Periodontitis and the Elderly: an Overview of the Disease and Its Impact on an Aging
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Importance of Chlorhexidine in Maintaining Periodontal Health
International Journal of Dentistry Research 2016; 1(1): 31-33 Review Article Importance of Chlorhexidine in Maintaining Periodontal IJDR 2016; 1(1): 31-33 December Health © 2016, All rights reserved www.dentistryscience.com Dr. Manpreet Kaur*1, Dr. Krishan Kumar1 1 Department of Periodontics, Post Graduate Institute of Dental Sciences, Rohtak-124001, Haryana, India Abstract Plaque is responsible for periodontal diseases. In order to prevent occurrence and progression of periodontal disease, removal of plaque becomes important. Mechanical tooth cleaning aids such as toothbrushes, dental floss, interdental brushes are used for removal of plaque. However, in some cases, chemical agents are used as an adjunct to mechanical methods to facilitate plaque control and prevent gingivitis. Chlorhexidine (CHX) mouthwash is the most commonly used and is considered as gold standard chemical agent. In this review, mechanism of action and other properties of CHX are discussed. Keywords: Plaque, Chemical agents, Chlorhexidine (CHX). INTRODUCTION Dental plaque is primary etiologic factor responsible for gingivitis and periodontitis [1]. Mechanical plaque control using toothbrushes, interdental brushes, dental floss prevent occurrence of gingivitis. However, in majority of population, mechanical methods of plaque control are ineffective due to less time spent[2] for plaque removal and lack of consistency. These limitations necessitate use of chemical plaque control agents as an adjunct to mechanical plaque control. Among various chemical agents, chlorhexidine (CHX) is considered to be a gold standard chemical agent for plaque control. Its structural formula consists of two symmetric 4-chlorophenyl rings and two biguanide groups connected by a central hexamethylene chain. Mechanism of action for CHX CHX is bactericidal and is effective against gram-positive bacteria, gram-negative bacteria and yeast organisms. -

DENTIN HYPERSENSITIVITY: Consensus-Based Recommendations for the Diagnosis & Management of Dentin Hypersensitivity
October 2008 | Volume 4, Number 9 (Special Issue) DENTIN HYPERSENSITIVITY: Consensus-Based Recommendations for the Diagnosis & Management of Dentin Hypersensitivity A Supplement to InsideDentistry® Published by AEGISPublications,LLC © 2008 PUBLISHER Inside Dentistry® and De ntin Hypersensitivity: Consensus-Based Recommendations AEGIS Publications, LLC for the Diagnosis & Management of Dentin Hypersensitivity are published by AEGIS Publications, LLC. EDITORS Lisa Neuman Copyright © 2008 by AEGIS Publications, LLC. Justin Romano All rights reserved under United States, International and Pan-American Copyright Conventions. No part of this publication may be reproduced, stored in a PRODUCTION/DESIGN Claire Novo retrieval system or transmitted in any form or by any means without prior written permission from the publisher. The views and opinions expressed in the articles appearing in this publication are those of the author(s) and do not necessarily reflect the views or opinions of the editors, the editorial board, or the publisher. As a matter of policy, the editors, the editorial board, the publisher, and the university affiliate do not endorse any prod- ucts, medical techniques, or diagnoses, and publication of any material in this jour- nal should not be construed as such an endorsement. PHOTOCOPY PERMISSIONS POLICY: This publication is registered with Copyright Clearance Center (CCC), Inc., 222 Rosewood Drive, Danvers, MA 01923. Permission is granted for photocopying of specified articles provided the base fee is paid directly to CCC. WARNING: Reading this supplement, Dentin Hypersensitivity: Consensus-Based Recommendations for the Diagnosis & Management of Dentin Hypersensitivity PRESIDENT / CEO does not necessarily qualify you to integrate new techniques or procedures into your practice. AEGIS Publications expects its readers to rely on their judgment Daniel W. -

