SNMMI Nuclear Medicine Technology Competency Based Curriculum
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

BREAST IMAGING for SCREENING and DIAGNOSING CANCER Policy Number: DIAGNOSTIC 105.9 T2 Effective Date: January 1, 2017
Oxford UnitedHealthcare® Oxford Clinical Policy BREAST IMAGING FOR SCREENING AND DIAGNOSING CANCER Policy Number: DIAGNOSTIC 105.9 T2 Effective Date: January 1, 2017 Table of Contents Page Related Policies INSTRUCTIONS FOR USE .......................................... 1 Omnibus Codes CONDITIONS OF COVERAGE ...................................... 1 Preventive Care Services BENEFIT CONSIDERATIONS ...................................... 2 Radiology Procedures Requiring Precertification for COVERAGE RATIONALE ............................................. 3 eviCore Healthcare Arrangement APPLICABLE CODES ................................................. 5 DESCRIPTION OF SERVICES ...................................... 6 CLINICAL EVIDENCE ................................................. 7 U.S. FOOD AND DRUG ADMINISTRATION ................... 16 REFERENCES .......................................................... 18 POLICY HISTORY/REVISION INFORMATION ................ 22 INSTRUCTIONS FOR USE This Clinical Policy provides assistance in interpreting Oxford benefit plans. Unless otherwise stated, Oxford policies do not apply to Medicare Advantage members. Oxford reserves the right, in its sole discretion, to modify its policies as necessary. This Clinical Policy is provided for informational purposes. It does not constitute medical advice. The term Oxford includes Oxford Health Plans, LLC and all of its subsidiaries as appropriate for these policies. When deciding coverage, the member specific benefit plan document must be referenced. The terms -

Breast Scintimammography
CLINICAL MEDICAL POLICY Policy Name: Breast Scintimammography Policy Number: MP-105-MD-PA Responsible Department(s): Medical Management Provider Notice Date: 11/23/2020 Issue Date: 11/23/2020 Effective Date: 12/21/2020 Next Annual Review: 10/2021 Revision Date: 09/16/2020 Products: Gateway Health℠ Medicaid Application: All participating hospitals and providers Page Number(s): 1 of 5 DISCLAIMER Gateway Health℠ (Gateway) medical policy is intended to serve only as a general reference resource regarding coverage for the services described. This policy does not constitute medical advice and is not intended to govern or otherwise influence medical decisions. POLICY STATEMENT Gateway Health℠ does not provide coverage in the Company’s Medicaid products for breast scintimammography. The service is considered experimental and investigational in all applications, including but not limited to use as an adjunct to mammography or in staging the axillary lymph nodes. This policy is designed to address medical necessity guidelines that are appropriate for the majority of individuals with a particular disease, illness or condition. Each person’s unique clinical circumstances warrant individual consideration, based upon review of applicable medical records. (Current applicable Pennsylvania HealthChoices Agreement Section V. Program Requirements, B. Prior Authorization of Services, 1. General Prior Authorization Requirements.) Policy No. MP-105-MD-PA Page 1 of 5 DEFINITIONS Prior Authorization Review Panel – A panel of representatives from within the Pennsylvania Department of Human Services who have been assigned organizational responsibility for the review, approval and denial of all PH-MCO Prior Authorization policies and procedures. Scintimammography A noninvasive supplemental diagnostic testing technology that requires the use of radiopharmaceuticals in order to detect tissues within the breast that accumulate higher levels of radioactive tracer that emit gamma radiation. -

Lacrimal Scintigraphy
LACRIMAL SCINTIGRAPHY Lacrimal Scintigraphy RO Boer, Medical Centre, Alkmaar (Retired) NOTE: no changes have been made since the version of 2007 1. Introduction A standardised volume of 10 μl 99mTc pertechnetate is instilled into the patient’s conjunctival sac using a micro-pipette. In principle, the quantity must be as small as possible, since any increase in the very small tear reservoir can lead to contamination of the eyelids and thus adversely affect the interpretability of the investigation. In contradistinction to the already well-established xray investigation whereby at all times outside influence is exerted on the tear drainage, the aim of this tracer investigation is to study the natural tear drainage. Normally, tears are drained from the conjunctival sac to the lacrimal sac (saccus lacrimalis), then to the naso-lacrimalduct (ductus nasolacrimalis) and finally to the nose and pharynx. 2. Methodology This guideline is based on available scientific literature on the subject, the previous guideline (Aanbevelingen Nucleaire Geneeskunde 2007), international guidelines from EANM and/or SNMMI if available and applicable to the Dutch situation. 3. Indications Epiphora (watering of the eye) is the initial indication. The ability to adequately manipulate the lacrimal pathways in order to improve drainage is closely linked to the indication. This is often achived through surgical procedures such as DCR (dacryocystorhinostomy) or DCP (dacryocystorhinoplasty, ‘angioplasty’ of the lacrimal pathways). Thereafter, the effect of these interventions can be evaluated by means of lacrimal scintigraphy. 4. Relation to other diagnostic procedures The Anel test is performed by cannulating the lower lacrimal point and injecting physiological saline. When the system becomes patent, the patient will taste salt. -

