Direct Toxicity of Iodinated Radiocontrast Media on Renal
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Pharmacologyonline 2: 727-753 (2010) Ewsletter Bradu and Rossini
Pharmacologyonline 2: 727-753 (2010) ewsletter Bradu and Rossini COTRAST AGETS - IODIATED PRODUCTS. SECOD WHO-ITA / ITA-OMS 2010 COTRIBUTIO O AGGREGATE WHO SYSTEM-ORGA CLASS DISORDERS AD/OR CLUSTERIG BASED O REPORTED ADVERSE REACTIOS/EVETS Dan Bradu and Luigi Rossini* Servizio Nazionale Collaborativo WHO-ITA / ITA-OMS, Università Politecnica delle Marche e Progetto di Farmacotossicovigilanza, Azienda Ospedaliera Universitaria Ospedali Riuniti di Ancona, Regione Marche, Italia Summary From the 2010 total basic adverse reactions and events collected as ADRs preferred names in the WHO-Uppsala Drug Monitoring Programme, subdivided in its first two twenty years periods as for the first seven iodinated products diagnostic contrast agents amidotrizoate, iodamide, iotalamate, iodoxamate, ioxaglate, iohexsol and iopamidol, their 30 WHO-system organ class disorders (SOCDs) aggregates had been compared. Their common maximum 97% levels identified six SOCDs only, apt to evaluate the most frequent single ADRs for each class, and their percentual normalization profiles for each product. The WILKS's chi square statistics for the related contingency tables, and Gabriel’s STP procedure applied to the extracted double data sets then produced profile binary clustering, as well as Euclidean confirmatory plots. They finally showed similar objectively evaluated autoclassificative trends of these products, which do not completely correspond to their actual ATC V08A A, B and C subdivision: while amidotrizoate and iotalamate, and respectively iohesol and iopamidol are confirmed to belong to the A and B subgroups, ioxaglate behaves fluctuating within A, B and C, but iodamide looks surprizingly, constantly positioned together with iodoxamate as binary/ternary C associated. In view of the recent work of Campillos et al (Science, 2008) which throws light on the subject, the above discrepancies do not appear anymore unexpected or alarming. -

Proceedings of the Fifty-Eighth Annual Meeting of the American Society for Clinical Investigation, Inc., Held in Atlantic City, N.J., May 2, 1966: Abstracts
Proceedings of the Fifty-Eighth Annual Meeting of the American Society for Clinical Investigation, Inc., Held in Atlantic City, N.J., May 2, 1966: Abstracts J Clin Invest. 1966;45(6):980-1037. https://doi.org/10.1172/JCI105414. Research Article Find the latest version: https://jci.me/105414/pdf ABSTRACTS Comparison of Effects of Alpha Adrenergic Blockade luminescence. Inhibition of ATPase activities by ouabain, on Resistance and Capacitance Vessels. FRANCOIS parachloromercuribenzoate (PCMB), and parachloro- M. ABBOUD * AND JOHN W. ECKSTEIN,* Iowa City, mercuribenzenesulfonate (PCMBS) was studied. ¶1 Mem- Iowa. brane ATPase of osmotically prepared platelet "ghosts" A foreleg of each of 20 dogs was perfused with blood is composed of Na+-K+-Mg++-dependent ATPase (15 to at a constant rate through the brachial artery. The 30%) and Mg++-activated ATPase (60 to 85%o). Ouabain nerves of the brachial plexus were transected, and an (10' M), which inhibits the Na+-K--dependent ATPase electrode was applied to their distal ends. Pressures were activity and produces a resultant loss of cellular K+, gain recorded simultaneously from the brachial artery and of Na+, and cell swelling, does not inhibit either ADP cephalic vein and from a small artery and small vein in aggregation or clot retraction. ¶f PCMB, an organic the paw. Pressor responses to injections of nor- mercurial compound that diffuses into cells, totally inacti- epinephrine (1, 2, and 4 /.tg) into the brachial artery and vates both ATPase activities in the ghost preparations to nerve stimulation (3, 6, and 12 cps) were measured and in the intact platelet. -

