Regulation of ATP-Binding Cassette Transporter Al in Cholesteryl Ester Storage Disease
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

De Novo Phosphatidylcholine Synthesis in Intestinal Lipid Metabolism and Disease
De Novo Phosphatidylcholine Synthesis in Intestinal Lipid Metabolism and Disease by John Paul Kennelly A thesis submitted in partial fulfillment of the requirements for the degree of Doctor of Philosophy in Nutrition and Metabolism Department of Agricultural, Food and Nutritional Science University of Alberta © John Paul Kennelly, 2018 Abstract Phosphatidylcholine (PC), the most abundant phospholipid in eukaryotic cells, is an important component of cellular membranes and lipoprotein particles. The enzyme CTP: phosphocholine cytidylyltransferase (CT) regulates de novo PC synthesis in response to changes in membrane lipid composition in all nucleated mammalian cells. The aim of this thesis was to determine the role that CTα plays in metabolic function and immune function in the murine intestinal epithelium. Mice with intestinal epithelial cell-specific deletion of CTα (CTαIKO mice) were generated. When fed a chow diet, CTαIKO mice showed normal lipid absorption after an oil gavage despite a ~30% decrease in small intestinal PC concentrations relative to control mice. These data suggest that biliary PC can fully support chylomicron output under these conditions. However, when acutely fed a high-fat diet, CTαIKO mice showed impaired intestinal fatty acid and cholesterol uptake from the intestinal lumen into enterocytes, resulting in lower postprandial plasma triglyceride concentrations. Impaired intestinal fatty acid uptake in CTαIKO mice was linked to disruption of intestinal membrane lipid transporters (Cd36, Slc27a4 and Npc1l1) and higher postprandial plasma Glucagon-like Peptide 1 and Peptide YY. Unexpectedly, there was a shift in expression of bile acid transporters to the proximal small intestine of CTαIKO mice, which was associated with enhanced biliary bile acid, PC and cholesterol output relative to control mice. -

Aandp2ch25lecture.Pdf
Chapter 25 Lecture Outline See separate PowerPoint slides for all figures and tables pre- inserted into PowerPoint without notes. Copyright © McGraw-Hill Education. Permission required for reproduction or display. 1 Introduction • Most nutrients we eat cannot be used in existing form – Must be broken down into smaller components before body can make use of them • Digestive system—acts as a disassembly line – To break down nutrients into forms that can be used by the body – To absorb them so they can be distributed to the tissues • Gastroenterology—the study of the digestive tract and the diagnosis and treatment of its disorders 25-2 General Anatomy and Digestive Processes • Expected Learning Outcomes – List the functions and major physiological processes of the digestive system. – Distinguish between mechanical and chemical digestion. – Describe the basic chemical process underlying all chemical digestion, and name the major substrates and products of this process. 25-3 General Anatomy and Digestive Processes (Continued) – List the regions of the digestive tract and the accessory organs of the digestive system. – Identify the layers of the digestive tract and describe its relationship to the peritoneum. – Describe the general neural and chemical controls over digestive function. 25-4 Digestive Function • Digestive system—organ system that processes food, extracts nutrients, and eliminates residue • Five stages of digestion – Ingestion: selective intake of food – Digestion: mechanical and chemical breakdown of food into a form usable by -
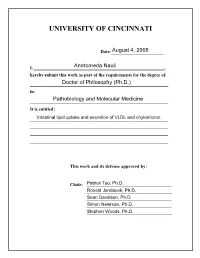
University of Cincinnati
UNIVERSITY OF CINCINNATI Date:___________________ I, _________________________________________________________, hereby submit this work as part of the requirements for the degree of: in: It is entitled: This work and its defense approved by: Chair: _______________________________ _______________________________ _______________________________ _______________________________ _______________________________ ii Intestinal lipid uptake and secretion of VLDL and chylomicron By: Andromeda Nauli August 2005 Previous degree: Bachelor of Science in Biomedical Sciences Degree to be conferred: Ph.D. Department of Pathology and Laboratory Medicine College of Medicine University of Cincinnati Committee chair: Patrick Tso, Ph.D. iii ABSTRACT Despite decades of research, our understanding of intestinal lipid absorption is limited. In this Ph.D. thesis, I have dealt with two main aspects of intestinal lipid absorption, namely the uptake of lipids and the formation and secretion of triacylglycerol-rich lipoproteins (very low density lipoproteins [VLDL] and chylomicrons). In terms of uptake, CD36 is one of the plasma membrane proteins implicated in mediating lipid uptake by the intestine. In order to test this hypothesis, we utilized the CD36 knockout mouse model equipped with intraduodenal and lymph cannulas. Our studies showed that the disruption of the CD36 gene led to a significant decrease in the uptake of cholesterol but not of fatty acids. Interestingly, the role of CD36 was not limited to uptake but also appeared to affect the formation and secretion of chylomicrons, the major lipoproteins carrying the absorbed dietary fat from the gut (Chapter 2). It was first proposed by Tso et al. (202) that the small intestine secretes both VLDL and chylomicrons. Previous work by Vahouny et al. (212) suggested that female rats produced more VLDL than male rats. -

