Value of Syndromic Surveillance in Monitoring a Focal Waterborne
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Oaklands, Harlestone Road, Chapel Brampton, Northamptonshire NN6 8AW
Oaklands, Harlestone Road, Chapel Brampton, Northamptonshire NN6 8AW An attractively positioned The annexe accommodation to the ground floor comprises entrance hall, cloakroom, family home in a sitting/dining room and fitted kitchenette. To desirable village location the first floor there are two bedrooms, store room and a three piece bathroom suite. The Property Features Oaklands is a delightful family home situated • Main hall with cloakroom off to the edge of the popular village of Chapel • Sitting room, office/family room and Brampton with countryside views and a self-contained guest accommodation/annexe. conservatory The property is believed to date to the late • Fitted kitchen/dining room 1970s and is of individual design occupying a • Four principal bedrooms to the main house generous plot. During their time at the • Self-contained two bedroom annexe with property, the owners have carried out a sitting room, kitchenette, bathroom and number of notable improvements, most recently the creation of a good sized refitted dressing area/storage room kitchen/dining room. A principal feature of • Off-road parking the property is an annexe which provides self- • Double garage contained living accommodation and could • Good proportioned gardens and grounds also appeal to someone looking to work from home. About 0.121 of a hectare (0.3 of an acre) The ground floor has a main entrance hall with cloakroom off providing access to an Outside office/family room and sitting room, all with A particular feature of the property is its situation. Oaklands is approached through oak flooring. The kitchen/dining room is approached from the main hall and comprises double electric gates which in turn lead to a a generous range of base and eye level units, good sized frontage providing secure off-road enamel sink unit set to oak work surfaces, parking for a number of vehicles. -

Village Design Statement Walgrave, Northamptonshire Contents
Villiallgea Dgeseig nD Staetesmiegntn Statement Walgrave, NoWratlghraave,mp Northoamnpstohnsihriree Summary This Village Design Statement has been prepared for thirdly, it is intended to be a document which the Parish of Walgrave by a Steering Group made up highlights the many positive features of village life of eighteen parishioners, over a period of some in Northamptonshire and the splendid nature of the fifteen months. local countryside. The Steering Group initiated a survey of the This Village Design Statement has produced a set of buildings of Walgrave, which provides a planning guidelines on the environment, open comprehensive description of every residence in the spaces, buildings, highways, utilities and agriculture. parish. This document, which can be viewed on The residents of Walgrave believe that if these application to the Walgrave Parish Council, has been guidelines are followed in all future development, an indispensable guide to the development of this the consequence will be a village which everyone statement. can be proud to live in, to visit and to enjoy. The Steering Group believes that what has emerged is a concise document which is attractive to several different groups of readers. Firstly, it will be used by professional developers and their agents in any proposals for development they may make; secondly, it is a short history of the village which travels back as far as the Domesday Book and is thus of general Chairman interest to adults and children of the village alike; Walgrave VDS Steering Group. Daventry District Council Planning Department, particularly Karen Britton and Richard Wood. The people of Walgrave represented by the steering group of: - Michael Bailey, Clare Baxter, John Beale, Chris Beattie, Malcolm Campbell, Jennie Holmes, David Knight, Matt Knight, John Lockhart, Simon Mead (chair), Fred Morgan, Tom Parker, Maggie Saxon, Robin Simmons, Norwood Whittle, Alan Wild, Kate Wilson, Ian Wilson. -

