Fact-Finding Report on Maternal Health in the Ghaziabad Government Health Sector
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
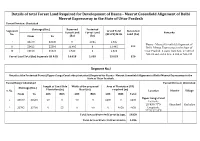
Details of Total Forest Land Required for Development of Dasna
Details of total Forest Land Required for Development of Dasna - Meerut Greenfield Alignment of Delhi Meerut Expressway in the State of Uttar Pradesh Forest Division: Ghaziabad Chainage (Km.) Reserved Protected Segments Grand Total Non-forest Forest Land Forest Land Remarks No. (RF+PF) in Ha Land (ha) From To (ha) (ha) I 33570 33630 0 1.035 1.035 Dasna - Meerut Greenfield Alignment of 320 II 53422 55396 11.495 0 11.495 Delhi Meerut Expressway in the State of III 23100 36520 2.523 0 2.523 Uttar Pradesh. It starts from Km. 27.500 of NH-24 and end at Km. 8.800 of NH-235 Forest Land Total (ha) Segments I,II & III 14.018 1.035 15.053 320 Segment No.I Details of the Protected Forest (Upper Ganga Canal side plantation) Required for Dasna - Meerut Greenfield Alignment of Delhi Meerut Expressway in the State of Uttar Pradesh. Forest Range: Ghaziabad Forest Division: Ghaziabad Length of Canal Side Width of the proposed Area of Plantation (PF) Chainage (Km.) S. No. Plantation (m) Road (m) required (m) Location District Village From To LHS RHS LHS RHS LHS RHS Total Upper Ganga Canal 1 33570 33630 60 0 90 0 5400 0 5400 Latitude: 28°43'0.77"N Ghaziabad Kushaliya 2 33705 33760 0 55 0 90 0 4950 4950 Longitude: 77°32'27.28"E Total Area of Protected Forest in Sqm. 10350 Total Area of Protected Forest in ha 1.035 Segment No.II Details of the Reserved Forest Land Required for Development of Dasna - Meerut Greenfield Alignment of Delhi Meerut Expressway in the State of Uttar Pradesh. -

Before the Uttar Pradesh Electricity Regulatory Commission
BEFORE THE UTTAR PRADESH ELECTRICITY REGULATORY COMMISSION Quorum Shri Desh Deepak Verma, Chairman Shri I. B. Pandey, Member Petitioner Western U.P. Power Transmission Co. Ltd., S-3, 2 nd Floor, Aditya Mega Mall, Indirapuram, Ghaziabad-201010 Versus Respondents 1. Managing Director, Paschimanchal Vidyut Vitran Nigam Ltd., Urja Bhawan, Victoria Park, Meerut-250001 2. Managing Director, Dakshinanchal Vidyut Vitran Nigam Ltd., Urja Bhawan 220, K.V. Up-Sansthan Bypass Road Agra – 282007 3. Managing Director, Poorvanchal Vidyut Vitran Nigam Ltd., Purvanchal Vidyut Bhawan, P.O. Vidyut Nagar, DLW, Varanasi. 4. Managing Director, Madhyanchal Vidyut Vitran Nigam Ltd., 4 Gokhale Marg, Lucknow 5. Managing Director, Uttar Pradesh Power Transmission Company Ltd., 14, Ashok Marg, Shakti Bhawan, Lucknow (UP) Present in the Hearing: 1. Shri Chandra Mohan Mathur, Chief Engineer, UPPTCL 2. Shri S. K. Bhattacharya, Superintending Engineer, UPPTCL 3. Shri J. P. Vimal, Executive Engineer, UPPTCL 4. Shri C. K. Mishra, Executive Engineer, UPPTCL 5. Shri Swapnil Dagur, CGM, WUPPTCL Page 1 of 18 ORDER (Hearing on 3.11.2015) M/s Western U.P. Power Transmission Co. Ltd., S-3, 2 nd Floor, Aditya Mega Mall, Indirapuram, Ghaziabad-201010 filed petition No. 1041/2015 in the matter under sub- section(3) of section 17 of the Indian Electricity Act,2003 and sub-section (iii) of section 4.3.1 of Uttar Pradesh Electricity Regulatory Commission (General Condition of Transmission Licensee) Regulation No. UPERC/Secy.-05-931 dated December 14, 2005 with respect to the intra-state transmission system being established by the Western U.P. Power Transmission Company Ltd for approval of Supplementary Agreement. -

Regional Office - U.P
