Farren 2020.Pdf (3.918Mb)
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

30297-Nidderdale 2012 Schedule 5:Layout 1
P R O G R A M M E (Time-table will be strictly adhered to where possible) ORDER OF JUDGING: Approx. 08.00 a.m. Breeding Hunters (commencing with Ridden Hunter Class) 09.00 a.m. Sheep Dog Trials 09.00 a.m. Carcass Class 09.00 a.m. Dogs Approx. 09.00 a.m. Riding and Turnout Approx. 09.00 a.m. Coloured Horse/Pony In-hand 09.15 a.m. Young Farmers’ Cattle 09.30 a.m. Dry Stone Walling Ballot 09.30 a.m. Beef Cattle (Local) 09.45 a.m. Sheep Approx. 10.00 a.m. All Other Cattle Judging commences Approx. 10.00 a.m. Children’s Riding Classes Approx. 10.00 a.m. Heavy Weight Agricultural Horses 10.00 a.m. Goats 10.00 a.m. Produce, Home Produce and Crafts (Benching 09.45 a.m.) 10.00 a.m. Flowers, Vegetables and Farm Crops (Benching 09.45 a.m.) 10.00 a.m. Poultry, Pigeons and Rabbits 10.30 a.m. ‘Pateley Pantry’ Stands Approx. 10.45 a.m. Mountain & Moorland 11.00 a.m. Pigs Approx. 11.00 a.m. Ridden Coloured 11.00 a.m. Trade Stands 1.15 p.m. Junior Shepherd/Shepherdess Classes (judged at the sheep pens) Approx. 2.00 p.m. Childrens’ Pet Classes (judged in the cattle rings) 2.00 p.m. Sheep - Supreme Championship MAIN RING ATTRACTIONS: 08.00-12.00 Judging - Horse and Pony classes 12.00-12.35 Inch Perfect Trials Display Team 12.35-12.55 Terrier Racing 12.55-1.30 ATV Manoeuvrability Test 1.30-2.00 Young Farmers Mascot Football 2.00-2.20 Parade of Fox Hounds by West of Yore Hunt & Claro Beagles 2.20-3.00 Inch Perfect Trials Display Team 3.00-3.30 GRAND PARADE AND PRESENTATION OF TROPHIES (Excluding Sheep, Goats, Pigs, Produce and WI) Parade of Tractors celebrating 8 decades of Nidderdale Young Farmers Club 3.30- Show Jumping OTHER ATTRACTIONS: Meltham & Meltham Mills Band playing throughout the day 12.00-12.15 St Cuthbert’s Primary School Band 12.15-1.15 Lofthouse & Middlesmoor Silver Band Forestry Exhibition Heritage Marquee Small Traders/Craft Marquee Pateley Pantry Marquee with Cookery Demonstrations 11.00 a.m. -

