1 NCCP Technology Review Committee (TRC) Meeting Notes
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

A Phase I Trial of Tamoxifen with Ribociclib (LEE011) in Adult Patients with Advanced ER+ (HER2 Negative) Breast Cancer
The TEEL Study: A Phase I Trial of Tamoxifen with Ribociclib (LEE011) in Adult Patients with Advanced ER+ (HER2 Negative) Breast Cancer NCT02586675 Version 12.0 September 14, 2016 TEEL Protocol- Tamoxifen +Ribociclib Page 1 TITLE PAGE The TEEL Study: A Phase I trial of Tamoxifen with Ribociclib (LEE011) in adult patients with advanced ER+ (HER2 negative) breast cancer. Protocol: MCC 18332 Chesapeake IRB Pro00015228 Principal Investigator: Co-Investigators: Statistician: Experimental Therapeutics Program H. Lee Moffitt Cancer Center 12902 Magnolia Drive Tampa, FL 33612 & Comprehensive Breast Program Moffitt McKinley Outpatient Center 10920 N. McKinley Dr. Tampa, FL 33612 Study Site Contact: Protocol Version 12 Date: September 14, 2016 TEEL Protocol- Tamoxifen +Ribociclib Page 2 TITLE PAGE .............................................................................................................................................. 1 SYNOPSIS ................................................................................................................................................... 5 Patient Population ................................................................................................................................. 5 Type of Study ......................................................................................................................................... 5 Prior Therapy......................................................................................................................................... 5 -

PD-1/PD-L1 Targeting in Breast Cancer: the First Clinical Evidences Are Emerging
Supplementary Materials: PD-1/PD-L1 Targeting in Breast Cancer: the First Clinical Evidences are Emerging. A Literature Review Table S1. Interventional studies with anti PD-1 or PDL-1 agents recruiting. Non-intraveinous administrations are indicated between brackets. Estimated Estimated Study Ph. Anti-PD(L)-1 Single (S) or Combination Study title NCT Conditions or disease Enrollement Sponsor Completion Date (n=) Inflammatory and metastatic breast cancer (IBC) 1 Pembrolizumab S MK-3475 for Metastatic Inflammatory Breast Cancer (MIBC) 02411656 35 June 2020 MD Anderson or mTNBC Entinostat, Nivolumab, and Ipilimumab in treating patients Breast carcinoma: HER2 negative, Ipilimumab with solid tumors that are metastatic or cannot be removed by Invasive BC, Metastatic BC 1 Entinostat [PO] 02453620 45 December 2019 NCI Nivolumab surgery or locally advanced or metastatic HER2-NegativeBreast BC stage III, IIIA, IIIB, IIIC, IV Cancer Unresectable solid neoplasm Adjuvant PVX-410 Vaccine and Durvalumab in stage II/III TNBC stage II, III; HLA-A2 positive by Massachusetts 1 Durvalumab PVX-410 [IM] 02826434 20 December 2022 Triple Negative Breast Cancer deoxyribonucleic acid (DNA) sequence analysis General Hospit A Study of changes in PD-L1 expression during preoperative Pembrolizumab 1 Nab-paclitaxel treatment with Nab-Paclitaxel and pembrolizumab in Hormone 02999477 HR positive breast cancer 50 January 2023 Dana-Farber Receptor (HR) Positive BC Cisplatine PD1 Antibody + GP as first line treatment for triple negative Fudan 1 JS001 (anti PD1) Gemcitabine -
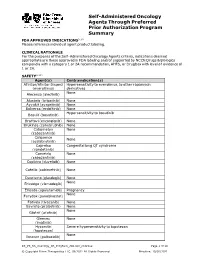
PRIOR AUTHORIZATION CRITERIA for APPROVAL Initial Evaluation Target Agent(S) Will Be Approved When ONE of the Following Is Met: 1
Self-Administered Oncology Agents Through Preferred Prior Authorization Program Summary FDA APPROVED INDICATIONS3-104 Please reference individual agent product labeling. CLINICAL RATIONALE For the purposes of the Self -Administered Oncology Agents criteria, indications deemed appropriate are those approved in FDA labeling and/or supported by NCCN Drugs & Biologics compendia with a category 1 or 2A recommendation, AHFS, or DrugDex with level of evidence of 1 or 2A. SAFETY3-104 Agent(s) Contraindication(s) Afinitor/Afinitor Disperz Hypersensitivity to everolimus, to other rapamycin (everolimus) derivatives None Alecensa (alectinib) Alunbrig (brigatinib) None Ayvakit (avapritinib) None Balversa (erdafitinib) None Hypersensitivity to bosutinib Bosulif (bosutinib) Braftovi (encorafenib) None Brukinsa (zanubrutinib) None Cabometyx None (cabozantinib) Calquence None (acalabrutinib) Caprelsa Congenital long QT syndrome (vandetanib) Cometriq None (cabozantinib) Copiktra (duvelisib) None Cotellic (cobimetinib) None Daurismo (glasdegib) None None Erivedge (vismodegib) Erleada (apalutamide) Pregnancy None Farydak (panobinostat) Fotivda (tivozanib) None Gavreto (pralsetinib) None None Gilotrif (afatinib) Gleevec None (imatinib) Hycamtin Severe hypersensitivity to topotecan (topotecan) None Ibrance (palbociclib) KS_PS_SA_Oncology_PA_ProgSum_AR1020_r0821v2 Page 1 of 19 © Copyright Prime Therapeutics LLC. 08/2021 All Rights Reserved Effective: 10/01/2021 Agent(s) Contraindication(s) None Iclusig (ponatinib) Idhifa (enasidenib) None Imbruvica (ibrutinib) -
Management of Multiple Myeloma: the Changing Paradigm
Management of Multiple Myeloma: The Changing Paradigm Relapsed/Refractory Disease Jeffrey A. Zonder, MD Karmanos Cancer Institute Objectives • Discuss use of standard myeloma therapies when used as therapy after relapse • Consider patient and disease factors which might impact therapy decisions. • Describe off-label options for patients who are not protocol candidates. Line ≠ Line ≠ Line ≠ … POLICE LINE – DO NOT CROSS POLICE LINE – DO NOT CROSS POLICE LINE – DO NOT CROSS POLICE LINE – DO NOT CROSS POLI LINE – DO NOT Define “Line” • A pre-defined course of therapy utilizing agents either simultaneously or sequentially – Len/Dex – Len/Dex ASCT – Vel/Dex ASCT Len/Dex – VDT-PACE ASCT TD ASCT VPT-PACE LD • Pts who have had the same # of “lines” of Rx may have had vastly different amounts of Rx What Is Relapsed/Refractory Disease? • Relapsed: recurrence after a response to therapy • Refractory: progression despite ongoing therapy What Do We Know About the Pt’s Myeloma? • What prior therapy has been used? • How well did it work? • Did the myeloma progress on active therapy? • High-risk cytogenetics/FISH/GEP? What Do We Know About the Patient? • Age • Other medical problems – Diabetes – Blood Clots • Lasting side effects from past therapies – Peripheral Neuropathy • Personal preferences and values Choosing Therapy for Relapsed/Refractory Myeloma Proteasome IMiDs Anthracyclines Alkylators Steroids HDACs Antibodies Inhibitors Thalidomide Bortezomib Doxil Melphalan Dex Panobinostat Elotuzumab Lenalidomide Carfilzomib Cytoxan Pred Vorinostat -