Regional Office - U.P. Pollution Control Board, Ghaziabad S.No. Name And Address Of The Products Hazardous HW Generating Streams HW Generation In Total Quantity Of HW In MTA (10) Remark Unit Manufactured In Waste (HW) As Per MTA As Per Quantity Of MTA Generating HW Process As Sch. 1 Sch. 2 Sch. 1 Sch. 2 Generation Landfillable Recyclable Incinerable Per Schedule In MTA 1 1 2 3 4 5 6 7 8 9=7+810 11 Closed Unit 1 BHAGWATI PHOSPH&ELEC 12 12.5 0.9 0.9 0.9000 0.0000 0.0000 SELF ENTERPRISES, PL(Ni&Cr) CLOSED S-28, SITE-4, SBD JOB WORK BASIS 2 F.M. PARTS & BREAK DISC 15 15.3 0 0 0.0000 0.0000 0.0000 SELF COMPONENT (P0 LTD, 31 CLOSED A LONI RD I.A. MOHAN NGR. 3 REINZ TALBROS LTD. , GASKET 15 15.3 0 0 0.0000 0.0000 0.0000 CLOSED 19,LONI Rd.MOHAN NGR JOINTING 4 GOOD LUCK INDUSTRY, H.F. ACID 17 17.1 120 120 120.0000 0.0000 0.0000 SELF CLOED 122, A.I.A., MOHAN NGR. 10 MT/D OWN REASONS 5 PANKAJ CHEMICALS, 80, H.F. ACID 17 17.1 0 0 0.0000 0.0000 0.0000 CLOSED R.I.A., MOHAN NGR., 6 ARISTRO PRINTERS P PRINTING OF 21 21.1 0.6 0.6 0.0000 0.0000 0.6000 SELF LTD., E-64, S.S. OF G.T. PAPERS CLOSED ROAD. 7 ASIA CHEMICAL, G.T. PAINTS & 21 21.1 6 6 0.0000 6.0000 0.0000 SELF ROAD, VARNISH CLSOED 8 ADDI INDUSTRIES, C-227, FABRIC 24 24.2 6 6 6.0000 0.0000 0.0000 SELF B.S. -

Planning Proposals for Water Supply of U.P. Sub Region of Ncr
PLANNING PROPOSALS FOR WATER SUPPLY OF U.P. SUB REGION OF NCR A DISSERTATION Submitted in partial fulfilment of the requirements for the award of the degree of MASTER OF URBAN AND RURAL PLANNING By MATINDER KUMAR DEPARTMENT OF ARCHITECTURE & PLANNING INDIAN INSTITUTE OF TECHNOLOGY ROORKEE ROORKEE - 247 667 (INDIA) JUNE, 2007 CANDIDATE'S DECLARATION I hereby certify that the work, which is being presented in the dissertation, entitled "PLANNING PROPOSALS FOR WATER SUPPLY OF U.P. SUB REGION OF NCR", in partial fulfillment of the requirement for the award of the Degree of MASTER OF URBAN AND RURAL PLANNING submitted in the Department of Architecture and Planning, Indian Institute of Technology - Roorkee, is an authentic record of my own work carried out during the period from May 2006 to June 2007 under the supervision of Prof. R. K. Jain, Associate Professor, Department of Architecture and Planning, Indian Institute of Technology - Roorkee. The matter embodied in this dissertation has not been submitted by me for the award of any other Degree. Place: Roorkee ktrAihnkt Dated: June 2c12007 (Matinder Kumar) This is to certify that the above statement made by the candidate Mr. Matinder Kumar is correct to the best of my knowledge. Place: Roorkee Dated: June, 2007 (Prof. R. K. Jain) Associate Professor Department of Architecture and Planning Indian Institute of Technology - Roorkee Roorkee — 247667, India ACKNOWLEDGEMENT I take this opportunity to express my deep sense of gratitude to my respected guide Prof. R. K. Jain, Department of Architecture and Planning, Indian Institute of Technology Roorkee (Uttrakhand) for his constant encouragement, support and expert guidance throughout this work starting from choosing the topic. -

Future of Settlement On