Farm Animals and Farming: Part 1
A GUIDE TO THE COUNTRYSIDE: FARM ANIMALS & FARMING by Hunter Adair Farm animals and farming: Part 1 When you are out in the countryside in the summer, you will see a great variety of animals running about in the fields, and if you happen to be travelling in the Dales, or in the hills you will mostly find sheep and probably suckler cattle, which are cows with their calves running with them. Some sheep are bred for the high hills and areas where the land is much less fertile than on the lowland farms. The hill bred sheep are hardy and can stand a great deal of rough weather. In the winter when a blizzard or snow storm is forecast the sheep will come down Judging Blue Face Leicester from the hill tops on their own to lower ground and shelter, they seem to know when a storm sheep at The Royal Highland is coming. Show In Edinburgh There are over 50 breeds of sheep in this country and many people from the towns and cities think one sheep is just like another. All the different breeds of sheep have their own characteristics and peculiarities. Some sheep are pure bred and some sheep are cross bred to get a particular lamb, which a farmer may prefer, and which may suit his farm. Some breeds of sheep have been developed in certain parts of the country and in certain areas, and the name of the sheep is taken from the district where they were born and bred. In Scotland for instance they have numerous breeds of sheep which are all different. -
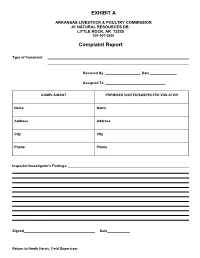
Complaint Report
EXHIBIT A ARKANSAS LIVESTOCK & POULTRY COMMISSION #1 NATURAL RESOURCES DR. LITTLE ROCK, AR 72205 501-907-2400 Complaint Report Type of Complaint Received By Date Assigned To COMPLAINANT PREMISES VISITED/SUSPECTED VIOLATOR Name Name Address Address City City Phone Phone Inspector/Investigator's Findings: Signed Date Return to Heath Harris, Field Supervisor DP-7/DP-46 SPECIAL MATERIALS & MARKETPLACE SAMPLE REPORT ARKANSAS STATE PLANT BOARD Pesticide Division #1 Natural Resources Drive Little Rock, Arkansas 72205 Insp. # Case # Lab # DATE: Sampled: Received: Reported: Sampled At Address GPS Coordinates: N W This block to be used for Marketplace Samples only Manufacturer Address City/State/Zip Brand Name: EPA Reg. #: EPA Est. #: Lot #: Container Type: # on Hand Wt./Size #Sampled Circle appropriate description: [Non-Slurry Liquid] [Slurry Liquid] [Dust] [Granular] [Other] Other Sample Soil Vegetation (describe) Description: (Place check in Water Clothing (describe) appropriate square) Use Dilution Other (describe) Formulation Dilution Rate as mixed Analysis Requested: (Use common pesticide name) Guarantee in Tank (if use dilution) Chain of Custody Date Received by (Received for Lab) Inspector Name Inspector (Print) Signature Check box if Dealer desires copy of completed analysis 9 ARKANSAS LIVESTOCK AND POULTRY COMMISSION #1 Natural Resources Drive Little Rock, Arkansas 72205 (501) 225-1598 REPORT ON FLEA MARKETS OR SALES CHECKED Poultry to be tested for pullorum typhoid are: exotic chickens, upland birds (chickens, pheasants, pea fowl, and backyard chickens). Must be identified with a leg band, wing band, or tattoo. Exemptions are those from a certified free NPIP flock or 90-day certificate test for pullorum typhoid. Water fowl need not test for pullorum typhoid unless they originate from out of state. -

227 Sheep SHEEP DEPARTMENT Kelly Secord
SHEEP DEPARTMENT Kelly Secord- Superintendent Entry Information: Entries can be made online at livestockexpo.org. Entry Deadline and Fee October 10, 2020 Junior Breeding Sheep Entry Fee: $18.00 Junior Market Lamb Entry Fee: $30.00 Open Show Entry Fee: $20.00 Junior Breeding and Market Showmanship Entry Fee: $10.00 *Pre-Entry required* There will be a $25.00 service charge on all declined credit cards. Sheep Arrival Schedule Junior Breeding Sheep - November 11, 8:00 a.m. thru November 13, 12 Noon Junior Market Lambs/Commercial Ewes - November 11, 8:00 a.m. thru November 12, 12 Noon Open Breeding Sheep - November 11, 8:00 a.m. thru November 14, 4:00 p.m. Release Schedule Junior Sheep: Breeds will be released following completion of each BREED show. (Unless entered in Open show, then must follow open show release) Open Sheep: All breeds released upon completion of each breed's show unless showing in Supreme Selection, Thursday, November 19th. Stalling Information Stalling will be done based on number of entries. Stalling preferences must be put on entrty form to be taken into consideration. Pen size in South Wing A & B is 6x6 or 7X7. Feeders Supply - (502) 583-3867 Show Schedule WEDNESDAY, NOVEMBER 11, 2020 8:00 a.m. Begin Receiving Sheep 12:00 Noon to 5:00 p.m. Breeding Sheep and Showmanship Check-In THURSDAY, NOVEMBER 12, 2020 8:00 a.m. Continue Receiving Sheep 9:00 a.m. to 5:00 p.m. Breeding Sheep and Showmanship Check-In 4:00 p.m. Market Lambs must be in place and weight cards turned in FRIDAY, NOVEMBER 13, 2020 8:00 a.m. -