Assessment of Efficacy of Chlorhexidine Chip As an Adjunct to Scaling and Root Planning Using N-Benzoyl- DL-Arginine-2-Naphthylamide Test Kit
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by Asian Pacific Journal of Health Sciences e-ISSN: 2349-0659 p-ISSN: 2350-0964 ORGINAL ARTICLE doi: 10.21276/apjhs.2018.5.2.21 Assessment of efficacy of chlorhexidine chip as an adjunct to scaling and root planning using N-benzoyl- DL-arginine-2-naphthylamide test kit Malvika Singh*, Rajan Gupta, Parveen Dahiya, Mukesh Kumar, Rohit Bhardwaj Department of Periodontics, Himachal Institute of Dental Sciences, Paonta Sahib, Sirmaur, Himachal Pradesh, India ABSTRACT Background: With increasing advances in the field of medicine, diagnosing a disease has been an easy task and periodontitis is no exception to this. N-benzoyl-DL-arginine-2-naphthylamide (BANA) test is a modern chair-side paraclinical method designed to detect the presence of one or more anaerobic bacteria commonly associated with periodontal disease, namely Treponema denticola, Porphyromonas gingivalis, and Tannerella forsythia in subgingival plaque samples taken from periodontally diseased teeth. Aim: The aim of the study was to assess the efficacy of chlorhexidine chip as an adjunct to scaling and root planning (SRP), using BANA Test Kit. Materials and Methods: A total of 20 chronic periodontitis patients (aged 35–55 years) having pocket depth of ≥5 mm in molar teeth were selected and randomly divided into following treatment groups: Group I: SRP and Group II: SRP along with chlorhexidine chip. The clinical and microbial parameters were recorded at baseline and 1 and 3 months post-treatment. BANA chairside test was used for estimation of specific microbiota. Statistical analysis used: Mann–Whitney test, Wilcoxon signed test, t-test, Pearson’s Chi-square test, and variability test were used. -

Probiotic Alternative to Chlorhexidine in Periodontal Therapy: Evaluation of Clinical and Microbiological Parameters
microorganisms Article Probiotic Alternative to Chlorhexidine in Periodontal Therapy: Evaluation of Clinical and Microbiological Parameters Andrea Butera , Simone Gallo * , Carolina Maiorani, Domenico Molino, Alessandro Chiesa, Camilla Preda, Francesca Esposito and Andrea Scribante * Section of Dentistry–Department of Clinical, Surgical, Diagnostic and Paediatric Sciences, University of Pavia, 27100 Pavia, Italy; [email protected] (A.B.); [email protected] (C.M.); [email protected] (D.M.); [email protected] (A.C.); [email protected] (C.P.); [email protected] (F.E.) * Correspondence: [email protected] (S.G.); [email protected] (A.S.) Abstract: Periodontitis consists of a progressive destruction of tooth-supporting tissues. Considering that probiotics are being proposed as a support to the gold standard treatment Scaling-and-Root- Planing (SRP), this study aims to assess two new formulations (toothpaste and chewing-gum). 60 patients were randomly assigned to three domiciliary hygiene treatments: Group 1 (SRP + chlorhexidine-based toothpaste) (control), Group 2 (SRP + probiotics-based toothpaste) and Group 3 (SRP + probiotics-based toothpaste + probiotics-based chewing-gum). At baseline (T0) and after 3 and 6 months (T1–T2), periodontal clinical parameters were recorded, along with microbiological ones by means of a commercial kit. As to the former, no significant differences were shown at T1 or T2, neither in controls for any index, nor in the experimental -