Spotlight on Ixazomib: Potential in the Treatment of Multiple Myeloma Barbara Muz Washington University School of Medicine in St
Washington University School of Medicine Digital Commons@Becker Open Access Publications 2016 Spotlight on ixazomib: Potential in the treatment of multiple myeloma Barbara Muz Washington University School of Medicine in St. Louis Rachel N. Ghazarian Washington University School of Medicine in St. Louis Monica Ou Washington University School of Medicine in St. Louis Micha J. Luderer Washington University School of Medicine in St. Louis Hubert D. Kusdono Washington University School of Medicine in St. Louis See next page for additional authors Follow this and additional works at: https://digitalcommons.wustl.edu/open_access_pubs Recommended Citation Muz, Barbara; Ghazarian, Rachel N.; Ou, Monica; Luderer, Micha J.; Kusdono, Hubert D.; and Azab, Abdel K., ,"Spotlight on ixazomib: Potential in the treatment of multiple myeloma." Drug Design, Development and Therapy.2016,10. 217-226. (2016). https://digitalcommons.wustl.edu/open_access_pubs/5207 This Open Access Publication is brought to you for free and open access by Digital Commons@Becker. It has been accepted for inclusion in Open Access Publications by an authorized administrator of Digital Commons@Becker. For more information, please contact [email protected]. Authors Barbara Muz, Rachel N. Ghazarian, Monica Ou, Micha J. Luderer, Hubert D. Kusdono, and Abdel K. Azab This open access publication is available at Digital Commons@Becker: https://digitalcommons.wustl.edu/open_access_pubs/5207 Journal name: Drug Design, Development and Therapy Article Designation: Review Year: 2016 Volume: -