Evaluation Report Radiocontrast Agents
Evaluation report Radiocontrast agents Report No. 187 Within the strategy aimed at reducing micro-pollutant inputs originating from ur- ban and industrial waste water, evaluation reports are being drafted for 10 groups of substances targeted at summarizing scientifi c and technical facts and at pointing out gaps of knowledge. Also, the evaluation reports present a variety of possible mea- sures at the source (e.g. registration of substances, limitation of uses) and technical measures in crucial wastewater treatment plants (e.g. introducing a further treatment stage). The “Conclusions” of the evaluation reports list the most effi cient measures to be further investigated into within a holistic ICPR strategy. However, these measures are no recommendations the ICPR addresses to its member states. Measures listed in this chapter will be integrated into a survey report of all measures in order to be able to take into account eventual synergetic effects of measures (effects of measures on different groups of substances) when proceeding with the fi nal evaluation. Based on the fi nal evaluation of all measures the ICPR will determine recommendations for the Member States Imprint Publisher: International Commission for the Protection of the Rhine (ICPR) Kaiserin-Augusta-Anlagen 15, D 56068 Koblenz P.O. box 20 02 53, D 56002 Koblenz Telephone +49-(0)261-94252-0, Fax +49-(0)261-94252-52 Email: [email protected] www.iksr.org ISBN 935324-53-7 © IKSR-CIPR-ICBR 2010 IKSR CIPR ICBR Evaluation report Radiocontrast agents 1. Introduction Radiocontrast agents are used for diagnostic purposes, as they absorb X-rays to a greater extent than human soft tissue and thus visualize these tissues. -
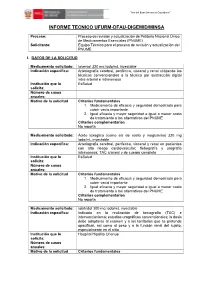
Informe Tecnico Ufurm-Dfau-Digemid/Minsa
“Año del Buen Servicio al Ciudadano” ” INFORME TECNICO UFURM-DFAU-DIGEMID/MINSA Proceso: Proceso de revisión y actualización de Petitorio Nacional Único de Medicamentos Esenciales (PNUME) Solicitante: Equipo Técnico para el proceso de revisión y actualización del PNUME I. DATOS DE LA SOLICITUD Medicamento solicitado: Ioversol 320 mg Iodo/mL inyectable Indicación específica: Arteriografía cerebral, periférica, visceral y renal utilizando las técnicas convencionales o la técnica por sustracción digital intra-arterial e intravenosa Institución que lo EsSalud solicita: Número de casos anuales: Motivo de la solicitud Criterios fundamentales 1. Medicamento de eficacia y seguridad demostrada para cubrir vacío importante. 2. Igual eficacia y mayor seguridad e igual o menor costo de tratamiento a las alternativas del PNUME Criterios complementarios No reporta Medicamento solicitado: Ácido ioxaglico (como sal de sodio y meglumina) 320 mg Iodo/mL inyectable Indicación específica: Arteriografia cerebral, periferica, visceral y renal en pacientes con alto riesgo cardiovascular; flebografía y urografía intravenosa; TAC craneal y de cuerpo completo Institución que lo EsSalud solicita: Número de casos anuales: Motivo de la solicitud Criterios fundamentales 1. Medicamento de eficacia y seguridad demostrada para cubrir vació importante. 2. Igual eficacia y mayor seguridad e igual o menor costo de tratamiento a las alternativas del PNUME Criterios complementarios No reporta Medicamento solicitado: Iobitridol 300 mg Iodo/mL inyectable Indicación específica: Indicado en la realización de tomografía (TAC) e intervencionismo; estudios urográficos convencionales; la dosis debe adaptarse al examen y a los territorios que se pretende opacificar, asi como al peso y a la función renal del sujeto, especialmente en el niño Institución que lo Hospital Hipólito Unanue solicita: Número de casos anuales: Motivo de la solicitud Criterios fundamentales “Año del Buen Servicio al Ciudadano” ” 1. -