Prion Agent Diversity and Species Barrier
Vet. Res. (2008) 39:47 www.vetres.org DOI: 10.1051/vetres:2008024 c INRA, EDP Sciences, 2008 Review article Prion agent diversity and species barrier Vincent Beringue´ 1*, Jean-Luc Vilotte2, Hubert Laude1 1 Institut National de la Recherche Agronomique (INRA), UR892, Virologie et Immunologie Moléculaires, F-78350 Jouy-en-Josas, France 2 INRA, UR339, Génétique Biochimique et Cytogénétique, F-78350 Jouy-en-Josas, France (Received 25 March 2008; accepted 30 May 2008) Abstract – Mammalian prions are the infectious agents responsible for transmissible spongiform en- cephalopathies (TSE), a group of fatal, neurodegenerative diseases, affecting both domestic animals and humans. The most widely accepted view to date is that these agents lack a nucleic acid genome and con- sist primarily of PrPSc, a misfolded, aggregated form of the host-encoded cellular prion protein (PrPC)that propagates by autocatalytic conversion and accumulates mainly in the brain. The BSE epizooty, allied with the emergence of its human counterpart, variant CJD, has focused much attention on two characteristics that prions share with conventional infectious agents. First, the existence of multiple prion strains that impose, after inoculation in the same host, specific and stable phenotypic traits such as incubation period, molec- ular pattern of PrPSc and neuropathology. Prion strains are thought to be enciphered within distinct PrPSc conformers. Second, a transmission barrier exists that restricts the propagation of prions between different species. Here we discuss the possible situations resulting from the confrontation between species barrier and prion strain diversity, the molecular mechanisms involved and the potential of interspecies transmission of animal prions, including recently discovered forms of TSE in ruminants. -

Selected Readings on the History and Use of Old Livestock Breeds
NATIONAL AGRICULTURAL LIBRARY ARCHIVED FILE Archived files are provided for reference purposes only. This file was current when produced, but is no longer maintained and may now be outdated. Content may not appear in full or in its original format. All links external to the document have been deactivated. For additional information, see http://pubs.nal.usda.gov. Selected Readings on the History and Use of Old Livestock Breeds United States Department of Agriculture Selected Readings on the History and Use of Old Livestock Breeds National Agricultural Library September 1991 Animal Welfare Information Center By: Jean Larson Janice Swanson D'Anna Berry Cynthia Smith Animal Welfare Information Center National Agricultural Library U.S. Department of Agriculture And American Minor Breeds Conservancy P.O. Box 477 Pittboro, NC 27312 Acknowledgement: Jennifer Carter for computer and technical support. Published by: U. S. Department of Agriculture National Agricultural Library Animal Welfare Information Center Beltsville, Maryland 20705 Contact us: http://awic.nal.usda.gov/contact-us Web site: www.nal.usda.gov/awic Published in cooperation with the Virginia-Maryland Regional College of Veterinary Medicine Policies and Links Introduction minorbreeds.htm[1/15/2015 2:16:51 PM] Selected Readings on the History and Use of Old Livestock Breeds For centuries animals have worked with and for people. Cattle, goats, sheep, pigs, poultry and other livestock have been an essential part of agriculture and our history as a nation. With the change of agriculture from a way of life to a successful industry, we are losing our agricultural roots. Although we descend from a nation of farmers, few of us can name more than a handful of livestock breeds that are important to our production of food and fiber. -

SHEEP Blackface Sheep Breeders' Association
SHEEP Blackface Sheep Breeders’ Association ................. 48 Tay Street, Perth, Scotland. Scottish Blackface Breeders’ Association ............... 1699 H H Hwy., Willow Springs, MO 65793 U.S.A. Bluefaced Leicester Sheep Breeders Association .. Riverside View, Warwick Rd., Carlisle, CA1 2BS Scotland Border Leicester Sheep Breeders ........................... Greenend, St. Boswells, Melrose, TD6 9ES England California Red Sheep Registry ................................ P.O. Box 468, LaPlata, NM 87418 U.S.A. British Charollais, Sheep Society ............................ Youngmans Rd., Wymondham, Norfolk NR18 0RR England Mouton Charollais, Texel & Romanov .................... U.P.R.A., 36, rue du Général Leclerc, 71120 Charolles, France American Cheviot Sheep Society, Inc ..................... R.R. 1, Box 100, Clarks Hill, IN 47930 U.S.A. Cheviot Sheep Society ............................................ 1 Bridge St., Hawick, Scotland North American Clun Forest Association ................ W 5855 Muhlum Rd., Holmen, WI 54636 U.S.A. Columbia Sheep Breeders’ Association of P.O. Box 272, Upper Sandusky, OH America 43351 U.S.A. American Corriedale Association, Inc. .................... Box 391, Clay City, IL 62824 U.S.A. Australian Corriedale Sheep Breeders’ Sydney, N.S.W., Australia. Association Corriedale Sheep Society, Inc. ............................... 154 Hereford St., Christchurch, New Zealand. American Cotswold Record Association ................. 18 Elm St., P.O. Box 59, Plympton, MA 02367 U.S.A. Cotswold Breeders Association ............................. -