Procedure Guideline for Breast Scintigraphy
Procedure Guideline for Breast Scintigraphy Iraj Khalkhali, Linda E. Diggles, Raymond Taillefer, Penny R. Vandestreek, Patrick J. Peller and Hani H. Abdel-Nabi Harbor-UCLA Medical Center, Terranee; Nuclear Imaging Consultants, Roseville, California; Hospital Hôtel-Dieu de Montreal, Montreal, Quebec, Canada; Lutheran General Hospital, Park Ridge, Illinois; and University of Buffalo, Buffalo, New York Key Words: breast scintigraphy;procedureguideline should be available, as well as sonograms, if J NucÃMed 1999; 40:1233-1235 obtained. 2. A breast physical examination must be performed by either the nuclear medicine physician or the PART I: PURPOSE referring physician. 3. The time of last menses and pregnancy and lactat- The purpose of this guideline is to assist nuclear medicine ing status of the patient should be determined. practitioners in recommending, performing, interpreting and reporting the results of 99mTc-sestamibi breast scintigraphy 4. Breast scintigraphy should be delayed at least 2 wk after cyst or fine-needle aspiration, and 4—6wk (mammoscintigraphy, scintimammography). after core or excisional biopsy. 5. The nuclear medicine physician should be aware of PART II: BACKGROUND INFORMATION AND DEFINITIONS physical signs and symptoms and prior surgical procedures or therapy. Breast scintigraphy is performed after intravenous admin istration of "mTc-sestamibi and includes planar and/or C. Precautions None SPECT. D. Radiopharmaceutical 1. Intravenous injection of 740-1110 MBq (20-30 PART III: COMMON INDICATIONS AND APPLICATIONS mCi) 99mTc-sestamibi should be administered in an A. Evaluate breast cancer in patients in whom mammog- arm vein contralateral to the breast with the sus raphy is not diagnostic or is difficult to interpret (e.g., pected abnormality. -

A Molecular Approach to Breast Imaging
Journal of Nuclear Medicine, published on January 16, 2014 as doi:10.2967/jnumed.113.126102 FOCUS ON MOLECULAR IMAGING A Molecular Approach to Breast Imaging Amy M. Fowler Department of Radiology, University of Wisconsin–Madison, Madison, Wisconsin malignant cells. A recent meta-analysis of the accuracy of 99mTc-sestamibi scintimammography as an adjunct to di- Molecular imaging is a multimodality discipline for noninvasively agnostic mammography for detection of breast cancer dem- visualizing biologic processes at the subcellular level. Clinical applications of radionuclide-based molecular imaging for breast onstrated a sensitivity of 83% and specificity of 85% (2). cancer continue to evolve. Whole-body imaging, with scinti- However, sensitivity was less for nonpalpable (59%) versus mammography and PET, and newer dedicated breast imaging palpable lesions (87%) despite comparable specificity, with systems are reviewed. The potential clinical indications and the no significant difference between planar and SPECT meth- challenges of implementing these emerging technologies are ods. Decreased sensitivity for nonpalpable, presumably presented. smaller, lesions is in part due to the limited spatial resolu- Key Words: molecular imaging; oncology; breast; PET; PET/ tion of conventional g cameras. CT; radiopharmaceuticals; breast cancer; breast-specific g im- In addition to 99mTc-sestamibi, the positron-emitting ra- aging; positron-emission mammography; positron-emission to- diopharmaceutical 18F-FDG accumulates in many types of mography cancer including breast. Meta-analyses of the accuracy of J Nucl Med 2014; 55:1–4 whole-body 18F-FDG PET used after standard diagnostic DOI: 10.2967/jnumed.113.126102 workup for patients with suspected breast lesions demon- strated sensitivities of 83%–89% and specificities of 74%– 80% (3,4). -

