Molecular Typing for Red Cell Antigens
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Human and Mouse CD Marker Handbook Human and Mouse CD Marker Key Markers - Human Key Markers - Mouse
Welcome to More Choice CD Marker Handbook For more information, please visit: Human bdbiosciences.com/eu/go/humancdmarkers Mouse bdbiosciences.com/eu/go/mousecdmarkers Human and Mouse CD Marker Handbook Human and Mouse CD Marker Key Markers - Human Key Markers - Mouse CD3 CD3 CD (cluster of differentiation) molecules are cell surface markers T Cell CD4 CD4 useful for the identification and characterization of leukocytes. The CD CD8 CD8 nomenclature was developed and is maintained through the HLDA (Human Leukocyte Differentiation Antigens) workshop started in 1982. CD45R/B220 CD19 CD19 The goal is to provide standardization of monoclonal antibodies to B Cell CD20 CD22 (B cell activation marker) human antigens across laboratories. To characterize or “workshop” the antibodies, multiple laboratories carry out blind analyses of antibodies. These results independently validate antibody specificity. CD11c CD11c Dendritic Cell CD123 CD123 While the CD nomenclature has been developed for use with human antigens, it is applied to corresponding mouse antigens as well as antigens from other species. However, the mouse and other species NK Cell CD56 CD335 (NKp46) antibodies are not tested by HLDA. Human CD markers were reviewed by the HLDA. New CD markers Stem Cell/ CD34 CD34 were established at the HLDA9 meeting held in Barcelona in 2010. For Precursor hematopoetic stem cell only hematopoetic stem cell only additional information and CD markers please visit www.hcdm.org. Macrophage/ CD14 CD11b/ Mac-1 Monocyte CD33 Ly-71 (F4/80) CD66b Granulocyte CD66b Gr-1/Ly6G Ly6C CD41 CD41 CD61 (Integrin b3) CD61 Platelet CD9 CD62 CD62P (activated platelets) CD235a CD235a Erythrocyte Ter-119 CD146 MECA-32 CD106 CD146 Endothelial Cell CD31 CD62E (activated endothelial cells) Epithelial Cell CD236 CD326 (EPCAM1) For Research Use Only. -

Viewed Under 23 (B) Or 203 (C) fi M M Male Cko Mice, and Largely Unaffected Magni Cation; Scale Bars, 500 M (B) and 50 M (C)
BRIEF COMMUNICATION www.jasn.org Renal Fanconi Syndrome and Hypophosphatemic Rickets in the Absence of Xenotropic and Polytropic Retroviral Receptor in the Nephron Camille Ansermet,* Matthias B. Moor,* Gabriel Centeno,* Muriel Auberson,* † † ‡ Dorothy Zhang Hu, Roland Baron, Svetlana Nikolaeva,* Barbara Haenzi,* | Natalya Katanaeva,* Ivan Gautschi,* Vladimir Katanaev,*§ Samuel Rotman, Robert Koesters,¶ †† Laurent Schild,* Sylvain Pradervand,** Olivier Bonny,* and Dmitri Firsov* BRIEF COMMUNICATION *Department of Pharmacology and Toxicology and **Genomic Technologies Facility, University of Lausanne, Lausanne, Switzerland; †Department of Oral Medicine, Infection, and Immunity, Harvard School of Dental Medicine, Boston, Massachusetts; ‡Institute of Evolutionary Physiology and Biochemistry, St. Petersburg, Russia; §School of Biomedicine, Far Eastern Federal University, Vladivostok, Russia; |Services of Pathology and ††Nephrology, Department of Medicine, University Hospital of Lausanne, Lausanne, Switzerland; and ¶Université Pierre et Marie Curie, Paris, France ABSTRACT Tight control of extracellular and intracellular inorganic phosphate (Pi) levels is crit- leaves.4 Most recently, Legati et al. have ical to most biochemical and physiologic processes. Urinary Pi is freely filtered at the shown an association between genetic kidney glomerulus and is reabsorbed in the renal tubule by the action of the apical polymorphisms