MAP ---- WATER TREATMENT PLANTS- DELHI ---- FUTURE SOURCES OF RAW WATER FOR DELHI CONTENTS ---- SEWAGE TREATMENT PLANTS- DELHI ---- DRAINAGE SYSTEM IN DELHI Modified Planning & Implementation of NCR: ---- LANDFILL SITES - DELHI ---- NATIONAL CAPITAL REGION PROPOSED SETTLEMENT ---- STRATEGY FOR THE DEVELOPMENT OF POWER PATTERN 2021 SECTOR 1. INITIAL PLANNING OF NOIDA. ---- LIST OF PROPOSED POLICY BOXES 2. POWERS OF SOME OF THE SECTIONS OF NCR ACT ---- NATIONAL CAPITAL REGION REGIONAL -2001 : ONLY IN BRIEF CONSTITUENT AREAS 3. WHAT TO DO? ---- NATIONAL CAPITAL REGION REGIONAL -2021 : 4. COMPREHENSIVE PLANNING WILL INCLUDE THE CONSTITUENT AREAS FOLLOWING ACTIVITIES: (104 ITEMS) + SOME ITEMS ---- NATIONAL CAPITAL REGION PHYSIOGRAPHY AND MORE SLOPE 5. SOME IMPORTANT POLICY DECISIONS. ---- NATIONAL CAPITAL REGION LITHOLOGY ---- PHYSICAL GROWTH OF DELHI 1803-1959 & SEVEN- SEVENTEEN DELHIS ---- NATIONAL CAPITAL REGION GEOMORPHIC 6. NAMES OF NCR CITIES/TOWNS FOR THE YEAR 2011 AND ---- NATIONAL CAPITAL REGION GROUND WATER 2021 PROSPECTS I. Haryana ---- POLICY ZONES II. Rajasthan ---- EXISTING SETTLEMENT PATTERN 2001 III. Uttar Pradesh ---- EXISTING TRANSPORT NETWORK (Roads) 2002 7. PROJECTED POPULATION OF NCR CITIES / TOWNS FOR ---- EXISTING TRANSPORT NETWORK (Rail) 2002 THE YEAR 2031 ---- PROPOSED TRANSPORT NETWORK (ROADS) 2021 I. Haryana ---- PROPOSED TRANSPORT NETWORK (RAIL) 2021 II. Rajasthan ---- GROUND WATER RECHARGEABLE AREAS III. Uttar Pradesh ---- MASTER PLAN FOR NOIDA - 2021 ---- MASTER PLAN FOR GREATER NOIDA - 2021 MODIFIED PLANNING & IMPLEMENTATION OF: NCR 1. PRESENT AREA = 30242 SQ.KM. 2. PROPOSED AREA BY 2031 = ___SQ.KM. AFTER ADDING NEW DISTRICTS. 3. PRESENT POPULATION (2017) = ___ M UPS CAMPUS BLOCK-A, PREET VIHAR, 4. PREDICTED POPULATION (2031) = ___ M DELHI-92 (M) 09811018374 E-mail: [email protected] R.G.GUPTA www.rgplan.org, www.rgedu.org, www.uict.org City/Policy Planner NATIONAL CAPITAL REGION TO PREPARATION, ENFORCEMENT AND 5. -

Physico-Chemical Assessment of Ganga Canal (Ghaziabad)
PHYSICO-CHEMICAL ASSESSMENT OF GANGA CANAL (GHAZIABAD) Monu Sharma1, Mohan Lala Verma2, Manish Tewatia3 4 5 6 Shubam Kumar , Bhanu Pratap Singh , Pranay Kumar 1,2,3,4,5,6 Department of Civil Engineering, SRM University,NCR Campus Modinagar (Ghaziabad) (India) ABSTRACT The piece of investigation was carried out to study the canal water as quality, nutrient status and Physico- chemical characteristic of Ghaziabad district of Uttar Pradesh, India. River water samples collected from residential area in 3 different locations were analyzed according to standard methods. The physical-chemical parameters such as pH, TSS, TDS, ALKALINITY, CHLORIDE, TOTAL HARDNESS, PHOSPHATE, SULPHATE, NITRATE, BOD, COD, DO, TURBIDITY, COLOUR, MAGNISIUM HARDNESS and CALCIUM HARDNESS have been analyzed. The results revealed that among the residential locations, many of the estimated physical-chemical parameters of residential areas are more or less with the permissible limits of WHO. Keywords: Quality, Parameter, Samples, Permissible limit. I. INTRODUCTION Water is an essential part of human being for living. A man can live without food for several days but he cannot live not more than four days without water. If there is any impurity in water then it may be hazardous for human being as well as agriculture so that the very important part of human being should be free from any impurity. The rapid rate of industrialization and urbanization in India has changed the face of urban landscape and brought in its wake problems of surface water contamination imperiling human beings. Effluents released from various industries are dumped into open pits or unlined channels without any treatment which contaminate canal water sources. -

Village Dasna P.S. Masuri, Gzb Mehrajuddin 9015499637 Village Shahpur, Dasna Gzb Mahi W/O Bhupende R 7011715175 Zafar Colony
