Reactions to Radiocontrast Media and Its Managment
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Xx250 Spc 2015 Uk
SUMMARY OF PRODUCT CHARACTERISTICS 1 NAME OF THE MEDICINAL PRODUCT XENETIX 250 (250 mgI/ml) Solution for injection. 2 QUALITATIVE AND QUANTITATIVE COMPOSITION per ml 50 ml 100 ml 200 ml 500 ml Iobitridol (INN) 548.4 mg 27.42 g 54.84 g 109.68 g 274.2 g Iodine corresponding to 250 mg 12.5 g 25 g 50 g 125 g Excipient with known effect : Sodium (up to 3.5 mg per 100 mL). For the full list of excipients, see section 6.1. 3 PHARMACEUTICAL FORM Solution for injection. Clear, colourless to pale yellow solution 4. CLINICAL PARTICULARS 4.1. Therapeutic indications For adults and children undergoing: . whole-body CT . venography . intra-arterial digital subtraction angiography . ERP/ERCP This medicinal product is for diagnostic use only. 4.2. Posology and method of administration The dosage may vary depending on the type of examination, the age, weight, cardiac output and general condition of the patient and the technique used. Usually the same iodine concentration and volume are used as with other iodinated X-ray contrast in current use. As with all contrast media, the lowest dose necessary to obtain adequate visualisation should be used. Adequate hydration should be assured before and after administration as for other contrast media. As a guideline, the recommended dosages are as follows: Indications Recommended dosage Whole-body CT The doses of contrast medium and the rates of administration depend on the organs under investigation, the diagnostic problem and, in particular, the different scan and image-reconstruction times of the scanners in use. -

Pharmacologyonline 2: 727-753 (2010) Ewsletter Bradu and Rossini
Pharmacologyonline 2: 727-753 (2010) ewsletter Bradu and Rossini COTRAST AGETS - IODIATED PRODUCTS. SECOD WHO-ITA / ITA-OMS 2010 COTRIBUTIO O AGGREGATE WHO SYSTEM-ORGA CLASS DISORDERS AD/OR CLUSTERIG BASED O REPORTED ADVERSE REACTIOS/EVETS Dan Bradu and Luigi Rossini* Servizio Nazionale Collaborativo WHO-ITA / ITA-OMS, Università Politecnica delle Marche e Progetto di Farmacotossicovigilanza, Azienda Ospedaliera Universitaria Ospedali Riuniti di Ancona, Regione Marche, Italia Summary From the 2010 total basic adverse reactions and events collected as ADRs preferred names in the WHO-Uppsala Drug Monitoring Programme, subdivided in its first two twenty years periods as for the first seven iodinated products diagnostic contrast agents amidotrizoate, iodamide, iotalamate, iodoxamate, ioxaglate, iohexsol and iopamidol, their 30 WHO-system organ class disorders (SOCDs) aggregates had been compared. Their common maximum 97% levels identified six SOCDs only, apt to evaluate the most frequent single ADRs for each class, and their percentual normalization profiles for each product. The WILKS's chi square statistics for the related contingency tables, and Gabriel’s STP procedure applied to the extracted double data sets then produced profile binary clustering, as well as Euclidean confirmatory plots. They finally showed similar objectively evaluated autoclassificative trends of these products, which do not completely correspond to their actual ATC V08A A, B and C subdivision: while amidotrizoate and iotalamate, and respectively iohesol and iopamidol are confirmed to belong to the A and B subgroups, ioxaglate behaves fluctuating within A, B and C, but iodamide looks surprizingly, constantly positioned together with iodoxamate as binary/ternary C associated. In view of the recent work of Campillos et al (Science, 2008) which throws light on the subject, the above discrepancies do not appear anymore unexpected or alarming. -

