Our System-Wide Remobilisation Plan April 2021 to March 2022
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Board Papers -June 2021
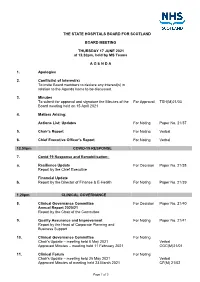
THE STATE HOSPITALS BOARD FOR SCOTLAND BOARD MEETING THURSDAY 17 JUNE 2021 at 12.30pm, held by MS Teams A G E N D A 1. Apologies 2. Conflict(s) of Interest(s) To invite Board members to declare any interest(s) in relation to the Agenda Items to be discussed. 3. Minutes To submit for approval and signature the Minutes of the For Approval TSH(M)21/03 Board meeting held on 15 April 2021 4. Matters Arising: Actions List: Updates For Noting Paper No. 21/37 5. Chair’s Report For Noting Verbal 6. Chief Executive Officer’s Report For Noting Verbal 12.50pm COVID-19 RESPONSE 7. Covid 19 Response and Remobilisation: a. Resilience Update For Decision Paper No. 21/38 Report by the Chief Executive Financial Update b. Report by the Director of Finance & E-Health For Noting Paper No. 21/39 1.20pm CLINICAL GOVERNANCE 8. Clinical Governance Committee For Decision Paper No. 21/40 Annual Report 2020/21 Report by the Chair of the Committee 9. Quality Assurance and Improvement For Noting Paper No. 21/41 Report by the Head of Corporate Planning and Business Support 10. Clinical Governance Committee For Noting Chair’s Update – meeting held 6 May 2021 Verbal Approved Minutes – meeting held 11 February 2021 CGC(M)21/01 11. Clinical Forum For Noting Chair’s Update – meeting held 25 May 2021 Verbal Approved Minutes of meeting held 23 March 2021 CF(M) 21/02 Page 1 of 3 1.45pm STAFF GOVERNANCE 12. Staff Governance Committee For Decision Paper No. -

Emergency Care Weekly Metadata
Publication Metadata (including revision details) Metadata Description Indicator Publication Weekly Update of Emergency Department Activity and Waiting title Times. Description This publication reports key statistics on attendances at Emergency Departments (ED) across Scotland. The information presented in the publication includes trends in the number of attendances and length of time patients spend in ED. Theme Health and Social Care Topic Emergency Care Format Webpage, Excel workbook and CSV. Data source(s) NHS Board aggregate submissions to PHS on Emergency Department Activity and Waiting Times. Date that data Tuesday of the week prior to publication are acquired Release date Every Tuesday Frequency Weekly Timeframe of New data for the week ending 9 days before publication (e.g. 16 data and April publication contains data for week ending 7 April) timeliness Continuity of 1) A&E discharge times at hospitals in NHS Lothian were not data accurately recorded up to November 2017. The Academy of Medical Royal Colleges was commissioned by Scottish Government to ascertain the causes for the data issues in NHS Lothian. The review findings were published 26 June 2018. 2) Since 3 March 2015, the Scottish Government (SG) has released Official Statistics weekly A&E activity and waiting times information for the EDs in Scotland, derived from aggregate information supplied by NHS Boards on the number of attendances and 4, 8, and 12 hour waits. PHS (formally ISD) took over this data collection for statistics covering the week ending 7 June 2015. 3) From 20 May 2018, Raigmore hospital in NHS Highland trialled a new patient flow system. As a consequence the accuracy of some patients’ waits may have been affected between this date and 4 July, however the total number of attendances remains correct. -