Fat Digestion: Intestinal Lipolysis and Product Absorption
Nutrition of the Lov: Birthweight Infant, edited by B. L. Salle and P. R. Swyer. Nestte Nutrition Workshop Series, Vol. 32. Nestec Ltd., Vevey/Raven Press, Ltd., New York © 1993. Fat Digestion: Intestinal Lipolysis and Product Absorption Lars Blackberg and *Olle Hernell Department of Medical Biochemistry and Biophysics, and 'Department of Pediatrics, University of Umea, S-901 85 Umea, Sweden Fat digestion in the breastfed newborn infant is a process catalyzed by three Upases. The process is initiated in stomach contents by gastric lipase and continues in the upper part of the small intestine by pancreatic colipase-dependent lipase and human milk bile-salt-stimulated lipase (BSSL). Development of powerful techniques in molecular biology has made it possible to gain better insight into the structure of these lipases, which is necessary for a detailed understanding of the different functional aspects. We shall briefly discuss recent advances in structural knowledge of the lipases as well as their functional implica- tions. We shall focus mainly on the human enzymes but, when relevant, also discuss corresponding enzymes of other species. GASTRIC LIPASE Gastric lipolysis and lipase activities of preduodenal origin have been recognized for many years. In humans the responsible enzyme is secreted by the chief cells of the gastric mucosa (1). The primary sequence of this 52-kDa glycoprotein is known through cloning and sequencing of cDNA (2). The tissue of origin differs between species but the amino acid sequence is highly conserved (2-5). Although, gastric lipase is of similar molecular size to colipase-dependent lipase the sequence shows only limited homology. -

299 INTESTINAL LIPID ABSORPTION and TRANSPORT Cam T. Phan
[Frontiers in Bioscience 6, d299-319, March 1, 2001] INTESTINAL LIPID ABSORPTION AND TRANSPORT Cam T. Phan and Patrick Tso Department of Pathology, University of Cincinnati Medical Center, 231 Albert Sabin Way, Cincinnati, OH 45267 TABLE OF CONTENTS 1. Abstract 2. Introduction 3. Dietary lipids 4. Structured lipids 5. Digestion of dietary lipids and structured lipids 5.1. Gastric lumen 5.2. Intestinal lumen 5.3. Digestion of phospholipid 5.4. Digestion of cholesteryl ester 6. Uptake of dietary lipids by enterocytes 6.1. Importance of micellar solubilization 6.2. Importance of unilamellar vesicles 6.3. Uptake of fat digestion products by enterocytes 7. Resynthesis of triglycerides and formation of chylomicrons 7.1. Monoglycerides and fatty acid 7.2. Phospholipids 7.3. Cholesterol 8. Assembly of intestinal lipoproteins 9. Clinical disorders of intestinal lipid transport 10. Acknowledgements 11. References 1. ABSTRACT The purpose of this review is to update the reader lacks the key lipid reesterification enzymes. Finally, the on our current knowledge of the digestion, uptake, and mechanisms of the formation and secretion of chylomicrons is transport of dietary lipid. In particular, it discusses how described and clinical disorders discussed. intestinal lipid transporters may play a role in the uptake of lipids by the enterocytes, and how chylomicrons are formed in 2. INTRODUCTION the enterocytes and packaged for export into the lymphatic system through exocytosis. The classification and properties Many past reviews have been written on the of lipids is first described followed by a discussion of digestion and absorption of lipid and the formation of structured lipids and their role in human nutrition. -