Exam # ___DAPE 731, Periodon
Exam 1-A NAME: _ _____ KEY A & B________________ Seat #: __________________________________ Exam # _________ DAPE 731, Periodontology Year III Dr. Elio Reyes, D.D.S., M.S.D. Dr. Dwight E. McLeod, D.D.S., M.S. October 13, 2009 USE Pencil on Separate Answer Sheet 50 questions multiple choice & true/false – 2 pts each 100 points 3 bonus questions fill in the blank – 1 point each. Total possible points 103 Which periodontal procedure has the specific goal of removing the epithelial lining of the periodontal pocket? A. Periodontal prophylaxis B. Gingival curettage C. Subgingival scaling and root planing D. Gingivoplasty E. None of the above Which one of the following procedures is considered a gingival curettage procedure? A. Gingivectomy B. Subgingival scaling and root planing C. Electrocautery procedure D. Excisional new attachment procedure E. The inverse bevel technique A positive Nikolsky’s sign determines the difference between these conditions: A. Cicatrical pemphigoid / Mucous membrane pemphigoid. B. Mucous membrane pemphigoid/ Pemphigus vulgaris. C. Pemphigus vulgaris/ Stomatitis medicamentosa. D. Stomatitis medicamentosa/ Cicatrical pemphigoid. E. None of the above. Which one of the following conditions is not classified into the “Periodontitis as a manifestation of systemic diseases” category? A. Hematological disorders B. Genetic disorders C. Diabetes mellitus D. A and B E. None of the above In distinguishing “Necrotizing Ulcerative Periodontitis” from “Periodontitis associated with Systemic Diseases”, which of the following factors would best assist you to differentiate? A. The amount of subgingival calculus present. B. Level of the mucogingival junction. C. Presence of pseudomembranous sloughed layer. D. Bleeding upon probing. Identify the tissues that comprise the pocket wall: 1. -

Assessment of a Panel of Risk Indicators in Severe Periodontitis Patients
Assessment of a panel of risk indicators in severe periodontitis patients Ciobanu L.¹, Miricescu D. ², Didilescu A.³, Țărmure V.4 ¹PhD Student in Dental Medicine, Division of Microbiology, Faculty of Dental Medicine, Carol Davila University of Medicine and Pharmacy, Bucharest, Romania ²Senior Lecturer, Division of Biochemistry, Faculty of Dental Medicine, Carol Davila University of Medicine and Pharmacy, Bucharest, Romania ³Professor, Division of Embryology, Faculty of Dental Medicine, Carol Davila University of Medicine and Pharmacy, Bucharest, Romania 4Associate Professor, Department of Orthodontics, Faculty of Dental Medicine, Iuliu Hațieganu University of Medicine and Pharmacy, Cluj-Napoca, Romania Correspondence to: Name: Ciobanu Lidia Address: Blvd. Camil Ressu 49, Bl. H26, Sc. D, Ap.61, Bucharest, Romania Phone: +40 724962500 E-mail address: [email protected] Abstract Aim and objectives The purpose of this study was to analyse a panel of risk indicators in a group of twenty-two patients with severe periodontitis. We also aimed to test possible associations between these indicators and the severity of periodontitis assessed by clinical attachment loss (CAL) mean values. Material and methods Periodontal status was assessed based on the CDC/AAP periodontitis case definition for population-based studies. Risk indicators, including age, gender, weight and height, level of education, and smoking habits, were recorded. Salivary cortisol level, as a marker of chronic stress, was also measured. Results The mean age of the patients was 44.86 (SD 12.81; range 24 to 72). Ten females (45.5%) were enrolled. Testing possible associations between risk indicators and CAL mean values showed no statistical significant correlations, although trends of positive correlations were found between males, BMI, and CAL, respectively Conclusions The present results suggest that a high BMI, as well as masculine gender, could have been important risk factors for severe periodontitis in this study group. -

Instant Update- Getting up to Speed in Periodontics for 2019 Pennsylvania Dental Association Gettysburg Meeting April 6, 2019 F
Instant Update- Getting Up To Speed in Periodontics for 2019 Pennsylvania Dental Association Gettysburg Meeting April 6, 2019 Francis G. Serio, DMD, MS, MBA Diplomate, American Board of Periodontology Staff Dentist, Greene County Health Care, Inc. Course Synopsis Some things change and some things remain the same. The bedrocks of periodontal therapy are time-tested but new approaches to some of these therapies are providing better outcomes for patients. In addition, advances in the science of periodontics have led to both a better understanding of the disease processes and a new classification system for the periodontal diseases and conditions. In addition, as implant dentistry continues to solidify its position, complications are becoming more commonplace. This course will focus on four main areas: The changes in science that have led to the new classification of the periodontal diseases and conditions. Current understanding of the perio-systemic connection. The “semi-surgical” approach to periodontal therapy. Peri-implant mucositis and peri-implantitis and what to do about it. At the end of this presentation, each participant will be able to: Identify the differences between the 1999 and 2017 disease classification systems. Identify key factors and systemic diseases that have a strong association with the periodontal diseases. Develop a “semi-surgical” treatment plan for a patient with periodontitis. Understand the key factors that contribute to peri-implant disease and possible therapeutic approaches. Periodontitis is a disease of the non-mineralized and mineralized connective tissues- What causes and contributes to its breakdown? Bacterial infections vs. Inflammation 1 Statistical vs. Clinical Significance Clinical significance- Jacobson, et al. -