Premises, Sites Etc Within 30 Miles of Harrington Museum Used for Military Purposes in the 20Th Century
Premises, Sites etc within 30 miles of Harrington Museum used for Military Purposes in the 20th Century The following listing attempts to identify those premises and sites that were used for military purposes during the 20th Century. The listing is very much a works in progress document so if you are aware of any other sites or premises within 30 miles of Harrington, Northamptonshire, then we would very much appreciate receiving details of them. Similarly if you spot any errors, or have further information on those premises/sites that are listed then we would be pleased to hear from you. Please use the reporting sheets at the end of this document and send or email to the Carpetbagger Aviation Museum, Sunnyvale Farm, Harrington, Northampton, NN6 9PF, [email protected] We hope that you find this document of interest. Village/ Town Name of Location / Address Distance to Period used Use Premises Museum Abthorpe SP 646 464 34.8 km World War 2 ANTI AIRCRAFT SEARCHLIGHT BATTERY Northamptonshire The site of a World War II searchlight battery. The site is known to have had a generator and Nissen huts. It was probably constructed between 1939 and 1945 but the site had been destroyed by the time of the Defence of Britain survey. Ailsworth Manor House Cambridgeshire World War 2 HOME GUARD STORE A Company of the 2nd (Peterborough) Battalion Northamptonshire Home Guard used two rooms and a cellar for a company store at the Manor House at Ailsworth Alconbury RAF Alconbury TL 211 767 44.3 km 1938 - 1995 AIRFIELD Huntingdonshire It was previously named 'RAF Abbots Ripton' from 1938 to 9 September 1942 while under RAF Bomber Command control. -

Exhibition Board 4 NNOR Route 7
Pitsford Modelling indicates that a junction Route through Pitsford here will be most effective in Quarry to avoid reducing traffic through Holcot. Boughton Park Holcot Road A508 Harborough Road Moulton Road Route through Boughton Fair Lane Connection to New Holcot Centre. Work Roundabout on A43 A43 required to replace affected facilities. Crosses Northampton and Lamport Railway, watercourse and HP gas Pitsford Road main, with least impact Brampton Lane on infrastructure Signalised Spectacle Lane Junction with controlled crossing for Chapel Brampton Alternative spur students road connections to Moulton Park Spur B Moulton Boughton Road Church Brampton A5199 Northampton Road Spur A Connection to Boughton Red House Road Moulton Lane A43 Vyse Road Sandy lane Connects to Red Boughton Lane Brampton Lane House Road Roundabout Buckton Fields Current A5076 Red House Road Brampton Heath development Future Round Spinney Golf Centre development A5199 Welford Road A508 Harborough Road Northamptonshire River Nene County Golf Club A5076 Holly Lodge Drive Rugby to Milton Keynes Railway Flood Northamptonshire Transport Plan Wider Schemes for Context Plain Planned dual carriageway North-west Relief Road Kingsthorpe Northampton Northern Orbital Route Grange (Option 7 is based on previous Option 1 from 2016 consultation) Farm Option 7 Option 7 variations for spur to Moulton Park Sections of road to be closed Junction/cross roads/roundabouts Northampton Kings Heath residential development (only one spur road will be chosen, Spur A and Spur B are (Dallington Grange) different options to connect to Moulton Park) NORTHAMPTON NORTHERN ORBITAL ROUTE: Option 7. -