ACR Manual on Contrast Media
ACR Manual On Contrast Media 2021 ACR Committee on Drugs and Contrast Media Preface 2 ACR Manual on Contrast Media 2021 ACR Committee on Drugs and Contrast Media © Copyright 2021 American College of Radiology ISBN: 978-1-55903-012-0 TABLE OF CONTENTS Topic Page 1. Preface 1 2. Version History 2 3. Introduction 4 4. Patient Selection and Preparation Strategies Before Contrast 5 Medium Administration 5. Fasting Prior to Intravascular Contrast Media Administration 14 6. Safe Injection of Contrast Media 15 7. Extravasation of Contrast Media 18 8. Allergic-Like And Physiologic Reactions to Intravascular 22 Iodinated Contrast Media 9. Contrast Media Warming 29 10. Contrast-Associated Acute Kidney Injury and Contrast 33 Induced Acute Kidney Injury in Adults 11. Metformin 45 12. Contrast Media in Children 48 13. Gastrointestinal (GI) Contrast Media in Adults: Indications and 57 Guidelines 14. ACR–ASNR Position Statement On the Use of Gadolinium 78 Contrast Agents 15. Adverse Reactions To Gadolinium-Based Contrast Media 79 16. Nephrogenic Systemic Fibrosis (NSF) 83 17. Ultrasound Contrast Media 92 18. Treatment of Contrast Reactions 95 19. Administration of Contrast Media to Pregnant or Potentially 97 Pregnant Patients 20. Administration of Contrast Media to Women Who are Breast- 101 Feeding Table 1 – Categories Of Acute Reactions 103 Table 2 – Treatment Of Acute Reactions To Contrast Media In 105 Children Table 3 – Management Of Acute Reactions To Contrast Media In 114 Adults Table 4 – Equipment For Contrast Reaction Kits In Radiology 122 Appendix A – Contrast Media Specifications 124 PREFACE This edition of the ACR Manual on Contrast Media replaces all earlier editions. -

Review Article Contrast Media Viscosity Versus Osmolality in Kidney Injury: Lessons from Animal Studies
Hindawi Publishing Corporation BioMed Research International Volume 2014, Article ID 358136, 15 pages http://dx.doi.org/10.1155/2014/358136 Review Article Contrast Media Viscosity versus Osmolality in Kidney Injury: Lessons from Animal Studies Erdmann Seeliger, Diana C. Lenhard, and Pontus B. Persson Institute of Physiology and Center for Cardiovascular Research, Charite-University´ Medicine Berlin, Campus Mitte, Hessische Straße 3-4, 10115 Berlin, Germany Correspondence should be addressed to Erdmann Seeliger; [email protected] Received 18 October 2013; Accepted 29 December 2013; Published 23 February 2014 Academic Editor: Richard Solomon Copyright © 2014 Erdmann Seeliger et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. Iodinated contrast media (CM) can induce acute kidney injury (AKI). CM share common iodine-related cytotoxic features but differ considerably with regard to osmolality and viscosity. Meta-analyses of clinical trials generally failed to reveal renal safety differences of modern CM with regard to these physicochemical properties. While most trials’ reliance on serum creatinine as outcome measure contributes to this lack of clinical evidence, it largely relies on the nature of prospective clinical trials: effective prophylaxis by ample hydration must be employed. In everyday life, patients are often not well hydrated; here we lack clinical data. However, preclinical studies that directly measured glomerular filtration rate, intrarenal perfusion and oxygenation, and various markers of AKI have shown that the viscosity of CM is of vast importance. In the renal tubules, CM become enriched, as water is reabsorbed, but CM are not. -

When Is the Use of Contrast Media in Chest CT Indicated? Bruno Hochhegger1,2,3, Robson Rottenfusser4,5, Edson Marchiori6
J Bras Pneumol. 2017;43(5):400-400 http://dx.doi.org/10.1590/S1806-37562017000000179 LETTER TO THE EDITOR When is the use of contrast media in chest CT indicated? Bruno Hochhegger1,2,3, Robson Rottenfusser4,5, Edson Marchiori6 TO THE EDITOR: nodule, small or large airway disease, and lung cancer screening, do not require the use of any contrast media. It is undeniable that CT plays an important role in the diagnosis and treatment of various clinical conditions However, for the assessment of vascular disease, CT involving the chest wall, mediastinum, pleura, pulmonary requires the use of an i.v. contrast agent to delineate the arteries, and lung parenchyma. The need for enhancement vessel lumen (e.g., aneurysm, dissection, and vascular using i.v. contrast media depends on the specific clinical tumor invasion). Pulmonary embolic disease is the third indication.(1-3) The most common contrast agents used most common cause of acute cardiovascular disease.(3,5) with CT imaging are iodinated. Intravenous iodinated Chest CT angiography is the most common way to assess contrast agents are used for opacification of vascular for pulmonary embolic disease because, in addition to structures. The major families of contrast agents are being accurate, fast, and widely available, it can assess ionic and nonionic. Contrast agents can be further alternate pathologies in cases of undifferentiated chest classified as high- or low-osmolality agents on the basis pain. Typically, the use of CT in order to investigate of the iodine concentration. Most centers use nonionic vascular disease or pleural pathology may include contrast agents (generally low-osmolality agents) for non-contrast-enhanced images to identify hemorrhage, i.v. -