Radiocontrast Agent Diatrizoic Acid Induces Mitophagy and Oxidative Stress Via Calcium Dysregulation
International Journal of Molecular Sciences Article Radiocontrast Agent Diatrizoic Acid Induces Mitophagy and Oxidative Stress via Calcium Dysregulation Dakota B. Ward, Kathleen C. Brown and Monica A. Valentovic * Department of Biomedical Sciences, Toxicology Research Cluster, Joan C. Edwards School of Medicine, Marshall University, 1 Marshall Drive, Huntington, WV 25755, USA * Correspondence: [email protected]; Tel.: +1-304-696-7332; Fax: +1-304-696-7391 Received: 20 May 2019; Accepted: 18 August 2019; Published: 21 August 2019 Abstract: Contrast-induced acute kidney injury (CI-AKI) is the third most common cause of hospital associated kidney damage. Potential mechanisms of CI-AKI may involve diminished renal hemodynamics, inflammatory responses, and direct cytotoxicity. The hypothesis for this study is that diatrizoic acid (DA) induces direct cytotoxicity to human proximal tubule (HK-2) cells via calcium dysregulation, mitochondrial dysfunction, and oxidative stress. HK-2 cells were exposed to 0–30 mg I/mL DA or vehicle for 2–24 h. Conversion of 3-(4,5-dimethylthiazol-2-yl)-2,5-diphenyltetrazolium bromide (MTT) and trypan blue exclusion indicated a decrease in mitochondrial and cell viability within 2 and 24 h, respectively. Mitochondrial dysfunction was apparent within 8 h post exposure to 15 mg I/mL DA as shown by Seahorse XF cell mito and Glycolysis Stress tests. Mitophagy was increased at 8 h by 15 mg I/mL DA as confirmed by elevated LC3BII/I expression ratio. HK-2 cells pretreated with calcium level modulators BAPTA-AM, EGTA, or 2-aminophenyl borinate abrogated DA-induced mitochondrial damage. DA increased oxidative stress biomarkers of protein carbonylation and 4-hydroxynonenol (4HNE) adduct formation. -

DISEASE of the MONTH J Am Soc Nephrol 11: 177–182, 2000
DISEASE OF THE MONTH J Am Soc Nephrol 11: 177–182, 2000 Contrast Nephropathy SEAN W. MURPHY, BRENDAN J. BARRETT, and PATRICK S. PARFREY Division of Nephrology and Clinical Epidemiology Unit, Memorial University of Newfoundland, St. John’s, Newfoundland, Canada. With the increasing use of radiographic contrast media in changes of cell injury and enzymuria after contrast administration diagnostic and interventional procedures, contrast-induced ne- (9). The nature of the contrast, associated ions, concentration, and phropathy (CN) has become an important cause of iatrogenic concomitant hypoxia are all important to the degree of cellular acute renal impairment. In fact, CN is the third leading cause damage, while the osmolality of the solution seems to be of of new acute renal failure in hospitalized patients (1). The secondary importance (8). The injection of contrast induces a pathophysiology and risk factors for this complication are biphasic hemodynamic change in the kidney, with an initial, becoming better understood, but there is still controversy sur- transient increase and then a more prolonged decrease in renal rounding many aspects. The purpose of this article is to review blood flow (2). The mediators of these changes are still unknown. recent developments in the area of CN. Particular emphasis Alterations in the metabolism of prostaglandin, nitric oxide, en- will be placed on means of minimizing the risk or preventing dothelin, or adenosine may play a role. this important problem. Risk Factors and Epidemiology Definition and Clinical Features Mild, transient decreases in GFR occur after contrast admin- Many different definitions of CN appear in the literature, but istration in almost all patient (10). -
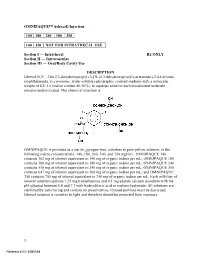
OMNIPAQUE™ (Iohexol) Injection
