F. Cravatt* The Skaggs Institute for Chemical Biology and Department of Chemical Physiology, The Scripps Research Institute, 10550 North Torrey Pines Road, La Jolla, California 92037, United States CONTENTS 2.4. Other Phospholipases 6034 1. Introduction 6023 2.4.1. LIPG (Endothelial Lipase) 6034 2. Small-Molecule Hydrolases 6023 2.4.2. PLA1A (Phosphatidylserine-Specific 2.1. Intracellular Neutral Lipases 6023 PLA1) 6035 2.1.1. LIPE (Hormone-Sensitive Lipase) 6024 2.4.3. LIPH and LIPI (Phosphatidic Acid-Specific 2.1.2. PNPLA2 (Adipose Triglyceride Lipase) 6024 PLA1R and β) 6035 2.1.3. MGLL (Monoacylglycerol Lipase) 6025 2.4.4. PLB1 (Phospholipase B) 6035 2.1.4. DAGLA and DAGLB (Diacylglycerol Lipase 2.4.5. DDHD1 and DDHD2 (DDHD Domain R and β) 6026 Containing 1 and 2) 6035 2.1.5. CES3 (Carboxylesterase 3) 6026 2.4.6. ABHD4 (Alpha/Beta Hydrolase Domain 2.1.6. AADACL1 (Arylacetamide Deacetylase-like 1) 6026 Containing 4) 6036 2.1.7. ABHD6 (Alpha/Beta Hydrolase Domain 2.5. Small-Molecule Amidases 6036 Containing 6) 6027 2.5.1. FAAH and FAAH2 (Fatty Acid Amide 2.1.8. ABHD12 (Alpha/Beta Hydrolase Domain Hydrolase and FAAH2) 6036 Containing 12) 6027 2.5.2. AFMID (Arylformamidase) 6037 2.2. Extracellular Neutral Lipases 6027 2.6. Acyl-CoA Hydrolases 6037 2.2.1. PNLIP (Pancreatic Lipase) 6028 2.6.1. FASN (Fatty Acid Synthase) 6037 2.2.2. PNLIPRP1 and PNLIPR2 (Pancreatic 2.6.2. -

Biogenesis of Lipid Bodies in Lobosphaera Incisa
Biogenesis of Lipid Bodies in Lobosphaera incisa Dissertation for the award of the degree “Doctor rerum naturalium” of the Georg-August-Universität Göttingen within the doctoral program GGNB Microbiology and Biochemistry of the Georg-August University School of Science (GAUSS) submitted by Heike Siegler from Münster Göttingen 2016 Members of the Thesis Committee Prof. Dr. Ivo Feußner Department for Plant Biochemistry, Albrecht-von-Haller Institute for Plant Sciences, University of Göttingen Prof. Dr. Volker Lipka Department of Plant Cell Biology, Albrecht-von-Haller Institute for Plant Sciences, University of Göttingen Prof. Dr. Thomas Friedl Department of Experimental Phycology and Culture Collection of Algae at the University of Göttingen, Albrecht-von-Haller Institute for Plant Sciences, University of Göttingen Members of the Examination Board Prof. Dr. Ivo Feußner (Referee) Department for Plant Biochemistry, Albrecht-von-Haller Institute for Plant Sciences, University of Göttingen Prof. Dr. Volker Lipka (2nd Referee) Department of Plant Cell Biology, Albrecht-von-Haller Institute for Plant Sciences, University of Göttingen Prof. Dr. Thomas Friedl Department of Experimental Phycology and Culture Collection of Algae at the University of Göttingen, Albrecht-von-Haller Institute for Plant Sciences, University of Göttingen Prof. Dr. Andrea Polle Department of Forest Botany and Tree Physiology, Büsgen Institute, University of Göttingen PD Dr. Thomas Teichmann Department of Plant Cell Biology, Albrecht-von-Haller Institute for Plant Sciences, University of Göttingen Dr. Martin Fulda Department for Plant Biochemistry, Albrecht-von-Haller Institute for Plant Sciences, University of Göttingen Date of oral examination: 30.05.2016 Affidavit I hereby declare that I wrote the present dissertation on my own and with no other sources and aids than quoted. -