BC Cancer Benefit Drug List September 2021
Page 1 of 65 BC Cancer Benefit Drug List September 2021 DEFINITIONS Class I Reimbursed for active cancer or approved treatment or approved indication only. Reimbursed for approved indications only. Completion of the BC Cancer Compassionate Access Program Application (formerly Undesignated Indication Form) is necessary to Restricted Funding (R) provide the appropriate clinical information for each patient. NOTES 1. BC Cancer will reimburse, to the Communities Oncology Network hospital pharmacy, the actual acquisition cost of a Benefit Drug, up to the maximum price as determined by BC Cancer, based on the current brand and contract price. Please contact the OSCAR Hotline at 1-888-355-0355 if more information is required. 2. Not Otherwise Specified (NOS) code only applicable to Class I drugs where indicated. 3. Intrahepatic use of chemotherapy drugs is not reimbursable unless specified. 4. For queries regarding other indications not specified, please contact the BC Cancer Compassionate Access Program Office at 604.877.6000 x 6277 or [email protected] DOSAGE TUMOUR PROTOCOL DRUG APPROVED INDICATIONS CLASS NOTES FORM SITE CODES Therapy for Metastatic Castration-Sensitive Prostate Cancer using abiraterone tablet Genitourinary UGUMCSPABI* R Abiraterone and Prednisone Palliative Therapy for Metastatic Castration Resistant Prostate Cancer abiraterone tablet Genitourinary UGUPABI R Using Abiraterone and prednisone acitretin capsule Lymphoma reversal of early dysplastic and neoplastic stem changes LYNOS I first-line treatment of epidermal -

UC Irvine UC Irvine Previously Published Works
UC Irvine UC Irvine Previously Published Works Title ACTR-10. A RANDOMIZED, PHASE I/II TRIAL OF IXAZOMIB IN COMBINATION WITH STANDARD THERAPY FOR UPFRONT TREATMENT OF PATIENTS WITH NEWLY DIAGNOSED MGMT METHYLATED GLIOBLASTOMA (GBM) STUDY DESIGN Permalink https://escholarship.org/uc/item/2w97d9jv Journal Neuro-Oncology, 20(suppl_6) ISSN 1522-8517 Authors Kong, Xiao-Tang Lai, Albert Carrillo, Jose A et al. Publication Date 2018-11-05 DOI 10.1093/neuonc/noy148.045 Peer reviewed eScholarship.org Powered by the California Digital Library University of California Abstracts 3 dyspnea; grade 2 hemorrhage, non-neutropenic fever; and grade 1 hand- toxicities include: 1 patient with pre-existing vision dysfunction had Grade foot. CONCLUSIONS: Low-dose capecitabine is associated with a modest 4 optic nerve dysfunction; 2 Grade 4 hematologic events and 1 Grade 5 reduction in MDSCs and T-regs and a significant increase in CTLs. Toxicity event(sepsis) due to temozolamide-induced cytopenias. CONCLUSION: has been manageable. Four of 7 evaluable patients have reached 6 months 18F-DOPA-PET -guided dose escalation appears reasonably safe and toler- free of progression. Dose escalation continues. able in patients with high-grade glioma. ACTR-10. A RANDOMIZED, PHASE I/II TRIAL OF IXAZOMIB IN ACTR-13. A BAYESIAN ADAPTIVE RANDOMIZED PHASE II TRIAL COMBINATION WITH STANDARD THERAPY FOR UPFRONT OF BEVACIZUMAB VERSUS BEVACIZUMAB PLUS VORINOSTAT IN TREATMENT OF PATIENTS WITH NEWLY DIAGNOSED MGMT ADULTS WITH RECURRENT GLIOBLASTOMA FINAL RESULTS Downloaded from https://academic.oup.com/neuro-oncology/article/20/suppl_6/vi13/5153917 by University of California, Irvine user on 27 May 2021 METHYLATED GLIOBLASTOMA (GBM) STUDY DESIGN Vinay Puduvalli1, Jing Wu2, Ying Yuan3, Terri Armstrong2, Jimin Wu3, Xiao-Tang Kong1, Albert Lai2, Jose A. -