CONTAINMENT ZONE INFORMATION OF DISTRICT GHAZIABAD Police Station Numb NAME OF Name of epi-centre PATIENT MOB. NO NO.OF CASES DATE OF SELLING Expected er of CONTAINMENT NAME Desealing Date ( Contai ZONE/ Hotspot if next 14 days nment Area no another Zone positive will be found) MASURI 1 DASNA ZONE VILLAGE DASNA P.S. MASURI, GZB MEHRAJUDDIN 9015499637 1 10-06-2020 20/10/2020 VILLAGE SHAHPUR, DASNA GZB MAHI W/O 7011715175 1 10-06-2020 20/10/2020 BHUPENDE R MASURI 2 MASURI ZAFAR COLONY NTPC ROAD MASURI FIZA CARE 9810565607 1 10-06-2020 20/10/2020 GZB GYASUDDI N MASURI 3 INDRA GARHI H.No - C-40 sadhbhawana nagar, madhu 8920007206 1 28/9/2020 10-11-2020 dasna, ghaziabad sharma FLAT NO 38, ROYAL GARDEN ARUN 9999145990 1 10-05-2020 19/10/2020 GANGAPURAM, GZB. KUMAR VILLAGE INDERGARHI NEAR PRIMARY DINESH S/O 9891843628 1 10-06-2020 20/10/2020 SCHOOL GZB PINTU MURADNAGA 4 MORTA VILLAGE SHAHPUR MORTA NEAR MONU 9899920787 1 10-09-2020 23/10/2020 R CANARA BANK GHAZIABAD SHARMA S/O SHIV MURADNAGA 5 DUHAI H.NO. 64 GARDEN ENCLAVE-II DUHAI REKHAKUMAR W/O 9560080539 1 10-08-2020 22/10/2020 R GZB ASHISH H.NO. 63, VILLAGE DUHAI, MEERUT RAKESH 7838413938 1 10-05-2020 19/10/2020 ROAD, GZB. TYAGI DEVANAND H.NO-85 MADHU VIHAR KHORA SHAH SON OF MADHU 1 9716453734 28-09-2020 11-10-2020 6 COLONY SEC-1 VAISHALI GZB DWARIKA VIHAR SAH 65 Madhu Vihar KHODA GZB 1 SIZARA DEVI 9319942744 28-09-2020 11-10-2020 2/80, GANG VIHAR, KHODA GANGA RADHA 7 COLONY GZB 2/80, GANG VIHAR, 1 9582322966 30-09-2020 14-10-2020 VIHAR MEHTA KHODA COLONY GZB G-222, DEEPAK VIHAR, KHORA DEEPAK 8 COLONY G-222, DEEPAK VIHAR, 1 SHANKER 9027993561 30-09-2020 14-10-2020 VIHAR KHORA COLONY RC-422 AZAD VIHAR KHODA 1 RAHUL JAIN 7011168893 10-06-2020 20-10-2020 COLONY GZB 9 AZAD VIHAR Rahul Jain RC 422, Azad Vihar, Khoda Colony 1 Son Lt. -

District Disaster Management Authority Ghaziabad District Administration, Collectorate Ghaziabad, Tel
Ghaziabad CITY DISASTER MANAGEMENT PLAN District Disaster Management Authority Ghaziabad District Administration, Collectorate Ghaziabad, Tel. No. 0120- 2824416, 2820106, 2822901, 2822902, Fax: 0120-2828798, Web: www.ghaziabad.nic.in GOI-UNDP Urban Risk Reduction Project Ghaziabad District City Disaster Management Plan 2011-2012 FORWORD The City Disaster Management Plan (CDMP) outlining the measures to be taken in the event of any natural or man-made disaster during the year 2011-2012 has been prepared on the basis of past experiences. The CDMP includes the facts and figures those have been collected from various sources with a view to meet the challenges during any Natural Disaster, while formulating the City Disaster Management Plan, instruction of Relief Commissioner, and also valuable suggestions of District Disaster Management Committee, have been taken into account. The plan is prepared to help the District Administration focus quickly on the essentials and crucial aspects of both preparedness and response. The plan deals with Risk Assessment and Vulnerability Analysis, Identification of Disaster Prone Areas, Response Structures, Inventory of Resources, Standard Operating Procedures, Directory of Institutions and key individuals etc. It is suggested that the District Level Officials who are in-charge of different departments will carefully go through the CDMP and remain alert to effectively countenance any emergent situations that may arise at any point of time. The CDMP is desired to serve as a useful handbook of operational guidelines for all concerned officials of the district, It is expected that District level Officials working in Ghaziabad District in different Departments will thoroughly acquaint themselves with these guidelines and also with the relevant provisions of Relief Code and CRF Guide Line. -