OMNIPAQUE™ (iohexol) Injection 140 180 240 300 350 140 350 NOT FOR INTRATHECAL USE Section I — Intrathecal Rx ONLY Section II — Intravascular Section III — Oral/Body Cavity Use DESCRIPTION Iohexol,N,N´ - Bis(2,3-dihydroxypropyl)-5-[N-(2,3-dihydroxypropyl)-acetamido]-2,4,6-triiodo- isophthalamide, is a nonionic, water-soluble radiographic contrast medium with a molecular weight of 821.14 (iodine content 46.36%). In aqueous solution each triiodinated molecule remains undissociated. The chemical structure is: OMNIPAQUE is provided as a sterile, pyrogen-free, colorless to pale-yellow solution, in the following iodine concentrations: 140, 180, 240, 300, and 350 mgI/mL. OMNIPAQUE 140 contains 302 mg of iohexol equivalent to 140 mg of organic iodine per mL; OMNIPAQUE 180 contains 388 mg of iohexol equivalent to 180 mg of organic iodine per mL; OMNIPAQUE 240 contains 518 mg of iohexol equivalent to 240 mg of organic iodine per mL; OMNIPAQUE 300 contains 647 mg of iohexol equivalent to 300 mg of organic iodine per mL; and OMNIPAQUE 350 contains 755 mg of iohexol equivalent to 350 mg of organic iodine per mL. Each milliliter of iohexol solution contains 1.21 mg tromethamine and 0.1 mg edetate calcium disodium with the pH adjusted between 6.8 and 7.7 with hydrochloric acid or sodium hydroxide. All solutions are sterilized by autoclaving and contain no preservatives. Unused portions must be discarded. Iohexol solution is sensitive to light and therefore should be protected from exposure. 1 Reference ID: 4080358 The available concentrations have the following physical properties: Absolute Concentration Osmolality* Osmolarity Viscosity Specific (mgI/mL) (mOsm/kg water) (mOsm/L) (cp) Gravity 20°C 37°C 37°C 140 322 273 2.3 1.5 1.164 180 408 331 3.1 2.0 1.209 240 520 391 5.8 3.4 1.280 300 672 465 11.8 6.3 1.349 350 844 541 20.4 10.4 1.406 * By vapor-pressure osmometry. -

Utilisation De La Prémédication Pour La Prévention Des Réactions D’Hypersensibilité Lors D’Un Examen D’Imagerie Médicale Avec Injection D’Un Agent De Contraste Iodé
Utilisation de la prémédication pour la prévention des réactions d’hypersensibilité lors d’un examen d’imagerie médicale avec injection d’un agent de contraste iodé Rapport d’examen rapide 01-19 Unité d’évaluation des technologies et des modes d’intervention en santé (UETMIS) Janvier 2019 Unité d’évaluation des technologies et des modes d’intervention en santé UETMIS Utilisation de la prémédication pour la prévention des réactions d’hypersensibilité lors d’un examen d’imagerie médicale avec injection d’un agent de contraste iodé Rapport d’examen rapide 01-2019 préparé par Sylvain L’Espérance, Ph.D. Brigitte Larocque, M.A. Martin Coulombe, M.Sc., M.A.P. Marc Rhainds, MD, M.Sc., FRCPC UETMIS, CHU de Québec-Université Laval Janvier 2019 Direction de la qualité, de l’évaluation, de l'éthique et des affaires institutionnelles (DQEEAI) https://www.chudequebec.ca/professionnels-de-la-sante/evaluation/evaluation.aspx Le contenu de cette publication a été rédigé et édité par l’Unité d’évaluation des technologies et des modes d’intervention en santé (UETMIS) du CHU de Québec-Université Laval. COORDINATION Dr Marc Rhainds, cogestionnaire médical et scientifique, UETMIS M. Martin Coulombe, adjoint au directeur – Évaluation, expérience patient et éthique, Direction de la qualité, de l’évaluation, de l’éthique et des affaires institutionnelles (DQEEAI) SECRÉTARIAT ET MISE EN PAGE Mme Awa Dieng, adjointe administrative, module Évaluation et expérience patient, DQEEAI Pour se renseigner sur cette publication ou toute autre activité de l’UETMIS, s’adresser à : Unité d’évaluation des technologies et des modes d’intervention en santé Hôpital Saint-François d'Assise du CHU de Québec-Université Laval 10, rue de l’Espinay Québec (Québec) G1L 3L5 Téléphone : 418 525-4444 poste 54682 Courriel : [email protected] Comment citer ce document : Unité d’évaluation des technologies et des modes d’intervention en santé (UETMIS) du CHU de Québec-Université Laval. -