Integration Joint Board Meeting Agenda
A meeting of the Clackmannanshire and Stirling Integration Joint Board will be held on Wednesday 17 June 2020 at 2pm - 4pm, By Video Conference Please notify apologies for absence to: [email protected] INTEGRATION JOINT BOARD MEETING AGENDA 1. NOTIFICATION OF APOLOGIES For Noting 2. NOTIFICATION OF SUBSTITUTES For Noting 3. DECLARATION(S) OF INTEREST For Noting 4. URGENT BUSINESS BROUGHT FORWARD BY CHAIRPERSON 5. MINUTE OF THE CLACKMANNANSHIRE & STIRLING INTEGRATION For Approval JOINT BOARD MEETING HELD ON 25 MARCH 2020 6. ACTION LOG 7. TRANSFORMING CARE AND STRATEGIC PLANNING 7.1 PRIMARY CARE IMRPROVEMENT PLAN For Noting (Paper Presented by Dr Stuart Cummings / Lesley Middlemiss) 7.2 MOBILISATION PLAN For Noting (Paper Presented by Wendy Forrest) 8. FINANCE 8.1 YEAR END FINANCE REPORT For Noting & (Paper Presented by Ewan Murray) Approval 9. PERFORMANCE 9.1 COVID - 19 UPDATE REPORT For Noting (Paper presented by Wendy Forrest / Ewan Murray) 9.2 PERFORMANCE REPORT For Noting & (Paper presented by Carolyn Wyllie) Approval 10. GOVERNANCE 10.1 INTEGRATION SCHEME For Noting (Paper presented by Lesley Fulford) 10.2 URGENT DECISION MAKING For Approval (Paper presented by Lindsay Thomson) 11. FOR NOTING 11.1 MINUTES a) STRATEGIC PLANNING GROUP: None for noting b) JOINT STAFF FORUM: None for noting c) IJB AUDIT & RISK COMMITTEE: None for noting d) CLINICAL CARE & GOVERNANCE MEETING: None for noting 12. EXEMPT ITEMS E12.1 None for noting 13. DATE OF NEXT MEETING Wednesday 23 September 2020 at 2 - 4pm Location or Videoconference -

NHS Forth Valley- Briefing Scottish Parliament Health and Sport Committee
NHS Forth Valley- Briefing Scottish Parliament Health and Sport Committee Contents 1.0 NHS Forth Valley - Strategic Context Page 2 2.0 Strategic Background: Links to ‘A Case for Change’, Healthcare Strategy- Shaping Page 3 the Future and Supporting Strategies 3.0 Progress in delivery of the Local Delivery Plan Page 5 3.1 Annual Review 2016/17: Links to Self Assessment and Annual Review Letter Page 5 3.2 LDP 2017/18: Link to NHS Forth Valley Annual Plan incorporating LDP Page 5 3.3 Approach to Performance : Link to Core Performance Report Page 5 3.4 Balanced Scorecard Summary Page 5 3.5 Timely Care Page 6 3.5.1 Unscheduled Care Page 6 3.5.2 Planned Care Page 6 3.6 Safe and Person Centred Care Page 11 3.6.1 HAI Page 11 3.6.2 HSMR Page 12 3.6.3 Complaints Page 12 3.7 Effective and Efficient care Page 15 3.7.1 Financial Performance Page 15 4.0 Progress and Performance of Integrated Joint Boards Page 16 4.1 Context Page 16 4.2 Key Targets Page 16 4.2.1 Delayed Discharges Page 16 4.2.2 Unplanned Attendance, Unplanned Admission, Unplanned Beddays Page 17 1 1.0 NHS Forth Valley - Strategic Context 1.1 Physicality Forth Valley is situated in the heart of Scotland in the central belt in between two large health boards with teaching hospitals, Glasgow in the West and Edinburgh in the East, and covers a geographic area from Killin and Tyndrum in the North and Strathblane to the west and Bo’ness in the South, see diagram 1. -