Kavinagar Ad-57 Avantika Gzb Gz 04-03-2021 17-04-2021
CONTAINMENT ZONE INFORMATION OF DISTRICT GHAZIABAD 09-04-2021 Expected NAME OF Desealing Date Police Station CONTAINMENT Name of epi-centre sealing date ( if next 14 days ZONE/ Hotspot Area no another positive will be found) KAVINAGAR AD-57 AVANTIKA GZB GZ 04-03-2021 17-04-2021 KAVINAGAR BE 281/SF 1 AVANTIKA 04-07-2021 21-04-2021 SE-139, SHASTRI KAVINAGAR NAGAR, CHIRANJEEV 04-08-2021 22-04-2021 VIHAR SE-139, SHASTRI KAVINAGAR NAGAR, CHIRANJEEV 04-08-2021 22-04-2021 VIHAR Chiranjivi Vihar SE-139, SHASTRI KAVINAGAR NAGAR, CHIRANJEEV 04-08-2021 22-04-2021 VIHAR 22 SEC-9 CHIRANJEEV KAVINAGAR 04-08-2021 22-04-2021 VIHAR 36 A SEC 5 CHIRANJEEV KAVINAGAR 04-07-2021 21-04-2021 VIHAR 22 SEC-9 CHIRANJEEV KAVINAGAR 04-07-2021 21-04-2021 VIHAR KAVINAGAR KF KAVINAGAR KF-40, KAVI NAGAR, GZB 04-07-2021 21-04-2021 KAVINAGAR KJ KAVINAGAR KJ - 29 KAVI NAGAR 31-03-2021 13-04-2021 KE-92/A KAVI NAGAR KAVINAGAR KE KAVINAGAR GZB 259-F RAM NAGAR 04-07-2021 21-04-2021 GZB KAVINAGAR KI-151, KAVI NAGAR 04-07-2021 21-04-2021 KI KAVINAGAR KAVINAGAR KI-151, KAVI NAGAR 04-07-2021 21-04-2021 KAVINAGAR KH-94, KAVI NAGAR 04-07-2021 21-04-2021 KAVINAGAR KH KAVINAGAR KH-94, KAVI NAGAR 04-07-2021 21-04-2021 KAVINAGAR KH-44, KAVI NAGAR 04-07-2021 21-04-2021 KAVINAGAR KC-E-79, KAVI NAGAR 04-07-2021 21-04-2021 KAVINAGAR KC KAVINAGAR KC-E-79, KAVI NAGAR 04-07-2021 21-04-2021 KAVINAGAR KC-135, KAVI NAGA 04-03-2021 17-04-2021 KAVINAGAR SEC 2 RAJ NAGAR 2/227 , RAJNAGAR GZB 04-07-2021 21-04-2021 KAVINAGAR SEC 10 RAJ R-10/116, RAJ NAGAR 04-07-2021 21-04-2021 KAVINAGAR NAGAR R-10/116, -

National Heal National Health Miss Th Mission
NATIONAL HEALTH MISS ION MONITORING OF IMPORT ANT COMPONENTS OF NH M PROGRAMME IMPLEMENTATION PLAN IN GHAZIABAD DISTRICT , UTTAR PRADESH SUBMITTED TO MINISTRY OF HEALTH A ND FAMILY WELFARE GOVERNMENT OF INDIA DR. RUBY A. SINGH MS. ADITI SINGH POPULATION RESEARCH CENTRE INSTITUTE OF ECONOMIC GROWTH, DELHI UNIVERSITY, DE LHI-110007 NOVEMBER 2017 NHM UTTAR PRADESH PIP 2017: GHAZIABAD DISTRICT PRC-IEG, DELHI TABLE OF CONTENTS NATIONAL HEALTH MISSION ......................................................................................................................... 1 TABLE OF CONTENTS ............................................................................................................................................. 1 LIST OF TABLES ..................................................................................................................................................... 3 LIST OF FIGURES ................................................................................................................................................... 4 ACKNOWLEDGEMENT ........................................................................................................................................... 5 ACRONYMS AND ABBREVIATIONS ......................................................................................................................... 6 EXECUTIVE SUMMARY .......................................................................................................................................... 7 Strengths ................................................................................................................................................................... -