in Xpr1 and primary fa- sodium-dependent phosphate transporters, NaPi-IIa/NaPi-IIc/Pit2. However, the milial brain calcification disorder.5 How- molecular identity of the protein(s) participating in the basolateral Pi efflux remains ever, the role of XPR1 in the maintenance unknown. Evidence has suggested that xenotropic and polytropic retroviral recep- of Pi homeostasis remains unknown. Here, tor 1 (XPR1) might be involved in this process. Here, we show that conditional in- we addressed this issue in mice deficient for activation of Xpr1 in the renal tubule in mice resulted in impaired renal Pi Xpr1 in the nephron. -

4-6 Weeks Old Female C57BL/6 Mice Obtained from Jackson Labs Were Used for Cell Isolation
Methods Mice: 4-6 weeks old female C57BL/6 mice obtained from Jackson labs were used for cell isolation. Female Foxp3-IRES-GFP reporter mice (1), backcrossed to B6/C57 background for 10 generations, were used for the isolation of naïve CD4 and naïve CD8 cells for the RNAseq experiments. The mice were housed in pathogen-free animal facility in the La Jolla Institute for Allergy and Immunology and were used according to protocols approved by the Institutional Animal Care and use Committee. Preparation of cells: Subsets of thymocytes were isolated by cell sorting as previously described (2), after cell surface staining using CD4 (GK1.5), CD8 (53-6.7), CD3ε (145- 2C11), CD24 (M1/69) (all from Biolegend). DP cells: CD4+CD8 int/hi; CD4 SP cells: CD4CD3 hi, CD24 int/lo; CD8 SP cells: CD8 int/hi CD4 CD3 hi, CD24 int/lo (Fig S2). Peripheral subsets were isolated after pooling spleen and lymph nodes. T cells were enriched by negative isolation using Dynabeads (Dynabeads untouched mouse T cells, 11413D, Invitrogen). After surface staining for CD4 (GK1.5), CD8 (53-6.7), CD62L (MEL-14), CD25 (PC61) and CD44 (IM7), naïve CD4+CD62L hiCD25-CD44lo and naïve CD8+CD62L hiCD25-CD44lo were obtained by sorting (BD FACS Aria). Additionally, for the RNAseq experiments, CD4 and CD8 naïve cells were isolated by sorting T cells from the Foxp3- IRES-GFP mice: CD4+CD62LhiCD25–CD44lo GFP(FOXP3)– and CD8+CD62LhiCD25– CD44lo GFP(FOXP3)– (antibodies were from Biolegend). In some cases, naïve CD4 cells were cultured in vitro under Th1 or Th2 polarizing conditions (3, 4). -

Fcγr Binding and ADCC Activity of Human Igg Allotypes
fimmu-11-00740 May 4, 2020 Time: 17:25 # 1 ORIGINAL RESEARCH published: 06 May 2020 doi: 10.3389/fimmu.2020.00740 FcgR Binding and ADCC Activity of Human IgG Allotypes Steven W. de Taeye1,2*†, Arthur E. H. Bentlage2, Mirjam M. Mebius3, Joyce I. Meesters3, Suzanne Lissenberg-Thunnissen2, David Falck4, Thomas Sénard4, Nima Salehi1, Manfred Wuhrer4, Janine Schuurman3, Aran F. Labrijn3, Theo Rispens1‡ and Gestur Vidarsson2‡ 1 Sanquin Research and Landsteiner Laboratory, Department of Immunopathology, Amsterdam UMC, University of Amsterdam, Amsterdam, Netherlands, 2 Sanquin Research and Landsteiner Laboratory, Department of Experimental Edited by: Immunohematology, Amsterdam UMC, University of Amsterdam, Amsterdam, Netherlands, 3 Genmab, Utrecht, Eric O. Long, Netherlands, 4 Center for Proteomics and Metabolomics, Leiden University Medical Center, Leiden, Netherlands National Institute of Allergy and Infectious Diseases (NIAID), United States Antibody dependent cellular cytotoxicity (ADCC) is an Fc-dependent effector function Reviewed by: of IgG important for anti-viral immunity and anti-tumor therapies. NK-cell mediated Amy W. Chung, ADCC is mainly triggered by IgG-subclasses IgG1 and IgG3 through the IgG-Fc- The University of Melbourne, Australia