Map of Farms and Agricultural Resources
COLRAIN Town of F I S K E 3 TER M EN IL ^_ D D AD P A L A ST RO 6 R O R Shelburne WE A R O C O R ^_ A S D E S V M A E A R D G R O A N D O S L 34 I ^_ W 15 BRO OK ROAD N ^_ TO K D N A A O R F R Existing Farms & D A Agricultural P O A R CHARLEMONT T T E E N N 35 R R U O B A ^_ L E D Resources H S N I A D R A Town of Shelburne L O O R P C E N I C A K R V L Existing Farms I L O L C 1 E R Id Owner NAME ADDRESS TYPE ^_ O A 28 D Bassett, Bob and 26 D A ^_ Open Space 1 Basset Farm Main St. Beef Cattle, Chickens, Maple Syrup ^_D O Connie R A O K 32 Bingham, Bardwell Ferry R W S 2 Goats A ^_ D Elliston Rd H L O O M Smead’s N Y E E L 3 Boivin, Corrie Meadow View Smead Hill Rd Dairy Cattle D T R A and Recreation T I O Farm L R T Bragdon, Jim Country Maple Old Greenfield Maple Syrup, Maple Products, and O L 4 and Angel Farm Rd Farm Services E R A Frank Williams U AD R RO 5 Call, C. Donald Registered Shropshire Sheep Q E Rd 7 S OW Plan T T ^_ S 10 Coombs, Russell Coombs Hill Rd, E LD Coombs Hill E NO R Y D ^_ 6 and daughter Colrain Barn in Dairy Cattle E A Farm T D R RO S Karen Herzig Shelburne A 17 C O I 2014 - 2021 R 13 ^_ N Dairy Cattle, Maple Syrup, Maple A E T N E H ^_ S Products, Seasonal Restaurant, E C A U L R E M Davenport, Norm Davenport M T M R M 7 Tower Rd Raw Milk, Eggs, Fire Wood, and A S T P E I and Lisa Maple Farm E T N L P Hay, Shelburne Falls Farmers E I E O D R A R O T S )"2 I Market M V S C E T R R Mercy Anderson E E C E 8 Dole, Bucky Anderson Farm Registered Milking Shorthorn Cattle T ROSS A T S S Rd TREET W O SHELBURNE 20 U Old -

Livestock Classes Prize Schedule
SCHEDULE SPONSOR CLOSING DATE FOR ENTRIES April 17th LIVESTOCK CLASSES PRIZE SCHEDULE ENTER ONLINE: WWW.RCSENTRIES.CO.UK | TELEPHONE: 01208 812183 HOSTING COMPETITIONS FOR ALPACAS - ANGORA GOATS - CATTLE - SHEEP PIGS - DAIRY GOATS - DONKEYS SHEARING - LIVE LAMB - YFC Visit our website to see our full range of classes and to enter online w w w . d e v o n c o u n t y s h o w . c o . u k CONTENTS PAGE Bye-Laws and Regulations ...................................................................................................................................................... 59 Privacy Policy ............................................................................................................................................................................. 5 Entry Fees ................................................................................................................................................................................... 5 Sponsorship ................................................................................................................................................................................ 6 Membership Application Form .................................................................................................................................................. 8 Provisional Judging Time Tables .............................................................................................................................................. 9 Regulations Cattle ....................................................................................................................................................................................... -