E-Auction 09.03.2021
THE JAMMU & KASHMIR BANK LIMITED Impaired Asset Portfolio Management Department, Zonal Office (North) Plot No.132-134 Sector 44, Gurgaon (Haryana) T+91 (0)0124-4715800, F+91 (0)0124-4715800 E [email protected], W www.jkbank.net E-AUCTION NOTICE (For sale of Immovable Mortgaged Property/ies under the SARFAESI Act, 2002) [Refer Proviso to rule 8(6)] Notice is hereby given to the public in general and to the borrowers and guarantors in particular that the below mentioned immovable properties mortgaged to The Jammu & Kashmir Bank Ltd., Business Unit Ghaziabad, the physical possession of which has been taken by the Authorised officer of the bank under Section 13(4) of the SARFAESI Act, will be sold through E-auction on “AS IS WHERE IS” “AS IS WHAT IS” AND “WHATEVER THERE IS” basis on 26-03-2021, for recovery of dues to The Jammu & Kashmir Bank Ltd from below mentioned borrower(s), mortgagor(s) and guarantor(s). The reserve price and Earnest money deposit (EMD) is displayed against the details of respective properties Description of Properties to be auctioned on 26-03-2021 (15 days notice) (Amount in Lacs) S. Name of the Borrower(s)/ Description of Property Demand Notice Reserve EMD No Mortgagor(s)/ Guarantor(s) Date & Amount Price 1. (1) M/s D.P. Steels Registered Office:-208, IInd floor, Flat No. G-1, Ground Floor (Front Side) 07.04.2015 Rs. Rs. Ansal Sumedha RDC Raj nagar, Ghaziabad (U.P.) having covered area measuring 1500 Rs. 2,12,57,162.22 155.29 15.53 Also at:- Shop no. -
Remote Sensing for Settlement Patterns in Metropolitan Regions: the Case of National Capital Region (Ncr) of Delhi, India
REMOTE SENSING FOR SETTLEMENT PATTERNS IN METROPOLITAN REGIONS: THE CASE OF NATIONAL CAPITAL REGION (NCR) OF DELHI, INDIA Mahavir Centre for Remote Sensing, School of Planning and Architecture, 4-B, I. P. Estate, New Delhi 110002, INDIA [email protected] KEY WORDS: Settlement Patterns, Metropolitan Regions, Remote Sensing, Continuously Built-up Area, NCR, Delhi ABSTRACT: The author earlier conducted a research, attempting to make two models, one for understanding, monitoring and describing settlement patterns in metropolitan regions, dependant primarily on remotely sensed data; and the second, for predicting settlement patterns in such regions, using National Capital Region (NCR), of Delhi, India, as a case study. As part of the model, a transferable approach of the ‘Continuously Built-up Area’ (CBA) was adopted, which allows identification of settlements at different levels of generalization. With the capability of providing frequent and synoptic views over large areas, remotely sensed data (e.g., satellite images) proved to be a useful base for carrying out macro-analyses of settlement patterns, at frequent intervals. The model for prediction was applied for the target year of 2001. About 10 years have passed by since the base year of data collection. While the region has changed tremendously during these years, recent data (Census of India, 2001) pertaining to the then target year (2001) is also now available. The moment is also apt, keeping in mind that the Regional Plan – 2001 National Capital Region has now expired and the Draft Regional Plan - 2021 has just come in. This paper reviews the models for 2001. It has been found that the predictions made by the model with regard to settlements becoming `towns’, CBAs and couples have largely come true.