NHS Guidlines
NHSScotland Identity guidelines Identikit Introduction In December 2000, Susan Deacon MSP, In this publication, the Minister said: “The public relate to and recognise Minister for Health and Community Care, the NHS. They believe their care is launched ‘Our National Health: provided by a national health service and staff take pride in the fact that a plan for action, a plan for change’ they work for the NHS. Research tells us that the variety of differently which set out a clear direction for the NHS named NHS bodies confuses the in Scotland with the aims of improving public and alienates staff. As part of our proposals to rebuild the National people’s health and creating a 21st century Health Service we will promote a new identity for the NHS in Scotland.” health service. The guidelines that follow provide an essential design toolkit to establish “Alongside the changes in NHS this new identity. The guidelines cover signage, vehicles, uniforms, stationery, boardrooms, we will re-establish literature, forms and other items. The a national identity for the aim is to replace, over time, the array of existing identities within NHS NHS in Scotland.” organisations with the single NHS identity while avoiding wastage and unnecessary expenditure. Our National Health: a plan for action, a plan for change section 3/page 31 2 Contents Section 1 Our national identity 4 Exclusion zone 6 Minimum size 6 Section 2 Identity structure 7 Essential elements 9 Identity variants 10 Caring device 12 Positioning the identity 14 Other identities 15 Working in partnership 16 Section 3 Identities for ideas & initiatives 17 Initiatives 18 Section 4 NHSScotland typefaces 19 Stone Sans 20 Arial 24 Garamond 25 Times New Roman 26 Literature 27 Section 5 Colour 28 Using colour 29 Primary colours 30 Colour palette 31 Tints 32 Printing the identity 33 3 Section One Our national identity Together, the initials ‘NHS’ and the caring symbol form the foundations of our identity. -

Mental Health Bed Census
Scottish Government One Day Audit of Inpatient Bed Use Definitions for Data Recording VERSION 2.4 – 10.11.14 Data Collection Documentation Document Type: Guidance Notes Collections: 1. Mental Health and Learning Disability Bed Census: One Day Audit 2. Mental Health and Learning Disability Patients: Out of Scotland and Out of NHS Placements SG deadline: 30th November 2014 Coverage: Census date: Midnight, 29th Oct 2014 Page 1 – 10 Nov 2014 Scottish Government One Day Audit of Inpatient Bed Use Definitions for Data Recording VERSION 2.4 – 10.11.14 Document Details Issue History Version Status Authors Issue Date Issued To Comments / changes 1.0 Draft Moira Connolly, NHS Boards Beth Hamilton, Claire Gordon, Ellen Lynch 1.14 Draft Beth Hamilton, Ellen Lynch, John Mitchell, Moira Connolly, Claire Gordon, 2.0 Final Beth Hamilton, 19th Sept 2014 NHS Boards, Ellen Lynch, Scottish John Mitchell, Government Moira Connolly, website Claire Gordon, 2.1 Final Ellen Lynch 9th Oct 2014 NHS Boards, Further clarification included for the following data items:: Scottish Government Patient names (applicable for both censuses) website ProcXed.Net will convert to BLOCK CAPITALS, NHS Boards do not have to do this in advance. Other diagnosis (applicable for both censuses) If free text is being used then separate each health condition with a comma. Mental Health and Learning Disability Bed Census o Data item: Mental Health/Learning Disability diagnosis on admission Can use full description option or ICD10 code only option. o Data item: Last known Mental Health/Learning Disability diagnosis Can use full description option or ICD10 code only option. -

Acute Hospital Activity and NHS Beds Information for Scotland
Acute Hospital Activity and NHS Beds Information for Scotland Annual – Year ending 31 March 2020 A National Statistics release for Scotland Public Health Scotland This is a National Statistics publication National Statistics status means that the official statistics meet the highest standards of trustworthiness, quality and public value. They are identified by the quality mark shown above. The UK Statistics Authority has designated these statistics as National Statistics signifying compliance with the Code of Practice for Statistics. Once statistics have been designated as National Statistics, it is a statutory requirement that the Code of Practice shall continue to be observed. The statistics last underwent a full assessment by the Office for Statistics Regulation (OSR) against the Code of Practice in September 2011. The OSR is the regulatory arm of the UK Statistics Authority. Find out more about the Code of Practice at: https://www.statisticsauthority.gov.uk/osr/code-of-practice/ Find out more about National Statistics at: https://www.statisticsauthority.gov.uk/national-statistician/types-of-official-statistics/ 1 Public Health Scotland Contents Introduction ...................................................................................................................................3 COVID-19 .....................................................................................................................................3 Background ...................................................................................................................................4 -