Proceedings of the Fifty-Eighth Annual Meeting of the American Society for Clinical Investigation, Inc., Held in Atlantic City, N.J., May 2, 1966: Abstracts
Proceedings of the Fifty-Eighth Annual Meeting of the American Society for Clinical Investigation, Inc., Held in Atlantic City, N.J., May 2, 1966: Abstracts J Clin Invest. 1966;45(6):980-1037. https://doi.org/10.1172/JCI105414. Research Article Find the latest version: https://jci.me/105414/pdf ABSTRACTS Comparison of Effects of Alpha Adrenergic Blockade luminescence. Inhibition of ATPase activities by ouabain, on Resistance and Capacitance Vessels. FRANCOIS parachloromercuribenzoate (PCMB), and parachloro- M. ABBOUD * AND JOHN W. ECKSTEIN,* Iowa City, mercuribenzenesulfonate (PCMBS) was studied. ¶1 Mem- Iowa. brane ATPase of osmotically prepared platelet "ghosts" A foreleg of each of 20 dogs was perfused with blood is composed of Na+-K+-Mg++-dependent ATPase (15 to at a constant rate through the brachial artery. The 30%) and Mg++-activated ATPase (60 to 85%o). Ouabain nerves of the brachial plexus were transected, and an (10' M), which inhibits the Na+-K--dependent ATPase electrode was applied to their distal ends. Pressures were activity and produces a resultant loss of cellular K+, gain recorded simultaneously from the brachial artery and of Na+, and cell swelling, does not inhibit either ADP cephalic vein and from a small artery and small vein in aggregation or clot retraction. ¶f PCMB, an organic the paw. Pressor responses to injections of nor- mercurial compound that diffuses into cells, totally inacti- epinephrine (1, 2, and 4 /.tg) into the brachial artery and vates both ATPase activities in the ghost preparations to nerve stimulation (3, 6, and 12 cps) were measured and in the intact platelet. -

Evaluation Report Radiocontrast Agents
Evaluation report Radiocontrast agents Report No. 187 Within the strategy aimed at reducing micro-pollutant inputs originating from ur- ban and industrial waste water, evaluation reports are being drafted for 10 groups of substances targeted at summarizing scientifi c and technical facts and at pointing out gaps of knowledge. Also, the evaluation reports present a variety of possible mea- sures at the source (e.g. registration of substances, limitation of uses) and technical measures in crucial wastewater treatment plants (e.g. introducing a further treatment stage). The “Conclusions” of the evaluation reports list the most effi cient measures to be further investigated into within a holistic ICPR strategy. However, these measures are no recommendations the ICPR addresses to its member states. Measures listed in this chapter will be integrated into a survey report of all measures in order to be able to take into account eventual synergetic effects of measures (effects of measures on different groups of substances) when proceeding with the fi nal evaluation. Based on the fi nal evaluation of all measures the ICPR will determine recommendations for the Member States Imprint Publisher: International Commission for the Protection of the Rhine (ICPR) Kaiserin-Augusta-Anlagen 15, D 56068 Koblenz P.O. box 20 02 53, D 56002 Koblenz Telephone +49-(0)261-94252-0, Fax +49-(0)261-94252-52 Email: [email protected] www.iksr.org ISBN 935324-53-7 © IKSR-CIPR-ICBR 2010 IKSR CIPR ICBR Evaluation report Radiocontrast agents 1. Introduction Radiocontrast agents are used for diagnostic purposes, as they absorb X-rays to a greater extent than human soft tissue and thus visualize these tissues. -