receptor (FcgR) IIIa. Polymorphisms in the immunoglobulin gamma heavy chain gene Geoffrey Thomas Hart, University of Minnesota Twin Cities, likely form a layer of variation in the strength of the ADCC-response, but this has United States never been studied in detail. We produced all 27 known IgG allotypes and assessed *Correspondence: FcgRIIIa binding and ADCC activity. While all IgG1, IgG2, and IgG4 allotypes behaved Steven W. de Taeye [email protected]; similarly within subclass, large allotype-specific variation was found for IgG3. -
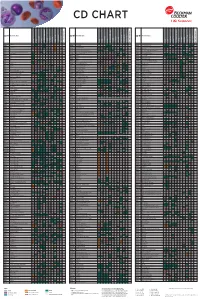
Flow Reagents Single Color Antibodies CD Chart
CD CHART CD N° Alternative Name CD N° Alternative Name CD N° Alternative Name Beckman Coulter Clone Beckman Coulter Clone Beckman Coulter Clone T Cells B Cells Granulocytes NK Cells Macrophages/Monocytes Platelets Erythrocytes Stem Cells Dendritic Cells Endothelial Cells Epithelial Cells T Cells B Cells Granulocytes NK Cells Macrophages/Monocytes Platelets Erythrocytes Stem Cells Dendritic Cells Endothelial Cells Epithelial Cells T Cells B Cells Granulocytes NK Cells Macrophages/Monocytes Platelets Erythrocytes Stem Cells Dendritic Cells Endothelial Cells Epithelial Cells CD1a T6, R4, HTA1 Act p n n p n n S l CD99 MIC2 gene product, E2 p p p CD223 LAG-3 (Lymphocyte activation gene 3) Act n Act p n CD1b R1 Act p n n p n n S CD99R restricted CD99 p p CD224 GGT (γ-glutamyl transferase) p p p p p p CD1c R7, M241 Act S n n p n n S l CD100 SEMA4D (semaphorin 4D) p Low p p p n n CD225 Leu13, interferon induced transmembrane protein 1 (IFITM1). p p p p p CD1d R3 Act S n n Low n n S Intest CD101 V7, P126 Act n p n p n n p CD226 DNAM-1, PTA-1 Act n Act Act Act n p n CD1e R2 n n n n S CD102 ICAM-2 (intercellular adhesion molecule-2) p p n p Folli p CD227 MUC1, mucin 1, episialin, PUM, PEM, EMA, DF3, H23 Act p CD2 T11; Tp50; sheep red blood cell (SRBC) receptor; LFA-2 p S n p n n l CD103 HML-1 (human mucosal lymphocytes antigen 1), integrin aE chain S n n n n n n n l CD228 Melanotransferrin (MT), p97 p p CD3 T3, CD3 complex p n n n n n n n n n l CD104 integrin b4 chain; TSP-1180 n n n n n n n p p CD229 Ly9, T-lymphocyte surface antigen p p n p n -

Blood Bank I D
The Osler Institute Blood Bank I D. Joe Chaffin, MD Bonfils Blood Center, Denver, CO The Fun Just Never Ends… A. Blood Bank I • Blood Groups B. Blood Bank II • Blood Donation and Autologous Blood • Pretransfusion Testing C. Blood Bank III • Component Therapy D. Blood Bank IV • Transfusion Complications * Noninfectious (Transfusion Reactions) * Infectious (Transfusion-transmitted Diseases) E. Blood Bank V (not discussed today but available at www.bbguy.org) • Hematopoietic Progenitor Cell Transplantation F. Blood Bank Practical • Management of specific clinical situations • Calculations, Antibody ID and no-pressure sample questions Blood Bank I Blood Groups I. Basic Antigen-Antibody Testing A. Basic Red Cell-Antibody Interactions 1. Agglutination a. Clumping of red cells due to antibody coating b. Main reaction we look for in Blood Banking c. Two stages: 1) Coating of cells (“sensitization”) a) Affected by antibody specificity, electrostatic RBC charge, temperature, amounts of antigen and antibody b) Low Ionic Strength Saline (LISS) decreases repulsive charges between RBCs; tends to enhance cold antibodies and autoantibodies c) Polyethylene glycol (PEG) excludes H2O, tends to enhance warm antibodies and autoantibodies. 2) Formation of bridges a) Lattice structure formed by antibodies and RBCs b) IgG isn’t good at this; one antibody arm must attach to one cell and other arm to the other cell. c) IgM is better because of its pentameric structure. P}Chaffin (12/28/11) Blood Bank I page 1 Pathology Review Course 2. Hemolysis a. Direct lysis of a red cell due to antibody coating b. Uncommon, but equal to agglutination. 1) Requires complement fixation 2) IgM antibodies do this better than IgG. -