Strategic Plan
Strategic Plan Clackmannanshire and Stirling Strategic Plan 2016 - 2019 Health and Social Care Partnership Clackmannanshire and Stirling Strategic Plan Clackmannanshire and Stirling Strategic Plan Contents Foreword 2 Background to Health & Social Care Integration .. .. .. .. .. .. .. .. .. .. .. .. .. .. .. .. .. .. .. .. .. .. ..3 .. .. .. .. .. Clackmannanshire & Stirling Health and Social Care Partnership 3 Integration Joint Board 3 Chief Officer .. .. .. .. .. .. .. .. .. .. .. .. .. .. .. .. .. .. .. .. .. .. .. .. .. .. .. .. .. .. .. .. .. .. .. .. .. .. .. .. .. .. ..3 .. .. .. .. .. .. The Strategic Plan .. .. .. .. .. .. .. .. .. .. .. .. .. .. .. .. .. .. .. .. .. .. .. .. .. .. .. .. .. .. 3.. .. .. .. .. .. .. .. .. .. .. .. .. .. .. .. .. Localities .. .. .. .. .. .. .. .. .. .. .. .. .. .. .. .. .. .. .. .. .. .. .. .. .. .. .. .. .. .. .. .. .. .. .. .. .. .. .. .. .. .. .. .. .. .. .. .. .. .. .. 3 Community Planning Partnerships 3 The Case for Change .. .. .. .. .. .. .. .. .. .. .. .. .. .. .. .. .. .. .. .. .. .. .. .. .. .. .. .. .. .. .. .. .. .. .. .. ..4 .. .. .. Why do we need to change? 4 Profile of Clackmannanshire Council & Stirling Council Areas 4 Our Vision and Outcomes 9 Our Local Vision and Outcomes 9 Outcomes .. .. .. .. .. .. .. .. .. .. .. .. .. .. .. .. .. .. .. .. .. .. .. .. .. .. .. .. .. .. .. .. .. .. .. .. .. .. .. .. .. .. .. .. .. .. .. .. .. .. 9 How we will achieve Improved Outcomes 10 What does all of this mean for you? 11 Services working in partnership 11 Key Themes and Ambitions 12 Our -

NIMH 250418 Name Role Locality Dr Sarah Beesley Lead Clinician And
NIMH 250418 Name Role Locality Dr Sarah Beesley Lead Clinician and Consultant Psychiatrist Gartnavel Royal Hospital Mr Simon Burt General Manager NHS Borders Locum Consultant Psychiatrist; Former Lead Clinician for Physical Healthcare in Mental Eastwood Health and Care Centre; NHS Greater Glasgow and Clyde; Scottish Dr Moira Connolly Health; Former Principal Medical Officer (Mental Health Government Ms Laura Coyle Lundbeck Dr Marie Devanney Consultant Psychiatrist NHS Lanarkshire Mr David Ellerby Practice Based Pharmacist Health and Social Care Moray Ms Maureen Johnston Strategic Inspector - Adults Care Inspectorate Dr Ihsan Kader Consultant Psychiatrist NHS Lothian Prof Stephen Lawrie Head of Psychiatry The University of Edinburgh Dr John Logan Consultant in Public Health Medicine NHS Lanarkshire Dr Angus MacBeth Lecturer in Clinical Psychology / Honorary Principal Clinical Psychologist University of Edinburgh / NHS Grampian Ms Anne MacDonald Senior Counsellor and Supervisor Morayshire Dr Justine McCulloch Consultant Psychiatrist NHS Forth Valley Mrs Linda Mckechnie Lead Nurse and Professional Manager, Community Mental Health Services NHS Dumfries and Galloway Mr Stuart McKenzie Chair of Congress; Clinical Nurse Manager in Forensic and Rehabilitation Services Royal College of Nursing, Scotland Dr Catriona McMahon Lead Industry Member Scottish Medicines Consortium Dr Lily McNamee Research Coordinator NRS Mental Health Network Mr Paul Midgley Director of NHS Insight Wilmington Healthcare Mr Graham Morgan MBE Engagement Officer Mental Welfare -