Gastric Digestive Function
Gastrointestinal Functions, edited by Edgard E. Delvin and Michael J. Lentze. Nestle Nutrition Workshop Series. Pediatric Program, Vol. 46. Nestec Ltd.. Vevey/Lippincott Williams & Wilkins. Philadelphia © 2001. Gastric Digestive Function Daniel Menard and Jean-Rene Basque Department of Anatomy and Cell Biology, Faculty of Medicine, University of Sherbrooke, Quebec, Canada The gastric epithelium not only has a protective barrier function (against hydro- chloric acid, peptidases, Helicobacter pylori, and so on) and a primary role in epithe- lial restitution (ulcer healing), but it also has specific digestive functions. The gastric mucosa is responsible for the secretion of luminal compounds such as mucus, hydro- chloric acid, pepsinogen, and lipase. One of the main purposes of gastric secretion is the digestion of dietary proteins. This involves the release of different pepsinogens (Pgl-5) by the fundic and antral gastric glands (1). These inactive proenzymes are synthesized and packaged into secretory granules of surface or glandular epithelial cells. Under acidic conditions, these secreted proenzymes are autocatalytically cleaved to generate their active form—pepsins (pepsin, prochymosin, progastricsin)—which are representative members of a group of proteolytic enzymes classified as aspartic proteases (2). In humans, pepsinogen 5 (Pg5), which is specifically synthesized and secreted by zymogenic chief cells, plays a primary role in the initiation of protein digestion and the proteolysis of collagen (the protein component of meat). Although pepsinogen has been a subject of research since the 19th century (3), knowledge acquired over the last decade on the functions of the human stomach has expanded to include a significant role in fat digestion (4). In contrast to pepsin, the presence of a true gastric lipase has been the subject of a long controversy (4). -

Lingual Lipase and Its Role in the Digestion of Dietary Lipid
Lingual Lipase and Its Role in the Digestion of Dietary Lipid MAnGrr HAMOSH and RoBErT 0. Scow From the Section on Endocrinology, Laboratory of Nutrition and Endocrinology, National Institute of Arthritis and Metabolic Diseases, Bethesda, Maryland 20014 A B S T R A C T The serous glands of rat tongue were saliva of calves contains a lipolytic activity, called "pre- found to contain a potent lipolytic enzyme which hydro- gastric esterase," which hydrolyzes triglyceride to FFA lyzed triglyceride to mostly diglyceride and free fatty in the stomach (11). Glandular tissue from the back re- acids (FFA) at pH 4.5-5.4. Homogenates of lingual se- gion of the tongue, the glossoepiglottic area of the rous glands from adult rats hydrolyzed 40-70 mmol of pharynx, and the pharyngeal end of the esophagus also triglyceride/g per h. The soft palate, anterior oral pharyn- contained the activity (12). Therefore, the secretory geal wall, and lateral oral pharyngeal glands also con- tissues of the mouth of suckling and adult rats were ex- tained the activity, but at a much lower level. The lipo- amined for lipolytic activity. This paper describes a po- lytic activity was also found in saliva collected through tent lipase found in the tongue and its possible role in the an esophageal cannula and in stomach contents of rats digestion of triglyceride. fed a fat-rich meal. The stomach contained very little activity, however, when saliva was excluded. Lipolytic METHODS activity was not found in the stomach wall or in the Animals. Adult female (Charles River, Charles River parotid, submandibular, and sublingual glands. -

Enzymes Involved in Lipid Digestion A
Enzymes involved in lipid digestion A. Salhi, F. Carriere, Myriam M.-L. Grundy, A. Aloulou To cite this version: A. Salhi, F. Carriere, Myriam M.-L. Grundy, A. Aloulou. Enzymes involved in lipid digestion. Myriam M.-L. Grundy; Peter J. Wilde. Bioaccessibility and digestibility of lipids from food, Springer Interna- tional Publishing, pp.3-28, 2021, 978-3-030-56908-2. 10.1007/978-3-030-56909-9_1. hal-03146298 HAL Id: hal-03146298 https://hal.archives-ouvertes.fr/hal-03146298 Submitted on 19 Feb 2021 HAL is a multi-disciplinary open access L’archive ouverte pluridisciplinaire HAL, est archive for the deposit and dissemination of sci- destinée au dépôt et à la diffusion de documents entific research documents, whether they are pub- scientifiques de niveau recherche, publiés ou non, lished or not. The documents may come from émanant des établissements d’enseignement et de teaching and research institutions in France or recherche français ou étrangers, des laboratoires abroad, or from public or private research centers. publics ou privés. Preprint of DOI: 10.1007/978-3-030-56909-9_1 Enzymes involved in lipid digestion Salhi, A. a, b , Carriere, F. b, Grundy, M. M.L c, and Aloulou, A. a a Laboratoire de Biochimie et de Genie Enzymatique des Lipases, ENIS, Universite de Sfax, 3038, Sfax, Tunisia b Aix Marseille Univ, CNRS, BIP, UMR7281, 31 Chemin Joseph Aiguier, 13402, Marseille Cedex 9, France c School of Agriculture, Policy and Development, Sustainable Agriculture and Food Systems Division, University of Reading, Earley Gate, Reading, RG6 6AR, UK Lipid digestion is a complex process that takes place at the lipid-water interface and involves various lipolytic enzymes present predominantly in the stomach and the small intestine (Carey, Small, & Bliss, 1983). -