Introduction to the Rh Blood Group.Pdf
Introduction to the Rhesus Blood Group Justin R. Rhees, M.S., MLS(ASCP)CM, SBBCM University of Utah Department of Pathology Medical Laboratory Science Program Objectives 1. Describe the major Rhesus (Rh) blood group antigens in terms of biochemical structure and inheritance. 2. Describe the characteristics of Rh antibodies. 3. Translate the five major Rh antigens, genotypes, and haplotypes from Fisher-Race to Wiener nomenclature. 4. State the purpose of Fisher-Race, Wiener, Rosenfield, and ISBT nomenclatures. Background . How did this blood group get its name? . 1937 Mrs. Seno; Bellevue hospital . Unknown antibody, unrelated to ABO . Philip Levine tested her serum against 54 ABO-compatible blood samples: only 13 were compatible. Rhesus (Rh) blood group 1930s several cases of Hemolytic of the Fetus and Newborn (HDFN) published. Hemolytic transfusion reactions (HTR) were observed in ABO- compatible transfusions. In search of more blood groups, Landsteiner and Wiener immunized rabbits with the Rhesus macaque blood of the Rhesus monkeys. Rhesus (Rh) blood group 1940 Landsteiner and Wiener reported an antibody that reacted with about 85% of human red cell samples. It was supposed that anti-Rh was the specificity causing the “intragroup” incompatibilities observed. 1941 Levine found in over 90% of erythroblastosis fetalis cases, the mother was Rh-negative and the father was Rh-positive. Rhesus macaque Rhesus (Rh) blood group Human anti-Rh and animal anti- Rh are not the same. However, “Rh” was embedded into blood group antigen terminology. The -

Supp Table 6.Pdf
Supplementary Table 6. Processes associated to the 2037 SCL candidate target genes ID Symbol Entrez Gene Name Process NM_178114 AMIGO2 adhesion molecule with Ig-like domain 2 adhesion NM_033474 ARVCF armadillo repeat gene deletes in velocardiofacial syndrome adhesion NM_027060 BTBD9 BTB (POZ) domain containing 9 adhesion NM_001039149 CD226 CD226 molecule adhesion NM_010581 CD47 CD47 molecule adhesion NM_023370 CDH23 cadherin-like 23 adhesion NM_207298 CERCAM cerebral endothelial cell adhesion molecule adhesion NM_021719 CLDN15 claudin 15 adhesion NM_009902 CLDN3 claudin 3 adhesion NM_008779 CNTN3 contactin 3 (plasmacytoma associated) adhesion NM_015734 COL5A1 collagen, type V, alpha 1 adhesion NM_007803 CTTN cortactin adhesion NM_009142 CX3CL1 chemokine (C-X3-C motif) ligand 1 adhesion NM_031174 DSCAM Down syndrome cell adhesion molecule adhesion NM_145158 EMILIN2 elastin microfibril interfacer 2 adhesion NM_001081286 FAT1 FAT tumor suppressor homolog 1 (Drosophila) adhesion NM_001080814 FAT3 FAT tumor suppressor homolog 3 (Drosophila) adhesion NM_153795 FERMT3 fermitin family homolog 3 (Drosophila) adhesion NM_010494 ICAM2 intercellular adhesion molecule 2 adhesion NM_023892 ICAM4 (includes EG:3386) intercellular adhesion molecule 4 (Landsteiner-Wiener blood group)adhesion NM_001001979 MEGF10 multiple EGF-like-domains 10 adhesion NM_172522 MEGF11 multiple EGF-like-domains 11 adhesion NM_010739 MUC13 mucin 13, cell surface associated adhesion NM_013610 NINJ1 ninjurin 1 adhesion NM_016718 NINJ2 ninjurin 2 adhesion NM_172932 NLGN3 neuroligin -