Evaluation of Nipple Discharge
New 2016 American College of Radiology ACR Appropriateness Criteria® Evaluation of Nipple Discharge Variant 1: Physiologic nipple discharge. Female of any age. Initial imaging examination. Radiologic Procedure Rating Comments RRL* Mammography diagnostic 1 See references [2,4-7]. ☢☢ Digital breast tomosynthesis diagnostic 1 See references [2,4-7]. ☢☢ US breast 1 See references [2,4-7]. O MRI breast without and with IV contrast 1 See references [2,4-7]. O MRI breast without IV contrast 1 See references [2,4-7]. O FDG-PEM 1 See references [2,4-7]. ☢☢☢☢ Sestamibi MBI 1 See references [2,4-7]. ☢☢☢ Ductography 1 See references [2,4-7]. ☢☢ Image-guided core biopsy breast 1 See references [2,4-7]. Varies Image-guided fine needle aspiration breast 1 Varies *Relative Rating Scale: 1,2,3 Usually not appropriate; 4,5,6 May be appropriate; 7,8,9 Usually appropriate Radiation Level Variant 2: Pathologic nipple discharge. Male or female 40 years of age or older. Initial imaging examination. Radiologic Procedure Rating Comments RRL* See references [3,6,8,10,13,14,16,25- Mammography diagnostic 9 29,32,34,42-44,71-73]. ☢☢ See references [3,6,8,10,13,14,16,25- Digital breast tomosynthesis diagnostic 9 29,32,34,42-44,71-73]. ☢☢ US is usually complementary to mammography. It can be an alternative to mammography if the patient had a recent US breast 9 mammogram or is pregnant. See O references [3,5,10,12,13,16,25,30,31,45- 49]. MRI breast without and with IV contrast 1 See references [3,8,23,24,35,46,51-55]. -

Evaluation of the Quantitative Accuracy of a Commercially-Available Positron Emission Mammography Scanner
The Texas Medical Center Library DigitalCommons@TMC The University of Texas MD Anderson Cancer Center UTHealth Graduate School of The University of Texas MD Anderson Cancer Biomedical Sciences Dissertations and Theses Center UTHealth Graduate School of (Open Access) Biomedical Sciences 8-2010 EVALUATION OF THE QUANTITATIVE ACCURACY OF A COMMERCIALLY-AVAILABLE POSITRON EMISSION MAMMOGRAPHY SCANNER Adam Springer Follow this and additional works at: https://digitalcommons.library.tmc.edu/utgsbs_dissertations Part of the Diagnosis Commons, Equipment and Supplies Commons, and the Other Medical Sciences Commons Recommended Citation Springer, Adam, "EVALUATION OF THE QUANTITATIVE ACCURACY OF A COMMERCIALLY-AVAILABLE POSITRON EMISSION MAMMOGRAPHY SCANNER" (2010). The University of Texas MD Anderson Cancer Center UTHealth Graduate School of Biomedical Sciences Dissertations and Theses (Open Access). 64. https://digitalcommons.library.tmc.edu/utgsbs_dissertations/64 This Thesis (MS) is brought to you for free and open access by the The University of Texas MD Anderson Cancer Center UTHealth Graduate School of Biomedical Sciences at DigitalCommons@TMC. It has been accepted for inclusion in The University of Texas MD Anderson Cancer Center UTHealth Graduate School of Biomedical Sciences Dissertations and Theses (Open Access) by an authorized administrator of DigitalCommons@TMC. For more information, please contact [email protected]. EVALUATION OF THE QUANTITATIVE ACCURACY OF A COMMERCIALLY- AVAILABLE POSITRON EMISSION MAMMOGRAPHY SCANNER -
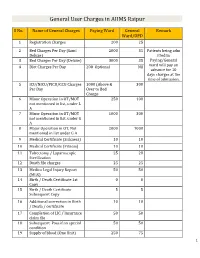
General User Charges in AIIMS Raipur
General User Charges in AIIMS Raipur S No. Name of General Charges Paying Ward General Remark Ward/OPD 1 Registration Charges 200 25 2 Bed Charges Per Day (Sami 2000 35 Patients being adm Deluxe) itted in 3 Bed Charges Per Day (Deluxe) 3000 35 Paying/General 4 Diet Charges Per Day 200 Optional Nil ward will pay an advance for 10 days charges at the time of admission. 5 ICU/NICU/PICU/CCU Charges 1000 (Above & 300 Per Day Over to Bed Charge 6 Minor Operation in OT/MOT 250 100 not mentioned in list, under L A 7 Minor Operation in OT/MOT 1000 300 not mentioned in list, under G A 8 Major Operation in OT, Not 2000 1000 mentioned in list under G A 9 Medical Certificate (Sickness) 10 10 10 Medical Certificate (Fitness) 10 10 11 Tubectomy / Laparoscopic 25 20 Sterilization 12 Death file charges 25 25 13 Medico Legal Injury Report 50 50 (MLR) 14 Birth / Death Certificate 1st 0 0 Copy 15 Birth / Death Certificate 5 5 Subsequent Copy 16 Additional correction in Birth 10 10 / Death / certificate 17 Completion of LIC / Insurance 50 50 claim file 18 Subsequent Pass if on special 50 50 condition 19 Supply of blood (One Unit) 250 75 1 20 Medical Board Certificate 500 500 On Special Case User Charges for Investigations in AIIMS Raipur S No. Name of Investigations Paying General Remark Ward Ward/OPD Anaesthsia 1 ABG 75 50 2 ABG ALONGWITH 150 100 ELECTROLYTES(NA+,K+)(Na,K) 3 ONLY ELECTROLYTES(Na+,K+,Cl,Ca+) 75 50 4 ONLY CALCIUM 50 25 5 GLUCOSE 25 20 6 LACTATE 25 20 7 UREA. -