Digestion of Human Milk Fat in Healthy Infants
NUTRITION RESEARCH 83 (2020) 15– 29 Available online at www.sciencedirect.com ScienceDirect www.nrjournal.com Review Article Digestion of human milk fat in healthy infants Xuan He a, b, Shannon M cClorry a, Olle Hernell c, Bo Lönnerdal a, Carolyn M. Slupsky a, b,⁎ a Department of Nutrition, Davis, One Shields Ave, Davis, CA 95616, USA b Department of Food Science and Technology, University of California, Davis, One Shields Ave, Davis, CA 95616, USA c Department of Clinical Sciences, Pediatrics, Umeå University, SE 901 85 Umeå, Sweden ARTICLE INFO ABSTRACT Article history: Lipid digestion is critical for infant development, and yet, the interconnection between lipid Received 17 March 2020 digestion and the microbiota is largely understudied. This review focuses on digestion of the Revised 2 August 2020 human milk fat globule and summarizes the current understanding of the mechanisms Accepted 7 August 2020 underlying this process in infants. We first discuss the partial hydrolysis of milk fat in the stomach, which leads to rearrangement of lipid droplets, creating a lipid-water interface Keywords: necessary for duodenal lipolysis. In the first few months of life, secretion of pancreatic Infant triglyceride lipase, phospholipase A2, and bile salts is immature. The dominant lipases aiding fat Neonate digestion in the newborn small intestine are therefore pancreatic lipase-related protein 2 and Lipid digestion bile salt–stimulated lipase from both the exocrine pancreas and milk. We summarize the Milk fat globule interaction between ionic fatty acids and cations to form insoluble fatty acid soaps and how it is Gut microbiota influenced by various factors, including cation availability, pH, and bile salt concentration, as well as saturation and chain length of fatty acids.Wefurtherarguethattheformationofthe soap complex does not contribute to lipid bioavailability. -
The Functional Role of CD36 Involved in Fatty Acid Transduction
Utah State University DigitalCommons@USU All Graduate Theses and Dissertations Graduate Studies 5-2014 The Functional Role of CD36 Involved in Fatty Acid Transduction Han Xu Utah State University Follow this and additional works at: https://digitalcommons.usu.edu/etd Part of the Biology Commons Recommended Citation Xu, Han, "The Functional Role of CD36 Involved in Fatty Acid Transduction" (2014). All Graduate Theses and Dissertations. 2172. https://digitalcommons.usu.edu/etd/2172 This Dissertation is brought to you for free and open access by the Graduate Studies at DigitalCommons@USU. It has been accepted for inclusion in All Graduate Theses and Dissertations by an authorized administrator of DigitalCommons@USU. For more information, please contact [email protected]. THE FUNCTIONAL ROLE OF CD36 INVOLVED IN FATTY ACID TRANSDUCTION By Han Xu A dissertation submitted in partial fulfillment of the requirements for the degree of DOCTOR OF PHILOSOPHY In Biology Approved: Timothy A. Gilbertson, Ph.D. David A. York, Ph.D. Major Professor Committee Member MieJung Park-York, Ph.D. Michael Lefevre, Ph.D. Committee Member Committee Member Anhong Zhou, Ph.D. Mark R. McLellan, Ph.D. Committee Member Vice President for Research and Dean of the School of Graduate Studies UTAH STATE UNIVERSITY Logan, Utah 2013 ii Copyright © Han Xu 2013 All Rights Reserved iii ABSTRACT The Functional Role of CD36 Involved in Fatty Acid Transduction by Han Xu, Doctor of Philosophy Utah State University, 2013 Major Professor: Dr. Timothy A. Gilbertson Department: Biology The multifunctional fatty acid (FA) binding protein, Cluster of Differentiation 36 (CD36), has been found to be expressed in a variety of tissues where it is involved in multiple fat-related biological processes, such as lipid metabolism in mammals and the detection of lipid-like pheromones in insects. -