Pitsford News
PITSFORD NEWS August—October 2020 From the Editorial Team… When we committed to producing a Newsletter for August, it’s fair to say that were weren’t expecting to have a lot to put in it. With many places closed and socialising limited to zoom meetings, telephone calls or for those who were lucky enough to be able to get outside, chatting across the road or over garden fences to friends and neighbours, we weren’t really expecting very much to report. Well, as usual Pitsford people have come up trumps! Folk have been working away behind the scenes and our community spirit remains unscathed. This month’s edition seems bigger than ever and is full of achievements, positive news and plans for the future. Our next edition will be in November and we hope to have more news of events and meetings that you can enjoy. Our last edition was only available online and we know that some people are unable to access the internet, so this month we are making a limited number of copies available in the phone box, the Church and the pub. If you know someone who would like a paper copy, please let them know, or even better collect one and pop it through their door. In this issue: 2 All Saint’s Church, Pitsford 12 Foodbank 3 Cub and Scout Groups WI 4 All Saint’s Church progress update 13 Village Hall Fundraising 5 All Saints’ Churchyard Extension Sportsfield and Pavilion 6 Time to get Fitter? 14 Royal British Legion 8 Some thoughts on village life.. -
AA How to Find Us 2017
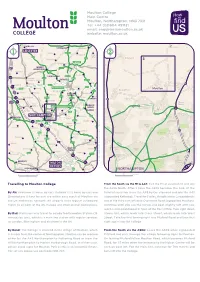
Moulton College Main Centre Moulton, Northampton, NN3 7RR Tel: +44 (0)1604 491131 email: [email protected] website: moulton.ac.uk WIGSTON A47 N UPPINGHAM Duddington N Holcot W E LEICESTER W E Hallaton A6003 2 1 Harringworth King’s S A6 Cliffe S A43 Pitsford Medbourne 3 A 5 CORBY 1 Cottingham 9 9 A427 M1 MARKET A427 HARBOROUGH Gilmorton A43 A6 A508 A4304 Brigstock DESBOROUGH A6003 20 Husbands A508 A43 Bosworth Clipston ROTHWELL A6116 Islip Welford Swinford A14 19 Cranford A14 A14 Naseby KETTERING Moulton Boughton Broughton A45 M1 Yelvertoft Thornby BURTON Ringstead Lamport LATIMER A A43 5 Finedon 18 West Haddon 1 A508 A509 Boughton 9 RAUNDS 9 Brixworth A6 Green A428 Harrowden M45 17 Round East Spinney Haddon HIGHAM 2 WELLINGBOROUGH FERRERS A5 Long Moulton Mears Ashby Moulton Park A5076 Buckby RUSHDEN A45 00 A5076 A45 NORTHAMPTON Earls Wollaston A6 DAVENTRY Barton A45 A509 16 A45 Sharnbrook Boothville A428 Yardley Bozeat 15a Hastings Spinney A50 Hill Everdon Bugbrooke 15 Lavendon A5123 A43 Kingsthorpe The Arbours A43 Roade A428 Blakesley Olney Licence Number PU100029016 Licence Number PU100029016 . A508 Stagsden Towcester M1 A5095 Culworth A509 A422 Hanslope KEMPSTON Queen’s All rights reserved All rights reserved A5 NEWPORT Kingsley . Silverstone Wootton A508 Park A PAGNELL Park 413 Cosgrove A43 Cranfield A421 Greatworth 14 Kingsthorpe A5095 Hollow A43 © Crown Copyright 422 © Crown Copyright Weston BRACKLEY A Abington 13 Favell A45 A422 MILTON A KEYNES 421 BUCKINGHAM A5 A421 Woburn NORTHAMPTON 0 5 10 KM 0 500 1000 METRES Travelling to Moulton College From the South via the M1 & A43: Exit the M1 at Junction 15 and join the A508 North. -

Moulton Heights Northamptonshire Design and Access Statement
ED78B Moulton Heights Northamptonshire Design and Access Statement On behalf of: Roundhill Northampton Ltd By: Marchini Curran Associates Doc Ref:14077 D01_001_rev c marchini curran associates Moulton Heights, Northamptonshire 02 Content 1.0 Introduction / Vision 5.0 Visuals 5.1 Village Centre 2.0 Context 5.1 Village Green 2.1 East Midlands Region 5.2 Rural Edge 2.2 Northampton and its Growth 2.3 North of Northampton Town 6.0 Sustainability 3.0 The Site - Moulton 7.0 Equality / Lifetime Housing 3.1 Site Location 3.2 Parish Boundaries 8.0 Security / Privacy 3.3 Application Site and Land Ownership 3.4 Site Photographs 9.0 Access Statement 3.5 Site Context 3.6 Site Characteristics 10.0 Summary 3.7 Site History Archaeology 4.0 Design Strategy and Proposals 4.1 Design Objectives 4.2 Design Guides /References / Precedents 4.3 Access - Wider transport Strategy 4.4 Design Strategy Diagram 4.5 Design Development 4.6 Masterplan 4.7 Parameter Diagrams 4.8 Development Typology 4.9 Business / Mixed Use Zone 4.10 Primary School 4.11 Landscape Strategy 4.12 Connections 4.13 Community Facilities 4.14 Architectural Style 01 Artist’s impression of Moulton Heights marchini curran associates Moulton Heights, Northamptonshire 03 1.0 Introduction This Design and Access Statement has been prepared by Marchini Curran Associates on behalf of Roundhill Northampton Limited (the Applicant) in support of an outline planning application for development at Moulton Heights which lies to the north of the Northampton MUA and to the north west of the village of Moulton. -