Guidelines on the Use of Iodinated Contrast Media in Patients with Kidney Disease 2012 – Digest Version – JSN, JRS and JCS Joint Working Group
Circulation Journal JCS GUIDELINES Official Journal of the Japanese Circulation Society http://www.j-circ.or.jp Guidelines on the Use of Iodinated Contrast Media in Patients With Kidney Disease 2012 – Digest Version – JSN, JRS and JCS Joint Working Group Table of Contents Abbreviations ∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙ 1884 CQ IV-3: Does the risk for developing CIN differ I Outline of the Digest Version of Guidelines between iso- and low-osmolar contrast media? ∙∙∙∙∙∙∙∙∙∙ 1893 on the Use of Iodinated Contrast Media in CQ IV-4: Does the risk for developing CIN differ among Patients With Kidney Disease ∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙ 1884 different low-osmolar contrast media? ∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙ 1893 1. Purpose of the Guidelines ∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙ 1884 CQ IV-5: Is the risk for developing CIN higher in patients 2. A Cautionary Note on the Use of the Present receiving contrast media via invasive (intra-arterial) Guidelines ∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙ 1885 administration than in those receiving contrast media 3. Selection of Literature, Levels of Evidence, and via non-invasive (intravenous) administration? ∙∙∙∙∙∙∙∙∙∙∙ 1896 Grades of Recommendations ∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙ 1885 V Invasive Diagnostic Imaging Including 4. Independent Assessment ∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙ 1885 Cardiac Angiography or Percutaneous 5. Future Plans ∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙ 1885 Catheter Intervention -
Ligand Presents Positive Results from Phase 1 Clinical Trial of Captisol-Enabled Iohexol
November 8, 2019 Ligand Presents Positive Results from Phase 1 Clinical Trial of Captisol-enabled Iohexol Presentation at the American Society of Nephrology (ASN) Kidney Week 2019 SAN DIEGO--(BUSINESS WIRE)-- Ligand Pharmaceuticals Incorporated (NASDAQ: LGND) presented positive results today from a Phase 1 clinical trial of its Captisol-enabled (CE) Iohexol program at ASN Kidney Week 2019 in Washington, D.C. The CE-Iohexol program was established in January 2018 to develop a Captisol-enabled, next-generation contrast agent for diagnostic imaging with a reduced risk of renal toxicity. The trial achieved the primary endpoint demonstrating pharmacokinetic bioequivalence between CE-Iohexol injection and a reference Iohexol injection (OMNIPAQUE™) after intravenous (IV) administration in healthy adults. CE-Iohexol injection was safe and well tolerated, and adverse events were in line with the known safety profile of OMNIPAQUE. Contrast agents are used to enhance diagnostic imaging. Despite their benefits and widespread use, contrast agents may place patients at an increased risk for acute kidney injury (AKI), especially those with certain risk factors undergoing cardiac interventional procedures utilizing intravascular iodinated contrast.1 CE-Iohexol is designed to reduce the risk of AKI during imaging procedures where iodinated contrast agents are administered. In preclinical studies using an animal model of AKI, CE-Iohexol administered at a dose similar to the clinical usage of iohexol in humans significantly reduced renal injury compared to iohexol alone and increased survival from 50% to 88%.2 The goal of the Phase 1 trial was to establish pharmacokinetic bioequivalence to support subsequent clinical trials that could support the submission of a 505(b)(2) new drug application (NDA) to the U.S. -