Drug Name Plate Number Well Location % Inhibition, Screen Axitinib 1 1 20 Gefitinib (ZD1839) 1 2 70 Sorafenib Tosylate 1 3 21 Cr
Drug Name Plate Number Well Location % Inhibition, Screen Axitinib 1 1 20 Gefitinib (ZD1839) 1 2 70 Sorafenib Tosylate 1 3 21 Crizotinib (PF-02341066) 1 4 55 Docetaxel 1 5 98 Anastrozole 1 6 25 Cladribine 1 7 23 Methotrexate 1 8 -187 Letrozole 1 9 65 Entecavir Hydrate 1 10 48 Roxadustat (FG-4592) 1 11 19 Imatinib Mesylate (STI571) 1 12 0 Sunitinib Malate 1 13 34 Vismodegib (GDC-0449) 1 14 64 Paclitaxel 1 15 89 Aprepitant 1 16 94 Decitabine 1 17 -79 Bendamustine HCl 1 18 19 Temozolomide 1 19 -111 Nepafenac 1 20 24 Nintedanib (BIBF 1120) 1 21 -43 Lapatinib (GW-572016) Ditosylate 1 22 88 Temsirolimus (CCI-779, NSC 683864) 1 23 96 Belinostat (PXD101) 1 24 46 Capecitabine 1 25 19 Bicalutamide 1 26 83 Dutasteride 1 27 68 Epirubicin HCl 1 28 -59 Tamoxifen 1 29 30 Rufinamide 1 30 96 Afatinib (BIBW2992) 1 31 -54 Lenalidomide (CC-5013) 1 32 19 Vorinostat (SAHA, MK0683) 1 33 38 Rucaparib (AG-014699,PF-01367338) phosphate1 34 14 Lenvatinib (E7080) 1 35 80 Fulvestrant 1 36 76 Melatonin 1 37 15 Etoposide 1 38 -69 Vincristine sulfate 1 39 61 Posaconazole 1 40 97 Bortezomib (PS-341) 1 41 71 Panobinostat (LBH589) 1 42 41 Entinostat (MS-275) 1 43 26 Cabozantinib (XL184, BMS-907351) 1 44 79 Valproic acid sodium salt (Sodium valproate) 1 45 7 Raltitrexed 1 46 39 Bisoprolol fumarate 1 47 -23 Raloxifene HCl 1 48 97 Agomelatine 1 49 35 Prasugrel 1 50 -24 Bosutinib (SKI-606) 1 51 85 Nilotinib (AMN-107) 1 52 99 Enzastaurin (LY317615) 1 53 -12 Everolimus (RAD001) 1 54 94 Regorafenib (BAY 73-4506) 1 55 24 Thalidomide 1 56 40 Tivozanib (AV-951) 1 57 86 Fludarabine -

CNS Penetration of the CDK4/6 Inhibitor Ribociclib in Non-Tumor
Cancer Chemotherapy and Pharmacology (2019) 84:447–452 https://doi.org/10.1007/s00280-019-03864-9 SHORT COMMUNICATION CNS penetration of the CDK4/6 inhibitor ribociclib in non‑tumor bearing mice and mice bearing pediatric brain tumors Yogesh T. Patel1,2 · Abigail Davis1 · Suzanne J. Baker3 · Olivia Campagne1 · Clinton F. Stewart1 Received: 22 January 2019 / Accepted: 3 May 2019 / Published online: 11 May 2019 © Springer-Verlag GmbH Germany, part of Springer Nature 2019 Abstract Purpose Ribociclib, an orally bioavailable small-molecule CDK4/6 inhibitor is currently undergoing evaluation to treat pedi- atric central nervous system (CNS) tumors. However, it is crucial that it penetrates the brain and tumor. Thus, the objectives of the present study were to derive a clinically relevant mouse dosage for cerebral microdialysis studies, and to characterize ribociclib CNS penetration in non-tumor bearing mice and in mice bearing DIPGx7 (glioma) cortical allograft tumors. Methods A plasma pharmacokinetic study of ribociclib (100 mg/kg, orally) was performed in CD1 nude mice bearing glioma cortical allografts to obtain initial plasma pharmacokinetic parameters and to derive D-optimal plasma sampling time-points for microdialysis studies. Using a cerebral microdialysis technique, the extracellular fuid (ECF) disposition of ribociclib was evaluated after a single oral ribociclib dose (100 mg/kg) in non-tumor bearing mice and in mice bearing glioma cortical allografts. A one-compartment plasma model with absorption and ECF compartments were ft to plasma and ECF concentration–time data using a nonlinear mixed efects modeling approach (NONMEM 7.2). Results The mean unbound ribociclib plasma exposure (6812 ng/ml*h) was similar to that observed clinically at recom- mended dosages in adults. -