Targeted Exome Sequencing Defines Novel and Rare Variants in Complex Blood Group Serology Cases for a Red Blood Cell Reference Laboratory Setting
IMMUNOHEMATOLOGY Targeted exome sequencing defines novel and rare variants in complex blood group serology cases for a red blood cell reference laboratory setting Elizna M. Schoeman ,1 Eileen V. Roulis ,1 Yew-Wah Liew,2 Jacqueline R. Martin,2 Tanya Powley,2 Brett Wilson,2 Glenda M. Millard ,1 Eunike C. McGowan ,1 Genghis H. Lopez ,1 Helen O’Brien ,1 Jennifer A. Condon,3 Robert L. Flower ,1 and Catherine A. Hyland 1 he key role of a modern red blood cell (RBC) ref- BACKGROUND: We previously demonstrated that erence laboratory in transfusion medicine is to targeted exome sequencing accurately defined blood employ serology to solve complex problems. group genotypes for reference panel samples Often, the lack of appropriate RBCs, sera, or characterized by serology and single-nucleotide T polymorphism (SNP) genotyping. Here we investigate reagents makes confident resolution of a complex case the application of this approach to resolve problematic difficult. Resources can be costly and scarce, if available at serology and SNP-typing cases. all, and often require collaboration and generosity of col- 1 STUDY DESIGN AND METHODS: The TruSight One leagues from other international laboratories. In addition, sequencing panel and MiSeq platform was used for reference laboratories commonly employ single- sequencing. CLC Genomics Workbench software was nucleotide polymorphism (SNP) typing microarrays for used for data analysis of the blood group genes RBC genotyping investigations; however, these arrays are implicated in the serology and SNP-typing problem. not comprehensive in their coverage of blood groups or 2-5 Sequence variants were compared to public databases variants. When the combination of traditional serologic listing blood group alleles. -

Inclusion of Additional Reference Reagents in the Existing Collection of WHO International Reference Reagents for Blood Group Genotyping
WHO/BS/2019.2371 ENGLISH ONLY EXPERT COMMITTEE ON BIOLOGICAL STANDARDIZATION Geneva, 21 to 25 October 2019 Inclusion of Additional Reference Reagents in the Existing Collection of WHO International Reference Reagents for Blood Group Genotyping Report of the international collaborative study to evaluate eighteen additional candidates for addition to the existing collection of four WHO International Reference Reagents for blood group genotyping Evgeniya Volkova1, Emilia Sippert1, Meihong Liu1, Teresita Mercado1, Gregory A Denomme2, Orieji Illoh1, Zhugong Liu1, Maria Rios1*, and the Collaborative Study Group3 1 Office of Blood Research and Review, CBER/FDA, Silver Spring, MD, USA. 2 Blood Research Institute and Diagnostic Laboratories, Versiti/BloodCenter of Wisconsin, Milwaukee, WI, USA. * Principal contact: [email protected] 3 Members of the Collaborative Study Group are listed in Appendix 1. NOTE: This document has been prepared for the purpose of inviting comments and suggestions on the proposals contained therein, which will then be considered by the Expert Committee on Biological Standardization (ECBS). Comments MUST be received by 27 September 2019 and should be addressed to the World Health Organization, 1211 Geneva 27, Switzerland, attention: Technologies, Standards and Norms (TSN). Comments may also be submitted electronically to the Responsible Officer: Dr Ivana Knezevic at email: [email protected]. © World Health Organization 2019 All rights reserved. This draft is intended for a restricted audience only, i.e. the individuals and organizations having received this draft. The draft may not be reviewed, abstracted, quoted, reproduced, transmitted, distributed, translated or adapted, in part or in whole, in any form or by any means outside these individuals and organizations (including the organizations' concerned staff and member organizations) without the permission of the World Health Organization. -