Allergic Reactions Following Contrast Material Administration: Nomenclature, Classification, and Mechanisms
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by RERO DOC Digital Library Int J Legal Med (2014) 128:95–103 DOI 10.1007/s00414-013-0912-x REVIEW ARTICLE Allergic reactions following contrast material administration: nomenclature, classification, and mechanisms Cristian Palmiere & Lionel Comment & Patrice Mangin Received: 30 July 2013 /Accepted: 3 September 2013 /Published online: 24 September 2013 # Springer-Verlag Berlin Heidelberg 2013 Abstract In forensic pathology routine, fatal cases of contrast Several drugs have been implicated as causing adverse reac- agent exposure can be occasionally encountered. In such tions, some potentially life-threatening. Reactions to situations, beyond the difficulties inherent in establishing the radiocontrast media, magnetic resonance imaging (MRI) contrast cause of death due to nonspecific or absent autopsy and agents, and contrast material used in neurosurgery as well as histology findings as well as limited laboratory investigations, ophthalmic surgery represent a portion of adverse drug reactions. pathologists may face other problems in formulating exhaus- In the medicolegal setting, fatal cases of contrast agent tive, complete reports, and conclusions that are scientifically exposure can be occasionally encountered. In these situations, accurate. Indeed, terminology concerning adverse drug reac- beyond the classical problems inherent in establishing the tions and allergy nomenclature is confusing. Some terms, still cause of death that are related to nonspecific or absent mac- utilized in forensic and radiological reports, are outdated and roscopic and microscopic findings as well as limited, reliable should be avoided. Additionally, not all forensic pathologists laboratory investigation tools, forensic pathologists may face master contrast material classification and pathogenesis of difficulties in formulating exhaustive reports and conclusions. -
United States Patent (19) 11 Patent Number: 6,086,851 Boni Et Al
US006086851A United States Patent (19) 11 Patent Number: 6,086,851 Boni et al. (45) Date of Patent: *Jul. 11, 2000 54 PHARMACEUTICAL COMPOSITIONS OTHER PUBLICATIONS CONTAINING INTERDIGITATION-FUSION 66 LIPOSOMES AND GELS Ames, et al., “The Role of Polyamines in the Neutralization of Bacteriophage Deoxyribonucleic Acid”, 1960, J. Biol. 75 Inventors: Lawrence T. Boni, Monmouth Chem. 235, 3,769–775. Junction, N.J.; Andrew S. Janoff, Bally, et al., “Dopamine accumulation in large unilamellar Yardley, Pa.; Sharma R. Minchey; vesicles Systems induced by transmembrane ion gradients', Walter R. Perkins, both of Monmouth S. Chen Phys' lipids, 47 97.07. Junction, N.J.; Christine E. Swenson, Boni, et al., “Aggregation and Fusion of Unilamellar Princeton Junction, N.J.; Patrick L. Sis by Poly(Ethylene Glycol)”, BBA 775, 1984, Ahl, Princeton, N.J.; Thomas S. Davis, Chapman, et al., “Physical Studies of Phospholipids..., X. The Valhalla, N.Y. Effect of Sonication on Aqueous Dispersions of Egg Yolk Lecithin', BBA, 163, 255, 1968. 73 ASSignee: The Liposome Company, Inc., Chen, et al., “Micro-determination of Phosphorous”, 1956, Princeton, N.J. Analytical Chem., 28, 11, 1756. Chong, P., et al. “A Differential Polarized Phase Fluoromet (*) Notice: This patent is subject to a terminal dis- ric Study of the Effects of High Hydrostatic Pressure upon claimer. the Fluidity of Cellular Membranes”, Biochemistry 1983, 22, 409–415. 21 Appl. No.: 08/881,651 Eum, et al., “Temperature-Induced Fusion of Small Unila mellar Vesicles Formed from Saturated Long-Chain Leci 22 Filed: Jun. 24, 1997 thins and Diheptanolyphosphatidylcholine”, Biochem., O O 1989, 28:8206–8213.