Principles of Physiology of Lipid Digestion
282 Principles of Physiology of Lipid Digestion E. Bauer*, S. Jakob1 and R. Mosenthin Institute of Animal Nutrition, University of Hohenheim, Emil-Wolff-Str. 10, 70599 Stuttgart, Germany ABSTRACT : The processing of dietary lipids can be distinguished in several sequential steps, including their emulsification, hydrolysis and micellization, before they are absorbed by the enterocytes. Emulsification of lipids starts in the stomach and is mediated by physical forces and favoured by the partial lipolysis of the dietary lipids due to the activity of gastric lipase. The process of lipid digestion continues in the duodenum where pancreatic triacylglycerol lipase (PTL) releases 50 to 70% of dietary fatty acids. Bile salts at low concentrations stimulate PTL activity, but higher concentrations inhibit PTL activity. Pancreatic triacylglycerol lipase activity is regulated by colipase, that interacts with bile salts and PTL and can release bile salt mediated PTL inhibition. Without colipase, PTL is unable to hydrolyse fatty acids from dietary triacylglycerols, resulting in fat malabsorption with severe consequences on bioavailability of dietary lipids and fat-soluble vitamins. Furthermore, carboxyl ester lipase, a pancreatic enzyme that is bile salt-stimulated and displays wide substrate reactivities, is involved in lipid digestion. The products of lipolysis are removed from the water-oil interface by incorporation into mixed micelles that are formed spontaneously by the interaction of bile salts. Monoacylglycerols and phospholipids enhance the ability of bile salts to form mixed micelles. Formation of mixed micelles is necessary to move the non-polar lipids across the unstirred water layer adjacent to the mucosal cells, thereby facilitating absorption. (Asian-Aust. J. -

Regulation of Lumen Fat Digestion: Enzymic Aspects
Proceedings of the Nutrition Society (1996), 55, 5-18 5 Regulation of lumen fat digestion: enzymic aspects BY ROBERT VERGER, MUSTAPHA AOUBALA, FREDERIC CARRIERE, STEPHANERANSAC, LILIANE DUPUIS, JOSIANE DE CARO, FRANCINE FERRATO, ISABELLE DOUCHET, RENE LAUGIER AND ALAIN DE CARO UPR 9025, Laboratoire de Lipolyse Enzyrnatique, IFRCl du CNRS 31 Chemin Joseph-Aiguier, 13402 Marseille Cedex 20, France Aspects enzymatiques de la digestion intraluminale des lipides RESUME Les triacylglydrols, qui constituent la majeure partie (90 B 95%) de l’alimentation lipidique chez l’homme, subissent dans l’estomac une hydrolyse partielle en diacyl- glycCrols et acides gras sous l’action d’une lipase prCduodCnale (lipase gastrique, linguale ou pharyngienne selon les espckes). Au niveau du duodCnum 1’Cmulsion formCe de triacylglydrols, diacylglydrols et acides gras entre en contact avec les sCcrCtions pancrkatiques et biliaires. Grke B l’action principale de la lipase pancrkatique et a celle de la lipase gastrique, les triacylglycCrols et les diacylglycCroles sont entikrement convertis en monoacylglycCrols et acides gras qui sont absorb& par les cellules de la bordure en brosse intestinale, sous forme de micelles mixtes avec les sels biliaires. Les lipases prdduodknales sont stables et actives en milieu acide. La purification et la caractkrisation des rCsidus d’amino acides essentiels a l’activitk enzymatique (sCrine au site catalytique, et groupe sulfhydryle) ont Cte rCalisCes sur les lipases prCduod6nales. De nombreuses lipases prCduodCnales ont CtC clonCes et une grande homologie dans les sequences a CtC observte. Des anticorps monoclonaux anti-lipase gastrique humaine ont CtC utilisCs d’une part comme marqueurs specifiques des sites fonctionnels et d’autre part pour l’immuno- purification de l’enzyme ainsi que pour la mise au point d’un dosage immunoenzyma- tique de type ELISA qui permet de discriminer entre la lipase pancrkatique et la lipase gastrique presentes dans des prCl6vements duodCnaux.