Iodinated Contrast Media and Their Adverse Reactions*
Iodinated Contrast Media and Their Adverse Reactions* Jagdish Singh and Aditya Daftary Teleradiology Solutions, Bangalore, India acteristics, including their chemical structure, osmolality, Cross-use of technology between nuclear medicine and radiol- iodine content, and ionization in solution (2,3). ogy technologists is expanding. The growth of PET/CT and the The parent molecule from which the contrast agents are increasing use of intravenous contrast agents during these pro- derived is benzene. This is a toxic water-insoluble liquid. cedures bring the nuclear medicine technologist into direct con- The carbon atoms on a benzene ring are numbered clock- tact with these agents and their associated complications. A basic understanding of the occurrence, risk factors, clinical fea- wise from 1 to 6. Benzoic acid is produced by introducing tures, and management of these procedures is of increasing an acid group at position 1 on the benzene ring. This acid importance to the nuclear medicine technologist. After reading group permits the formation of salts or amides, which this article, the technologist will be able to list the factors that influence water solubility. 2,4,6-triiodobenzoic acid is ob- increase the risk of contrast reactions; understand ways to min- tained by introducing iodine atoms at positions 2, 4, and 6 imize the occurrence of contrast reactions; and develop a plan to on the ring. Iodine is the element used in contrast media identify, treat, and manage the reactions effectively. as it possesses 3 important properties essential for the Key Words: iodinated contrast media; contrast reactions production of contrast media: high-contrast density, firm J Nucl Med Technol 2008; 36:69–74 binding to the benzene molecule, and low toxicity. -
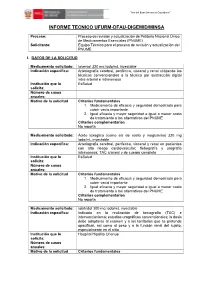
Informe Tecnico Ufurm-Dfau-Digemid/Minsa
“Año del Buen Servicio al Ciudadano” ” INFORME TECNICO UFURM-DFAU-DIGEMID/MINSA Proceso: Proceso de revisión y actualización de Petitorio Nacional Único de Medicamentos Esenciales (PNUME) Solicitante: Equipo Técnico para el proceso de revisión y actualización del PNUME I. DATOS DE LA SOLICITUD Medicamento solicitado: Ioversol 320 mg Iodo/mL inyectable Indicación específica: Arteriografía cerebral, periférica, visceral y renal utilizando las técnicas convencionales o la técnica por sustracción digital intra-arterial e intravenosa Institución que lo EsSalud solicita: Número de casos anuales: Motivo de la solicitud Criterios fundamentales 1. Medicamento de eficacia y seguridad demostrada para cubrir vacío importante. 2. Igual eficacia y mayor seguridad e igual o menor costo de tratamiento a las alternativas del PNUME Criterios complementarios No reporta Medicamento solicitado: Ácido ioxaglico (como sal de sodio y meglumina) 320 mg Iodo/mL inyectable Indicación específica: Arteriografia cerebral, periferica, visceral y renal en pacientes con alto riesgo cardiovascular; flebografía y urografía intravenosa; TAC craneal y de cuerpo completo Institución que lo EsSalud solicita: Número de casos anuales: Motivo de la solicitud Criterios fundamentales 1. Medicamento de eficacia y seguridad demostrada para cubrir vació importante. 2. Igual eficacia y mayor seguridad e igual o menor costo de tratamiento a las alternativas del PNUME Criterios complementarios No reporta Medicamento solicitado: Iobitridol 300 mg Iodo/mL inyectable Indicación específica: Indicado en la realización de tomografía (TAC) e intervencionismo; estudios urográficos convencionales; la dosis debe adaptarse al examen y a los territorios que se pretende opacificar, asi como al peso y a la función renal del sujeto, especialmente en el niño Institución que lo Hospital Hipólito Unanue solicita: Número de casos anuales: Motivo de la solicitud Criterios fundamentales “Año del Buen Servicio al Ciudadano” ” 1. -

Radiocontrast Agent Diatrizoic Acid Induces Mitophagy and Oxidative Stress Via Calcium Dysregulation
International Journal of Molecular Sciences Article Radiocontrast Agent Diatrizoic Acid Induces Mitophagy and Oxidative Stress via Calcium Dysregulation Dakota B. Ward, Kathleen C. Brown and Monica A. Valentovic * Department of Biomedical Sciences, Toxicology Research Cluster, Joan C. Edwards School of Medicine, Marshall University, 1 Marshall Drive, Huntington, WV 25755, USA * Correspondence: [email protected]; Tel.: +1-304-696-7332; Fax: +1-304-696-7391 Received: 20 May 2019; Accepted: 18 August 2019; Published: 21 August 2019 Abstract: Contrast-induced acute kidney injury (CI-AKI) is the third most common cause of hospital associated kidney damage. Potential mechanisms of CI-AKI may involve diminished renal hemodynamics, inflammatory responses, and direct cytotoxicity. The hypothesis for this study is that diatrizoic acid (DA) induces direct cytotoxicity to human proximal tubule (HK-2) cells via calcium dysregulation, mitochondrial dysfunction, and oxidative stress. HK-2 cells were exposed to 0–30 mg I/mL DA or vehicle for 2–24 h. Conversion of 3-(4,5-dimethylthiazol-2-yl)-2,5-diphenyltetrazolium bromide (MTT) and trypan blue exclusion indicated a decrease in mitochondrial and cell viability within 2 and 24 h, respectively. Mitochondrial dysfunction was apparent within 8 h post exposure to 15 mg I/mL DA as shown by Seahorse XF cell mito and Glycolysis Stress tests. Mitophagy was increased at 8 h by 15 mg I/mL DA as confirmed by elevated LC3BII/I expression ratio. HK-2 cells pretreated with calcium level modulators BAPTA-AM, EGTA, or 2-aminophenyl borinate abrogated DA-induced mitochondrial damage. DA increased oxidative stress biomarkers of protein carbonylation and 4-hydroxynonenol (4HNE) adduct formation. -