Scotland's Out-Of-Hospital Cardiac Arrest Strategy 2021-2026
Scotland’s Out-of-Hospital Cardiac Arrest Strategy 2021-2026 March 2021 Scotland’s Out of Hospital Cardiac Arrest Strategy 1. Foreword 2. Introduction a. Progress to date b. Partners to the strategy c. Covid-19 3. Summary of the Strategy aims Pathway for survival: 4. Getting Scotland Ready - We will ensure people in Scotland can identify the signs of a cardiac arrest. 5. Bystander Action - We will encourage an increased willingness to call 999, deliver bystander CPR and defibrillation among people who witness an out-of-hospital cardiac arrest. 6. Hospital Care - We will ensure patients receive high-quality, person-centred care. 7. Aftercare - We will ensure that people in Scotland affected by out-of-hospital cardiac arrest receive appropriate aftercare. 8. Data and Innovation – We will ensure access to timely, high quality data to facilitate open review, discussion, learning and action planning. Conclusion and Annexes 9. Conclusion 10. Annex A: Overlapping strategies 11. Annex B: Glossary 12. Annex C: References 1 Strategy Foreword Mairi Gougeon, Minister for Public Health and Sport Every year, over 3,000 people in Scotland experience an out-of-hospital cardiac arrest (OHCA). A cardiac arrest is when the heart stops pumping blood around the body, commonly because of a problem with the electrical signals in a person’s heart. It is a significant healthcare challenge and addressing it is a priority for the Scottish Government. Throughout the last five years, the Save a Life for Scotland (SALFS) partnership has equipped over 640,000 people, around 11% of the population of Scotland, with CPR skills. -

Forth Valley Community Health Partnerships Scheme Of
DDDrrraaafffttt ––– vvveeerrrsssiioioonnn 666 Forth Valley Community Health Partnerships Scheme of Establishment ‘Working Together For Healthier Communities’ 1 222333 DDDeeeccceeemmmbbbeeerrr 222000000444 DDDrrraaafffttt ––– vvveeerrrsssiioioonnn 666 Contents 1. INTRODUCTION.........................................................................................................................5 1.1 OUR VISION .....................................................................................................................................6 1.2 BACKGROUND..................................................................................................................................6 1.3 OUR APPROACH IN FORTH VALLEY .................................................................................................8 1.4 PRINCIPLES ......................................................................................................................................9 1.5 OBJECTIVES ...................................................................................................................................10 2. IMPROVING SERVICES..........................................................................................................12 2.1 OUTCOMES.....................................................................................................................................12 2.1.1 Shift locus of care to local communities........................................................................................12 2.1.2 Closing the Inequality -

PHS Procurement Strategy 2020-2023
Public Health Scotland procurement strategy 2020–23 1 Note: In line with the Reform Act and to ensure our annual procurement report details our performance against the strategy, this strategy will be subject to formal annual review. This will take account of any changes to organisational objectives and in NHS and Scottish Government policies and strategies. Strategy owner: Kris Lindsay, Procurement Manager Email: [email protected] Telephone: 0131 275 7454 Citation: Lindsay K. Public Health Scotland procurement strategy 2020–23. Edinburgh: Public Health Scotland; 2021. Contents Definition Glossary ..................................................................................................................... 2 Introduction ................................................................................................................ 4 Procurement vision/mission statement ....................................................................... 4 Strategy rationale ....................................................................................................... 5 Strategic aims, objectives and key priorities ............................................................... 6 Mandatory obligations .............................................................................................. 11 Engaging with suppliers ........................................................................................... 12 Monitoring, reviewing and reporting ......................................................................... 16 1 Glossary