Periodontal Health, Gingival Diseases and Conditions 99 Section 1 Periodontal Health
CHAPTER Periodontal Health, Gingival Diseases 6 and Conditions Section 1 Periodontal Health 99 Section 2 Dental Plaque-Induced Gingival Conditions 101 Classification of Plaque-Induced Gingivitis and Modifying Factors Plaque-Induced Gingivitis Modifying Factors of Plaque-Induced Gingivitis Drug-Influenced Gingival Enlargements Section 3 Non–Plaque-Induced Gingival Diseases 111 Description of Selected Disease Disorders Description of Selected Inflammatory and Immune Conditions and Lesions Section 4 Focus on Patients 117 Clinical Patient Care Ethical Dilemma Clinical Application. Examination of the gingiva is part of every patient visit. In this context, a thorough clinical and radiographic assessment of the patient’s gingival tissues provides the dental practitioner with invaluable diagnostic information that is critical to determining the health status of the gingiva. The dental hygienist is often the first member of the dental team to be able to detect the early signs of periodontal disease. In 2017, the American Academy of Periodontology (AAP) and the European Federation of Periodontology (EFP) developed a new worldwide classification scheme for periodontal and peri-implant diseases and conditions. Included in the new classification scheme is the category called “periodontal health, gingival diseases/conditions.” Therefore, this chapter will first review the parameters that define periodontal health. Appreciating what constitutes as periodontal health serves as the basis for the dental provider to have a stronger understanding of the different categories of gingival diseases and conditions that are commonly encountered in clinical practice. Learning Objectives • Define periodontal health and be able to describe the clinical features that are consistent with signs of periodontal health. • List the two major subdivisions of gingival disease as established by the American Academy of Periodontology and the European Federation of Periodontology. -

Clinical Sheet
Dental Surgery Clinical Sheet PERIODONTAL REGENERATION ON TWO TEETH AFFECTED BY A SEVERE PERIODONTAL DISEASE Use of an equine origin granular graft in combination with an amelogenin gel. In subjects most at risk, the inflammatory response to bacterial colonization of gingival pockets may give rise to periodontitis, a destructive process that leads to the loss of some of the bone and connective tissue, as well as to apical migration of junctional epithelium. Starting from typical symptoms of gingivitis, characterized by redness, swelling and bleeding tendency, over time one observes a significant change in the biofilm species, where A. actinomycetemcomitans start becoming predominant, as well as red complex bacteria and, to a lesser extent, those of the orange complex. The progress of periodontitis is not constant over time and may vary from person to person, however in its aggressive forms it often eventually leads to the loss of the affected members. Causal therapy eliminates the microbial biofilm and the inflammatory condition caused by it, Francesco Bellucci Private practitioner but the tissue defects will not be able to repair spontaneously. Hence the clinical need to have Avellino, Italy recourse to regeneration procedures that include the alveolar process, to achieve preservation [email protected] of the members originally involved in the pathology for the longest time possible. Within this framework, using a graft that may be remodeled by osteoclasts and that is very easy to handle may be a significant aid in achieving long-term clinical success. The use of amelogenin-based gels may be just as useful due to their action on the periodontal ligament. -