Radioactive Seed Localization of Breast Lesions: an Adequate Localization Method Without Seed Migration
ORIGINAL ARTICLE Radioactive Seed Localization of Breast Lesions: An Adequate Localization Method without Seed Migration Tanja Alderliesten, PhD,* Claudette E. Loo, MD,* Kenneth E. Pengel, MSc,* Emiel J. Th. Rutgers, MD, PhD, Kenneth G. A. Gilhuijs, PhD,* and Marie-Jeanne T. F. D. Vrancken Peeters, MD, PhD *Department of Radiology; and Department of Surgery, The Netherlands Cancer Institute – Antoni van Leeuwenhoek Hospital (NKI-AVL), Amsterdam, The Netherlands n Abstract: Preoperative localization is important to optimize the surgical treatment of breast lesions, especially in nonpal- pable lesions. Radioactive seed localization (RSL) using iodine-125 is a relatively new approach. To provide accurate guid- ance to surgery, it is important that the seeds do not migrate after placement. The aim of this study was to assess short-term and long-term seed migration after RSL of breast lesions. In 45 patients, 48 RSL procedures were performed under ultrasound or stereotactic guidance. In the first 12 patients, the lesion was localized with two markers: an iodine-125 seed and a refer- ence marker. In 33 patients, 36 RSL procedures were performed using a single iodine-125 seed. All patients received control mammograms after seed placement and prior to surgery. In the patients with two markers, migration was defined as the differ- ence in the largest distance between the markers observed in the mammograms. For single-marked lesions, migration was assessed by comparing distances between anatomical landmarks in the mammograms. RSL was successful in all patients. Seeds were in-situ for 59.5 days on average (3–136 days). The detection rate during surgery was 100%. -
Nuclear Technology Reivew for 2002
GC GC(46)/INF/5 16 July 2002 International Atomic Energy Agency GENERAL Distr. GENERAL CONFERENCE Original: ENGLISH Forty-sixth regular session Item 15 of the provisional agenda (GC(46)/1) NUCLEAR TECHNOLOGY REVIEW 2002 1. In response to requests by Member States, the Secretariat produces a comprehensive Nuclear Technology Review every two years, with a shorter supplement in the intervening years. The present report is the second comprehensive compilation giving a global perspective on nuclear technologies for both power and non-power applications. 2. The NTR-2002 contains an Executive Summary and then reviews the following areas: Fundamentals of Nuclear Development; Nuclear Power, Fuel Cycle and Waste Management; Applications for Food, Water and Health; and Applications for Environment and Sustainable Industrial Processes. 3. The document has been modified to take account, to the extent possible, of specific comments by the Board and other comments received from Member States. For reasons of economy, this document has been printed in a limited number. Delegates are kindly requested to bring their copies of documents to meetings. GC(46)/INF/5 Page 2 NUCLEAR TECHNOLOGY REVIEW 2002 Table of Contents EXECUTIVE SUMMARY 4 PART I. FUNDAMENTALS OF NUCLEAR DEVELOPMENT 7 I-1. NUCLEAR, ATOMIC AND MOLECULAR DATA 7 I-2. RESEARCH REACTORS, ACCELERATORS AND RADIOISOTOPES 9 I-2.1. Research Reactors 9 I-2.2. Accelerators 11 I-2.3. Radioisotopes 13 I-3. NUCLEAR INSTRUMENTATION 14 I-4. NUCLEAR FUSION 15 PART II. NUCLEAR POWER, FUEL CYCLE AND WASTE MANAGEMENT 17 II-1. THE GLOBAL NUCLEAR POWER PICTURE 17 II-1.1. -