The Manor House, Victors Barns, Northampton Road, Brixworth, Northamptonshire NN6 9DQ
The Manor House, Victors Barns, Northampton Road, Brixworth, Northamptonshire NN6 9DQ A most impressive stone Garden house with fabulous views Laying to the south and south west of the property with several patio areas, lawn, pool with terrace and over open countryside with views over open countryside. £2,950 pcm exclusive, Location unfurnished Brixworth is a large village situated to the north of Northampton and south of Market Harborough off The Property the A508. The village has shops, pubs, restaurant, primary schooling and an historic and ancient The Manor House is constructed of stone with Saxon church. The village is well placed for road interesting effects within to give a period feel. and rail networks with stations at Kettering, There are stone mullioned windows, deep Northampton and Market Harborough. There are a skirting boards, oak panelling, wooden arch- number of good private schools locally including shaped doors etc. The accommodation is over Spratton hall, Maidwell Hall and Northamptonshire three floors with three reception rooms, an Grammar School at Pitsford. Leisure facilities extremely spacious, newly fitted kitchen and include sailing and fishing at both Hollowell and large utility room. To the first floor is the Pitsford reservoirs, flying at Sywell and golf at master suite comprising bedroom, dressing Church Brampton and Harlestone. room, en suite shower room and floating galleried landing. To the second floor are three further bedrooms, one with an en suite shower • Northampton 8 miles room, and a family bathroom. -

Further Information on These Decisions Can Be
Delegated Weekly List For period Monday 18 December 2017 and Friday 22 December 2017 Further information on these decisions can be obtained from the Daventry District Council Website at: http://www.daventrydc.gov.uk/living/planning-and-building-control/search-comment-planning/ Application No. Location Proposal Decision Decision Date DA/2017/0751 2, Northampton Lane North, Demolition of existing house, garage and Approval Full 20-Dec-2017 Moulton, Northamptonshire, NN3 workshop. Construction of two detached 7RQ dwellings. DA/2017/0839 Lodge Farm, Pitsford Road, Lawful Development Certificate Approval Cert 20-Dec-2017 Moulton, Northamptonshire, NN3 (Proposed) for installation of solar pv of Lawfulness 7QL system to roof of existing college building Prop (Lodge Farm 1) DA/2017/0840 Moulton College (Pitsford Centre), Lawful Development Certificate Approval Cert 20-Dec-2017 Pitsford Road, Moulton, (Proposed) for installation of solar pv of Lawfulness Northamptonshire, NN3 7SX system to roof of existing college building Prop (Pitsford Centre - Chris Moody) DA/2017/0841 Moulton College (Pitsford Centre), Lawful Development Certificate Approval Cert 20-Dec-2017 Pitsford Road, Moulton, (Proposed) for installation of solar pv of Lawfulness Northamptonshire, NN3 7SX system to roof of existing college building Prop (Pitsford Centre - Equine Gate 4) DA/2017/0842 Moulton College (Holcot Centre), Lawful Development Certificate Approval Cert 20-Dec-2017 Pitsford Centre, Pitsford Road, (Proposed) for installation of solar pv of Lawfulness Moulton, Northamptonshire, -