Principles of Periodontology Andrew R
Marquette University e-Publications@Marquette School of Dentistry Faculty Research and Dentistry, School of Publications 2-1-2013 Principles of Periodontology Andrew R. Dentino Marquette University, [email protected] Seokwoo Lee Jason Mailhot Arthur F. Hefti Marquette University, [email protected] Accepted version. Periodontology 2000, Vol. 61, No. 1 (February 2013): 16-53. DOI. © 1999-2018 John Wiley & Sons, Inc. Used with permission. Marquette University e-Publications@Marquette Dentistry Faculty Research and Publications/School of Dentistry This paper is NOT THE PUBLISHED VERSION; but the author’s final, peer-reviewed manuscript. The published version may be accessed by following the link in the citation below. Periodontology 2000, Vol. 61, No. 1 (2013): 16-53. DOI. This article is © Wiley and permission has been granted for this version to appear in e-Publications@Marquette. Wiley does not grant permission for this article to be further copied/distributed or hosted elsewhere without the express permission from Wiley. Table of Contents Abstract ......................................................................................................................................................... 3 History ........................................................................................................................................................... 5 Early Observations .................................................................................................................................... 5 From -
Staging and Grading Periodontitis
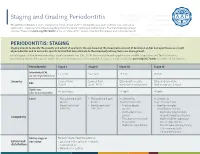
Staging and Grading Periodontitis The 2017 World Workshop on the Classification of Periodontal and Peri-Implant Diseases and Conditions resulted in a new classification of periodontitis characterized by a multidimensional staging and grading system. The charts below provide an overview. Please visit perio.org/2017wwdc for the complete suite of reviews, case definition papers, and consensus reports. PERIODONTITIS: STAGING Staging intends to classify the severity and extent of a patient’s disease based on the measurable amount of destroyed and/or damaged tissue as a result of periodontitis and to assess the specific factors that may attribute to the complexity of long-term case management. Initial stage should be determined using clinical attachment loss (CAL). If CAL is not available, radiographic bone loss (RBL) should be used. Tooth loss due to periodontitis may modify stage definition. One or more complexity factors may shift the stage to a higher level. Seeperio.org/2017wwdc for additional information. Periodontitis Stage I Stage II Stage III Stage IV Interdental CAL 1 – 2 mm 3 – 4 mm ≥5 mm ≥5 mm (at site of greatest loss) Severity Coronal third Coronal third Extending to middle Extending to middle RBL (<15%) (15% - 33%) third of root and beyond third of root and beyond Tooth loss No tooth loss ≤4 teeth ≥5 teeth (due to periodontitis) Local • Max. probing depth • Max. probing depth In addition to In addition to ≤4 mm ≤5 mm Stage II complexity: Stage III complexity: • Mostly horizontal • Mostly horizontal • Probing depths • Need for -

Retrospective Analysis of the Risk Factors of Peri-Implantitis Nathan Anderson1, Adam Lords2, Ronald Laux3, Wendy Woodall4, Neamat Hassan Abubakr5
ORIGINAL RESEARCH Retrospective Analysis of the Risk Factors of Peri-implantitis Nathan Anderson1, Adam Lords2, Ronald Laux3, Wendy Woodall4, Neamat Hassan Abubakr5 ABSTRACT Aim and objective: Peri-implantitis is a key concern for dental implants and the main common reason for implant failure. This investigation evaluated the risk factors and their implications on peri-implantitis. Materials and methods: A retrospective search of the patients’ clinical notes was performed to identify the documented cases of peri-implantitis. The inclusion criteria encompassed patients who were 18 years and older and were seen at the School of Dental Medicine, University of Nevada, Las Vegas, from January 2014 through September 2018. The search revealed that the number of peri-implantitis cases was 28, with an overall 45 implants. Data were collected and analyzed using the Chi-square test. Results: Total 28 patients presented with peri-implantitis. The distribution of males to females with peri-implantitis was 60.7 and 39.3%, respectively. The highest number of patients (21.4%) presenting with peri-implantitis fell within the age range of 65–69 years; 53.3% of peri- implantitis cases were in the maxillary arch. The predilection area for peri-implantitis was the mandibular first molar (24.4%). Periodontitis was the most significant cause (60.7%); respiratory diseases (42.9%) followed by hypertension (28.6%) were the most prevalent medical conditions in the studied population. Peri-implantitis occurred most frequently among Caucasians (62.7%), followed by Hispanics (29%). Conclusion: Within the limitations of the current evaluation, findings support previous claims that periodontitis remains the strongest predictor of peri-implantitis.