Red Blood Cell Antigen Genotyping
Red Blood Cell Antigen Genotyping Testing is useful in determining allelic variants predicting red blood cell (RBC) antigen phenotypes for patients with recent history of transfusion or with conflicting serological antibody results due to partial, variant, or weak expression antigens. Also Tests to Consider useful as an aid in management of hemolytic disease of the fetus and newborn (HDFN). Typical Testing Strategy Disease Overview Phenotype Testing Evaluates specific RBC antigen presence by serology Prevalence and/or Incidence Results can aid in selecting antigen negative RBC units Erythrocyte alloimmunization occurs in up to 58% of sickle cell patients, up to 35% in other transfusion-dependent patients, and in approximately 0.8% of all pregnant Antigen Testing, RBC Phenotype women. Extended 0013020 Method: Hemagglutination Serological testing includes K, Fya, Fyb, Jka, Symptoms Jkb, S, s (k, cellano, testing performed if indicated) to assess maternal or paternal RBC Transfusion reactions or HDFN can occur due to alloimmunization: phenotype status. Antigen Testing, Rh Phenotype 0013019 Intravascular hemolysis: hemoglobinuria, jaundice, shock Extravascular hemolysis: fever and chills Method: Hemagglutination HDFN: fetal hemolytic anemia, hepatosplenomegaly, jaundice, erythroblastosis, Antigen testing for D, C, E, c, and e to assess neurological damage, hydrops fetalis maternal, paternal, or newborn Rh phenotype status Clinical presentation is variable and dependent upon the specific antibody and recipient factors Genotype Testing May help -

Mirepoix LLC on Behalf of Caris Life Sciences, June 22, 2020 No Revisions to These Recommendations
0211U Oncology (pan-tumor), DNA and RNA by next generation sequencing, utilizing formalin-fixed paraffin-embedded tissue, interpretative report for single nucleotide variants, copy number alterations, tumor mutational burden, and microsatellite instability, with therapy association Submitted by Joel de Jesus, Mirepoix LLC on behalf of Caris Life Sciences, June 22, 2020 No revisions to these recommendations 0211U: MI Cancer Seek™ - NGS analysis C. Public Comment Rationale • Recommendation to crosswalk 0211U MI Cancer Seek is a combined whole transcriptome AND whole exome to 0019U (NLA=$3675.00) + 0036U sequencing test that is equivalent to (NLA=$4780.00) performing both: • 0019U: Oncology, RNA, gene expression • 1x multiplier for each by whole transcriptome sequencing, formalin-fixed paraffin-embedded tissue • Recommendation of an NLA equal to or fresh frozen tissue, predictive $8455 for 0211U algorithm reported as potential targets for therapeutic agents • 0036U: Exome (ie, somatic mutations), paired formalin-fixed paraffin-embedded tumor tissue and normal specimen, sequence analyses Submitted by Joel de Jesus, Mirepoix LLC on behalf of Caris Life Sciences, June 22, 2020 No revisions to these recommendations 0211U: MI Cancer Seek™ - NGS analysis C. 0019U* 0211U 0036U** Assay type Whole Whole Whole Whole Transcriptome Transcriptome Exome Exome Sequencing Sequencing Sequencing Sequencing Platform NGS NGS (Illumina) NGS (Illumina) RNASeq RNASeq & DNASeq DNASeq Samples tested FFPE & frozen tumor tissue FFPE tumor tissue FFPE tumor tissue