Aandp2ch25lecture.Pdf
Chapter 25 Lecture Outline See separate PowerPoint slides for all figures and tables pre- inserted into PowerPoint without notes. Copyright © McGraw-Hill Education. Permission required for reproduction or display. 1 Introduction • Most nutrients we eat cannot be used in existing form – Must be broken down into smaller components before body can make use of them • Digestive system—acts as a disassembly line – To break down nutrients into forms that can be used by the body – To absorb them so they can be distributed to the tissues • Gastroenterology—the study of the digestive tract and the diagnosis and treatment of its disorders 25-2 General Anatomy and Digestive Processes • Expected Learning Outcomes – List the functions and major physiological processes of the digestive system. – Distinguish between mechanical and chemical digestion. – Describe the basic chemical process underlying all chemical digestion, and name the major substrates and products of this process. 25-3 General Anatomy and Digestive Processes (Continued) – List the regions of the digestive tract and the accessory organs of the digestive system. – Identify the layers of the digestive tract and describe its relationship to the peritoneum. – Describe the general neural and chemical controls over digestive function. 25-4 Digestive Function • Digestive system—organ system that processes food, extracts nutrients, and eliminates residue • Five stages of digestion – Ingestion: selective intake of food – Digestion: mechanical and chemical breakdown of food into a form usable by -

Regulation of ATP-Binding Cassette Transporter Al in Cholesteryl Ester Storage Disease
Regulation of ATP-Binding Cassette Transporter Al In Cholesteryl Ester Storage Disease by NICOLAS JAMES BILBEY B.Sc (Honours), Thompson Rivers University, 2006 A THESIS SUBMiTTED IN PARTIAL FULFILLMENT OF THE REQUIREMENTS FOR THE DEGREE OF MASTER OF SCIENCE in THE FACULTY OF GRADUATE STUDIES (Experimental Medicine) THE UNIVERSITY OF BRITISH COLUMBIA (Vancouver) June 2009 © Nicolas James Bilbey, 2009 ABSTRACT Previous studies from the Francis laboratory have determined that regulation of ABCA1 expression is impaired in the lysosomal cholesterol storage disorder Niemann-Pick type C (NPC) disease, the presumed reason for the low plasma HDL-cholesterol (HDL-C) levels found in the majority of NPC disease patients. Cholesteryl ester storage disease (CESD) is another lysosomal cholesterol storage disorder, resulting from deficiency in lysosomal acid lipase (LAL). CESD patients develop premature atherosclerosis, possibly related to their known low plasma HDL-C levels. We hypothesized that in CESD the reduced activity of LAL also leads to impaired ABCA1 regulation and HDL formation due to the decrease in release of unesterified cholesterol from lysosomes. Our results show that human CESD fibroblasts exhibit a blunted increase in ABCA1 mRNA and protein in response to addition of low density lipoprotein (LDL) to the medium when compared to normal human fibroblasts. Efflux of LDL-derived cholesterol radiolabel and mass to apolipoprotein A-I-containing medium was markedly reduced in CESD fibroblasts compared to normal fibroblasts. Cellular radiolabeled cholesteryl ester derived from LDL and total cell cholesteryl ester mass was increased in CESD compared to normal cells. Delivery of an adenovirus expressing full length human lysosomal acid lipase (Ad-hLAL) results in correction of LAL activity and an increase ABCA1 protein expression, as well as correction of cholesterol and phospholipid release to apoA-I and normalization of cholesteryl ester levels in the CESD fibroblasts. -
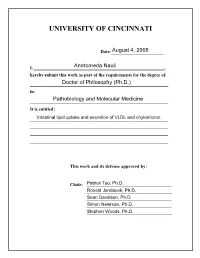
University of Cincinnati
UNIVERSITY OF CINCINNATI Date:___________________ I, _________________________________________________________, hereby submit this work as part of the requirements for the degree of: in: It is entitled: This work and its defense approved by: Chair: _______________________________ _______________________________ _______________________________ _______________________________ _______________________________ ii Intestinal lipid uptake and secretion of VLDL and chylomicron By: Andromeda Nauli August 2005 Previous degree: Bachelor of Science in Biomedical Sciences Degree to be conferred: Ph.D. Department of Pathology and Laboratory Medicine College of Medicine University of Cincinnati Committee chair: Patrick Tso, Ph.D. iii ABSTRACT Despite decades of research, our understanding of intestinal lipid absorption is limited. In this Ph.D. thesis, I have dealt with two main aspects of intestinal lipid absorption, namely the uptake of lipids and the formation and secretion of triacylglycerol-rich lipoproteins (very low density lipoproteins [VLDL] and chylomicrons). In terms of uptake, CD36 is one of the plasma membrane proteins implicated in mediating lipid uptake by the intestine. In order to test this hypothesis, we utilized the CD36 knockout mouse model equipped with intraduodenal and lymph cannulas. Our studies showed that the disruption of the CD36 gene led to a significant decrease in the uptake of cholesterol but not of fatty acids. Interestingly, the role of CD36 was not limited to uptake but also appeared to affect the formation and secretion of chylomicrons, the major lipoproteins carrying the absorbed dietary fat from the gut (Chapter 2). It was first proposed by Tso et al. (202) that the small intestine secretes both VLDL and chylomicrons. Previous work by Vahouny et al. (212) suggested that female rats produced more VLDL than male rats. -