Intraoperative Gamma Probe Detection of Bone Invasive
Intraoperative and Postoperative Gamma Detection of Somatostatin Receptors in Bone Invasive “En Plaque” Meningiomas Emmanuel GAY, MD; Jean Philippe VUILLEZ, MD, PhD; Olivier PALOMBI, MD; Pierre Yves BRARD, MD; Pierre BESSOU, MD and Jean Guy PASSAGIA, MD. Department of Neurosurgery (EG, OP, JGP), Department of Nuclear Medecine (JPhV, PYB) and Departement of Neuroradiology (PB), University Hospital Grenoble, France. This is a non-final version of an article published in final form in Neurosurgery: July 2005 - Volume 57 - Issue 1 - pp 107-113 E. GAY Corresponding author: Emmanuel GAY, MD Department of Neurosurgery (Pr A.L. Benabid) CHU Grenoble BP217 38043 Grenoble Cedex 09 FRANCE Tel: 33 476 76 54 71 Fax: 33 476 76 58 13 Email: [email protected] 2 E. GAY Intraoperative and Postoperative Gamma Detection… Abstract: Objective: Scintigraphy with radiolabeled somatostatin analogue ([111In-DTPA] octreotide), detects the somatostatin receptors that are found in vitro in all meningiomas. Previous studies have proved the benefit of radioimmunoguided surgery with a handheld gamma probe, for the assessment and the removal of neuroendocrine tumors. We conducted a study to determine whether intraoperative radiodetection of somatostastin receptors is feasible and could increase the probability of complete meningioma resection, especially for bone invasive “en plaque” meningiomas that are difficult to control surgically. Methods: Eighteen patients with “en plaque” sphenoid wing and skull convexity meningiomas were studied for pre and post-operative somatostatin receptor scintigraphy. In 10 of them, intraoperative radiodetection using a handheld gamma probe was performed 24 hours after the intravenous administration of [111In-DTPA] octreotide. This procedure was combined with a computer-aided navigation system. -

(EANM) Acceptance Testing for Nuclear Medicine Instrumentation
Eur J Nucl Med Mol Imaging (2010) 37:672–681 DOI 10.1007/s00259-009-1348-x GUIDELINES Acceptance testing for nuclear medicine instrumentation Ellinor Busemann Sokole & Anna Płachcínska & Alan Britten & on behalf of the EANM Physics Committee Published online: 5 February 2010 # EANM 2010 Keywords Quality control . Quality assurance . requirement that acceptance testing be performed should Acceptance testing . Nuclear medicine instrumentation . be included in the purchase agreement of an instrument. Gamma camera . SPECT. PET. CT. Radionuclide calibrator. This agreement should specify responsibilities regarding Thyropid uptake probe . Nonimaging intraoperative probe . who does acceptance testing, the procedure to be followed Gamma counting system . Radiation monitors . when unsatisfactory results are obtained, and who supplies Preclinical PET the required phantoms and software. A specific time slot must be allocated for performing acceptance tests. Introduction Acceptance and reference tests These recommendations cover acceptance and reference tests that should be performed for acceptance testing of Acceptance tests are performed to verify that the instrument instrumentation used within a nuclear medicine department. performs according to its specifications. Each instrument is These tests must be performed after installation and before supplied with a set of basic specifications. These have been the instrument is put into clinical use, and before final produced by the manufacturer according to standard test payment for the device. These recommendations