Overstone Neighbourhood Development Plan 2019-2029
OVERSTONE NEIGHBOURHOOD DEVELOPMENT PLAN 2019-2029 Produced by the Overstone Neighbourhood Plan Steering Group and Overstone Parish Council Submission Version Contents Foreword ........................................................................................................................................... 3 Section 1: Introduction .................................................................................................................... 4 1.1. : Overview .......................................................................................................................4 1.2. : What is a Neighbourhood Development Plan? ...............................................................7 1.3. : How the Neighbourhood Development Plan fits into the Planning System .....................7 1.4. : Sustainability Appraisal ..................................................................................................8 1.5. : Community Engagement & Consultation .......................................................................9 Section 2: About Overstone and Its Demographics............................................................................ 10 2.1. : The History of Overstone ............................................................................................. 10 2.2. : Population and Housing Demographics ..................................................................... 11 2.3. : What Overstone will be like in the next 10 years? ........................................................ 13 2.4. : Growth -

Naseby Natters Issue 18
Now 350 copies delivered free every quarter! Naseby Natters issue 18 What’s Inside NASEBY AND BEYOND! • The Village Update • Wind Farm Update Welcome to yet another cram packed We are also trying to add a new article • Naseby Weather edition of Natters, but more entitled “All in a days work”. An insight • Textile Recycling importantly; welcome to the residents into a fascinating day job. • Naseby Churches of Haselbech who are now included in • Naseby School & NSA DID YOU KNOW? • A Bit About Sponsors the distribution of our much loved You can download all previous editions • Age Concern newsletter! of Naseby Natters from the • On Yer Bike • Village Hall & Sports Court We were approached a few months www.naseby.org web site. Right back to • Village Design Statement back by residents of Haselbech and issue 1! Also you can leave feedback • Battle of Naseby Series - Finale after a few discussions, it was felt that about Natters at anytime by filling in • Let’s Rant! • The Fitzgeralds of Naseby to include Haselbech was only full of the easy to follow on-line form. We’d love to hear what you think (good or • Open Gardens pluses! So welcome to you, one and all - • Biffa Land Fill-ed Up we hope you enjoy your first edition. For bad!) plus any ideas for future articles • Bit of Fun you might have. So get in touch! fellow Nasebians we hope issue 18 is • What a Waste • All in a Days Work better than ever! AJ Green - “Editor” • Great Expectations & Tragedy 01604 743765 • [email protected] • Great Daffodil Run ANOTHER NEW TEAM MEMBER: We - Happy reading to one and all - • Carvells Home Farm Show would like to take this opportunity to • Love Junk Mail welcome Becky Ash from Haselbech to THE NEWSLETTER TEAM • It’s a Dogs Life the ever expanding team. -

Court Farm House Overstone Park, Overstone, Northamptonshire NN6 0AP
Court Farm House Overstone Park, Overstone, Northamptonshire NN6 0AP A spacious contemporary house with Features • About 3,800 sq.ft. gross internal stables and land in a parkland • Five bedrooms • Entrance hall with cloakroom off • Four bath/shower rooms (two en suite) setting outside the village of • Drawing room, study and sitting room • Triple garage and stables • Well fitted kitchen/breakfast room Overstone • Landscaped garden, orchard and paddock • Large oak framed garden room • Games room with office above In all about 1.47 hectares (3.63 acres). • Utility room The Property Court Farm House dates from 1992 and is built of local limestone with brick detailing and a tiled roof. It stands some 600 yards off Sywell Road, Overstone in open parkland with its garden and paddock surrounding it on all sides. The house was built to a high standard with full double glazing, extensive use of oak joinery, a kitchen refurbished in 2005 and an excellent oak framed garden room added in 2009. The house has a wonderfully peaceful rural setting and yet is in walking distance of the village and close to the amenities of Northampton. Location Court Farm House lies to the south of the village of Overstone in the parkland of the once grand country house of Overstone Park. The house is approached over a long private road shared with neighbou ring properties. Within the parkland is Overstone Park Golf Club, which has a leisure pool, gym and an 18 hole golf course. There is a primary school in Overstone with secondary schooling in the nearby village of Moulton.