University of Southampton Research Repository Eprints Soton
University of Southampton Research Repository ePrints Soton Copyright © and Moral Rights for this thesis are retained by the author and/or other copyright owners. A copy can be downloaded for personal non-commercial research or study, without prior permission or charge. This thesis cannot be reproduced or quoted extensively from without first obtaining permission in writing from the copyright holder/s. The content must not be changed in any way or sold commercially in any format or medium without the formal permission of the copyright holders. When referring to this work, full bibliographic details including the author, title, awarding institution and date of the thesis must be given e.g. AUTHOR (year of submission) "Full thesis title", University of Southampton, name of the University School or Department, PhD Thesis, pagination http://eprints.soton.ac.uk UNIVERSITY OF SOUTHAMPTON FACULTY OF MEDICINE, HEALTH & LIFE SCIENCES School of Biological Sciences Proteins as markers of TSE infection in sheep blood Joanne Martin Thesis for the degree of Doctor of Philosophy September 2008 UNIVERSITY OF SOUTHAMPTON ABSTRACT FACULTY OF MEDICINE, HEALTH AND LIFE SCIENCES SCHOOL OF BIOLOGICAL SCIENCES Doctor of Philosophy PROTEINS AS MARKERS OF TSE INFECTION IN SHEEP BLOOD Joanne Martin Transmissible spongiform encephalopathies (TSEs) are a group of fatal infectious neurodegenerative diseases affecting both humans and agricultural animals. TSE transmission via blood transfusion has been demonstrated experimentally in rodent, primate and sheep models. Additionally, in humans, four variant Creutzfeld-Jakob disease (vCJD) cases have been reported which probably resulted from infected blood transfusions. Although TSEs can be transmitted via blood transfusion, little is known about which blood cells are involved in the replication of the TSE agent and how infectivity is spread throughout the body prior to neuroinvasion. -

Wyefield Apiaries Label
ADRAN Y DEFAID • SHEEP SECTION The Society acknowledges with grateful thanks the assistance/sponsorship of the section by Greenlands Insurance Services Ltd, Farmplus Constructions Ltd, Ewe Moo Foot Rest, J. Straker, Chadwick and Sons, The Tack Room, Chilvers Country Supplies, Scotmin Nutrition NODIADAU CYFFREDINOL • CYMHWYSTER Sheep GENERAL NOTES • ELIGIBILITY Defaid 1. ALL SHEEP MUST BE NON MV ACCREDITED. 2. Exhibitors limited to two entries per class unless otherwise specified. 3. Any sheep displayed as part of a tradestand will NOT be eligible to enter in any of the competitive classes scheduled below. 4. The decisions relating to the allocation of particular breeds to the relevant sections scheduled shall be at the discretion of the Chief Steward whose decision will be final. The Society reserves the right to re-allocate entries where appropriate. 5. If extreme numbers of high entries are received for the event the Society reserves the right to take the necessary action deemed appropriate. 6. Please make sure that all sheep are entered in the correct class. Incorrect entries cannot be transferred. No animal can be entered in more than one section. 7. All sheep should be ‘shown to best advantage’ or as determined by their Breed Societies. 8. Appropriate pens will be allocated by the Chief Steward prior to the event. Each pen is approximately 1.5m x 1.5m. If space is available, the Society will also provide random tack pens. 9. Exhibitors: please note that during the judging of the section’s champion, second placed exhibits must be on standby, otherwise they will not be considered for judging. -
Breeding Sheep Without Compromise Bluefaced
www.blueleicester.co.uk To the 2015 edition of the Welcome Spring Looking Ahead Magazine Chairman’s Message Diversity is our Editorial breed’s strength. Office News .....................................................4 Stay Strong Stu ...............................................5 President’s Message .......................................6 Welcome to “The Year of The Sheep” (Chinese New Publicity Report ...............................................7 Year)! Flock Feature - Piel View ..............................8-9 Hopefully this is a good omen, as last year China Flock Feature - Firth ..................................10-11 imported 13,000 tonnes of British lamb, and hopefully Flock Feature - Tanhouse Farm ................12-13 this year will see an increase, sadly partly due to the NSA North Sheep 2015 ............................14-15 draught in Australia and New Zealand as lamb numbers NSA Welsh Sheep 2015 ...........................16-17 are down. Carl Stephenson 2015 Female Sale Reports .......................18-21 British Wool Marketing Board Update ............23 The female sales got the year off to a good start at Hawes and Carlisle, with many ewes Regional News ........................................24, 26 and hoggs going to start new flocks. The Bluefaced Leicester is the sire of the unprecedented commercial ewe “The Mule”, Advertising which is the greatest producer of prime lambs from grass. Mules are bred from a variety A B Europe ...................................................IFC of hill ewes, which go on to breed