WO 2015/048577 A2 April 2015 (02.04.2015) W P O P C T
(12) INTERNATIONAL APPLICATION PUBLISHED UNDER THE PATENT COOPERATION TREATY (PCT) (19) World Intellectual Property Organization International Bureau (10) International Publication Number (43) International Publication Date WO 2015/048577 A2 April 2015 (02.04.2015) W P O P C T (51) International Patent Classification: (81) Designated States (unless otherwise indicated, for every A61K 48/00 (2006.01) kind of national protection available): AE, AG, AL, AM, AO, AT, AU, AZ, BA, BB, BG, BH, BN, BR, BW, BY, (21) International Application Number: BZ, CA, CH, CL, CN, CO, CR, CU, CZ, DE, DK, DM, PCT/US20 14/057905 DO, DZ, EC, EE, EG, ES, FI, GB, GD, GE, GH, GM, GT, (22) International Filing Date: HN, HR, HU, ID, IL, IN, IR, IS, JP, KE, KG, KN, KP, KR, 26 September 2014 (26.09.2014) KZ, LA, LC, LK, LR, LS, LU, LY, MA, MD, ME, MG, MK, MN, MW, MX, MY, MZ, NA, NG, NI, NO, NZ, OM, (25) Filing Language: English PA, PE, PG, PH, PL, PT, QA, RO, RS, RU, RW, SA, SC, (26) Publication Language: English SD, SE, SG, SK, SL, SM, ST, SV, SY, TH, TJ, TM, TN, TR, TT, TZ, UA, UG, US, UZ, VC, VN, ZA, ZM, ZW. (30) Priority Data: 61/883,925 27 September 2013 (27.09.2013) US (84) Designated States (unless otherwise indicated, for every 61/898,043 31 October 2013 (3 1. 10.2013) US kind of regional protection available): ARIPO (BW, GH, GM, KE, LR, LS, MW, MZ, NA, RW, SD, SL, ST, SZ, (71) Applicant: EDITAS MEDICINE, INC. -

Fat Digestion: Intestinal Lipolysis and Product Absorption
Nutrition of the Lov: Birthweight Infant, edited by B. L. Salle and P. R. Swyer. Nestte Nutrition Workshop Series, Vol. 32. Nestec Ltd., Vevey/Raven Press, Ltd., New York © 1993. Fat Digestion: Intestinal Lipolysis and Product Absorption Lars Blackberg and *Olle Hernell Department of Medical Biochemistry and Biophysics, and 'Department of Pediatrics, University of Umea, S-901 85 Umea, Sweden Fat digestion in the breastfed newborn infant is a process catalyzed by three Upases. The process is initiated in stomach contents by gastric lipase and continues in the upper part of the small intestine by pancreatic colipase-dependent lipase and human milk bile-salt-stimulated lipase (BSSL). Development of powerful techniques in molecular biology has made it possible to gain better insight into the structure of these lipases, which is necessary for a detailed understanding of the different functional aspects. We shall briefly discuss recent advances in structural knowledge of the lipases as well as their functional implica- tions. We shall focus mainly on the human enzymes but, when relevant, also discuss corresponding enzymes of other species. GASTRIC LIPASE Gastric lipolysis and lipase activities of preduodenal origin have been recognized for many years. In humans the responsible enzyme is secreted by the chief cells of the gastric mucosa (1). The primary sequence of this 52-kDa glycoprotein is known through cloning and sequencing of cDNA (2). The tissue of origin differs between species but the amino acid sequence is highly conserved (2-5). Although, gastric lipase is of similar molecular size to colipase-dependent lipase the sequence shows only limited homology. -