Iodinated Contrast Media Guideline
IODINATED CONTRAST MEDIA GUIDELINE FACULTY OF CLINICAL RADIOLOGY THE ROYAL AUSTRALIAN AND NEW ZEALAND COLLEGE OF RADIOLOGISTS® Name of document and version: Iodinated Contrast Media Guideline, V2.3 Approved by: Faculty of Clinical Radiology Date of approval: March 2018 Suggested Citation: The Royal Australian and New Zealand College of Radiologists. Iodinated Contrast Media Guideline. Sydney: RANZCR; 2018. ABN 37 000 029 863 Copyright for this publication rests with The Royal Australian and New Zealand College of Radiologists ® The Royal Australian and New Zealand College of Radiologists Level 9, 51 Druitt Street Sydney NSW 2000 Australia Email: [email protected] Website: www.ranzcr.edu.au Telephone: +61 2 9268 9777 Disclaimer: The information provided in this document is of a general nature only and is not intended as a substitute for medical or legal advice. It is designed to support, not replace, the relationship that exists between a patient and his/her doctor. Document name Iodinated Contrast Media Guideline Description The Iodinated Contrast Media Guideline is intended to assist The Royal Australian and New Zealand College of Radiologists®, its staff, Fellows, members and other individuals involved in the administration of iodinated contrast media to patients undergoing medical imaging procedures. Created By Standards of Practice and Accreditation Committee Date Created 2011 Maintained By Faculty of Clinical Radiology, Policy and Advocacy Unit Version Number Modifications Made Date Modified 2011 Document published 2.0 Document updated and published April 2016 2.1 Grammatical error corrected in R31 February 2017 2.2 Nitroglycerin dosages corrected in R39 June 2017 2.3 Adrenaline dosage corrected in R56 March 2018 Iodinated Contrast Media Guideline, V2.3 © The Royal Australian and New Zealand College of Radiologists® March 2018 Page 2 of 39 TABLE OF CONTENTS 1. -

(320 Mg I/Ml), Solution for Injection Meglumine Ioxaglate and Sodium Ioxaglate
HEXABRIX 320 (320 mg I/mL), solution for injection Meglumine ioxaglate and sodium ioxaglate Read all of this leaflet carefully before you start using this medicine. Keep this leaflet. You may need to read it again. If you have any further questions, ask your doctor or pharmacist. This medicine has been prescribed for you. Do not pass it on to others. It may harm them, even if their symptoms are the same as yours. If any of the side effects gets serious, or if you notice any side effects not listed in this leaflet, please tell your doctor or pharmacist. In this leaflet: 1. What HEXABRIX 320, solution for injection is and what it is used for 2. What you need to know before you use HEXABRIX 320, solution for injection 3. How to use HEXABRIX 320, solution for injection 4. Possible side effects 5. How to store HEXABRIX 320, solution for injection 6. Contents of the pack and other information 1. WHAT HEXABRIX 320 IS AND WHAT IT IS USED FOR HEXABRIX 320 is a contrast agent. It belongs to the group of contrast agents used for radiological examinations. HEXABRIX 320 is used to enhance the contrast of the images obtained during these examinations, in order to improve the visualisation and delineation of certain parts of the body, such as: Certain hollow organs (opacification of body cavities), The uterus and fallopian tubes (ducts connecting the uterus to the ovaries) in female patients (hysterosalpingography), Blood vessels (angiography), Joints (arthrography), Urinary system (urography). This medicine is for diagnostic use only. 2.