(12) Patent Application Publication (10) Pub. No.: US 2003/0198970 A1 Roberts (43) Pub
US 2003O19897OA1 (19) United States (12) Patent Application Publication (10) Pub. No.: US 2003/0198970 A1 Roberts (43) Pub. Date: Oct. 23, 2003 (54) GENOSTICS clinical trials on groups or cohorts of patients. This group data is used to derive a Standardised method of treatment (75) Inventor: Gareth Wyn Roberts, Cambs (GB) which is Subsequently applied on an individual basis. There is considerable evidence that a significant factor underlying Correspondence Address: the individual variability in response to disease, therapy and FINNEGAN, HENDERSON, FARABOW, prognosis lies in a person's genetic make-up. There have GARRETT & DUNNER been numerous examples relating that polymorphisms LLP within a given gene can alter the functionality of the protein 1300 ISTREET, NW encoded by that gene thus leading to a variable physiological WASHINGTON, DC 20005 (US) response. In order to bring about the integration of genomics into medical practice and enable design and building of a (73) Assignee: GENOSTIC PHARMA LIMITED technology platform which will enable the everyday practice (21) Appl. No.: 10/206,568 of molecular medicine a way must be invented for the DNA Sequence data to be aligned with the identification of genes (22) Filed: Jul. 29, 2002 central to the induction, development, progression and out come of disease or physiological States of interest. Accord Related U.S. Application Data ing to the invention, the number of genes and their configu rations (mutations and polymorphisms) needed to be (63) Continuation of application No. 09/325,123, filed on identified in order to provide critical clinical information Jun. 3, 1999, now abandoned. concerning individual prognosis is considerably less than the 100,000 thought to comprise the human genome. -

A Systematic Review on Self-Micro Emulsifying Drug Delivery Systems: a Potential Strategy for Drugs with Poor Oral Bioavailability
International Journal of Applied Pharmaceutics ISSN- 0975-7058 Vol 11, Issue 1, 2019 Review Article A SYSTEMATIC REVIEW ON SELF-MICRO EMULSIFYING DRUG DELIVERY SYSTEMS: A POTENTIAL STRATEGY FOR DRUGS WITH POOR ORAL BIOAVAILABILITY G. V. RADHA1*, K. TRIDEVA SASTRI1, SADHANA BURADA1, JAMPALA RAJKUMAR1 1GITAM Institute of Pharmacy, GITAM Deemed to be University, Rushikonda, Visakhapatnam, Andhra Pradesh State, India Email: [email protected] Received: 26 Sep 2018, Revised and Accepted: 19 Nov 2018 ABSTRACT Currently a marked interest in developing lipid-based formulations to deliver lipophilic compounds. Self-emulsifying system has emerged as a dynamic strategy for delivering poorly water-soluble compounds. These systems can embrace a wide variety of oils, surfactants, and co-solvents. An immediate fine emulsion is obtained on exposure to water/gastro-intestinal fluids. The principal interest is to develop a robust formula for biopharmaceutical challenging drug molecules. Starting with a brief classification system, this review signifies diverse mechanisms concerning lipid- based excipients besides their role in influencing bioavailability, furthermore pertaining to their structured formulation aspects. Consecutive steps are vital in developing lipid-based systems for biopharmaceutical challenging actives. Such a crucial structured development is critical for achieving an optimum formula. Hence lipid excipients are initially scrutinized for their solubility and phase behavior, along with biological effects. Blends are screened by means of simple dilution test and are consequently studied with more advanced biopharmaceutical tests. After discerning of the principle formula, diverse technologies are offered to incorporate the fill-mass either in soft/hard gelatin capsules. There is also feasibility to formulated lipid-system as a solid dosage form. -

299 INTESTINAL LIPID ABSORPTION and TRANSPORT Cam T. Phan
[Frontiers in Bioscience 6, d299-319, March 1, 2001] INTESTINAL LIPID ABSORPTION AND TRANSPORT Cam T. Phan and Patrick Tso Department of Pathology, University of Cincinnati Medical Center, 231 Albert Sabin Way, Cincinnati, OH 45267 TABLE OF CONTENTS 1. Abstract 2. Introduction 3. Dietary lipids 4. Structured lipids 5. Digestion of dietary lipids and structured lipids 5.1. Gastric lumen 5.2. Intestinal lumen 5.3. Digestion of phospholipid 5.4. Digestion of cholesteryl ester 6. Uptake of dietary lipids by enterocytes 6.1. Importance of micellar solubilization 6.2. Importance of unilamellar vesicles 6.3. Uptake of fat digestion products by enterocytes 7. Resynthesis of triglycerides and formation of chylomicrons 7.1. Monoglycerides and fatty acid 7.2. Phospholipids 7.3. Cholesterol 8. Assembly of intestinal lipoproteins 9. Clinical disorders of intestinal lipid transport 10. Acknowledgements 11. References 1. ABSTRACT The purpose of this review is to update the reader lacks the key lipid reesterification enzymes. Finally, the on our current knowledge of the digestion, uptake, and mechanisms of the formation and secretion of chylomicrons is transport of dietary lipid. In particular, it discusses how described and clinical disorders discussed. intestinal lipid transporters may play a role in the uptake of lipids by the enterocytes, and how chylomicrons are formed in 2. INTRODUCTION the enterocytes and packaged for export into the lymphatic system through exocytosis. The classification and properties Many past reviews have been written on the of lipids is first described followed by a discussion of digestion and absorption of lipid and the formation of structured lipids and their role in human nutrition. -

Regional Heterogeneity Impacts Gene Expression in the Subarctic Zooplankter Neocalanus flemingeri in the Northern Gulf of Alaska
ARTICLE https://doi.org/10.1038/s42003-019-0565-5 OPEN Regional heterogeneity impacts gene expression in the subarctic zooplankter Neocalanus flemingeri in the northern Gulf of Alaska Vittoria Roncalli 1,2, Matthew C. Cieslak1, Martina Germano1, Russell R. Hopcroft3 & Petra H. Lenz1 1234567890():,; Marine pelagic species are being increasingly challenged by environmental change. Their ability to persist will depend on their capacity for physiological acclimatization. Little is known about limits of physiological plasticity in key species at the base of the food web. Here we investigate the capacity for acclimatization in the copepod Neocalanus flemingeri, which inhabits the Gulf of Alaska, a heterogeneous and highly seasonal environment. RNA-Seq analysis of field-collected pre-adults identified large regional differences in expression of genes involved in metabolic and developmental processes and response to stressors. We found that lipid synthesis genes were up-regulated in individuals from Prince William Sound and down-regulated in the Gulf of Alaska. Up-regulation of lipid catabolic genes in offshore individuals suggests they are experiencing nutritional deficits. The expression differences demonstrate physiological plasticity in response to a steep gradient in food availability. Our transcriptional analysis reveals mechanisms of acclimatization that likely contribute to the observed resilience of this population. 1 Pacific Biosciences Research Center, University of Hawai’iatMānoa, 1993 East-West Rd., Honolulu, HI 96822, USA. 2 Department of Genetics, Microbiology and Statistics, Facultat de Biologia, IRBio, Universitat de Barcelona, Av. Diagonal 643, 08028 Barcelona, Spain. 3 Institute of Marine Science, University of Alaska, Fairbanks, 120 O’Neill, Fairbanks, AK 99775-7220, USA. Correspondence and requests for materials should be addressed to V.R.