New Drug Update: the Next Step in Personalized Medicine
New Drug Update: The Next Step in Personalized Medicine Jordan Hill, PharmD, BCOP Clinical Pharmacy Specialist WVU Medicine Mary Babb Randolph Cancer Center Objectives • Review indications for new FDA approved anti- neoplastic medications in 2017 • Outline place in therapy of new medications • Become familiar with mechanisms of action of new medications • Describe adverse effects associated with new medications • Summarize dosing schemes and appropriate dose reductions for new medications First-in-Class Approvals • FLT3 inhibitor – midostaurin • IDH2 inhibitor – enasidenib • Anti-CD22 antibody drug conjugate – inotuzumab ozogamicin • CAR T-cell therapy - tisagenlecleucel “Me-too” Approvals • CDK 4/6 inhibitor – ribociclib and abemaciclib • PD-L1 inhibitors • Avelumab • Durvalumab • PARP inhibitor – niraparib • ALK inhibitor – brigatinib • Pan-HER inhibitor – neratinib • Liposome-encapsulated combination of daunorubicin and cytarabine • PI3K inhibitor – copanlisib Drugs by Malignancy AML Breast Bladder ALL FL Lung Ovarian 0 1 2 3 Oral versus IV 46% 54% Oral IV FIRST-IN CLASS FLT3 Inhibitor - midostaurin Journal of Hematology & Oncology 2017;10:93 Midostaurin (Rydapt®) • 717 newly diagnosed FLT3+ AML Patients • Induction and consolidation chemotherapy and placebo maintenance versus chemotherapy + midostaurin and Treatment maintenance midostaurin • OS: 74.7 mo versus 25.6 mo (P=0.009) Efficacy • EFS: 8.2 mo versus 3.0 mo (P=0.002) • Higher grade > 3 anemia, rash, and nausea Safety N Engl J Med 2017;377:454-64 Midostaurin (Rydapt®) • Approved indications: FLT3+ AML, mast cell leukemia, systemic mastocytosis • AML dose: 50 mg twice daily with food on days 8-21 • Of each induction cycle (+ daunorubicin and cytarabine) • Of each consolidation cycle (+ high dose cytarabine) • ADEs: nausea, myelosuppression, mucositis, increases in LFTs, amylase/lipase, and electrolyte abnormalities • Pharmacokinetics: hepatic metabolism, substrate of CYP 3A4; < 5% excretion in urine RYDAPT (midostaurin) [package insert]. -

A Novel Treatment for Triple-Negative Breast Cancer
Huateng Pharma https://en.huatengsci.com A Novel Treatment For Triple-negative Breast Cancer Triple-negative breast cancer is a cancer that tests negative for estrogen receptors, progesterone receptors, and excess HER2 protein. These results mean the growth of the cancer is not fueled by the hormones estrogen and progesterone, or by the HER2 protein. So, triple-negative breast cancer does not respond to hormonal therapy medicines or medicines that target HER2 protein receptors. This type of breast cancer accounts for 10-20% of all types of breast cancer. It has special biological behavior and clinicopathological characteristics, and the prognosis is worse than other types. For doctors and researchers, there is intense interest in finding new medications that can treat this kind of breast cancer. Photodynamic therapy is a novel method for the treatment of breast cancer. By combining a photosensitizer with a corresponding light source, reactive oxygen species (ROS) are generated to selectively destroy the diseased tissues, so as to kill the cancer cells. But at the same time it will also lead to the formation of hypoxia in tumor tissues and reduce the therapeutic effect. Recently, the team of Professor Jin Hongjun from the Molecular Imaging Center of Sun Yat-sen University No.5 Hospital and the Tumor Center of Sun Yat-sen University No.5 Hospital explored a novel method to improve hypoxia in photodynamic therapy, and Huateng Pharma https://en.huatengsci.com preliminarily found that oxyphotodynamic therapy combined with metformin has the potential to treat triple-negative breast cancer. The research was published in the Annals of Translational Medicine (ATM,IF:3.297). -

Ribociclib (LEE011)
Clinical Development Ribociclib (LEE011) Oncology Clinical Protocol CLEE011G2301 (EarLEE-1) / NCT03078751 An open label, multi-center protocol for U.S. patients enrolled in a study of ribociclib with endocrine therapy as an adjuvant treatment in patients with hormone receptor-positive, HER2- negative, high risk early breast cancer Authors Document type Amended Protocol Version EUDRACT number 2014-001795-53 Version number 02 (Clean) Development phase II Document status Final Release date 17-Apr-2018 Property of Novartis Confidential May not be used, divulged, published or otherwise disclosed without the consent of Novartis Template version 22-Jul-2016 Novartis Confidential Page 2 Amended Protocol Version 02 (Clean) Protocol No. CLEE011G2301 Table of contents Table of contents ................................................................................................................. 2 List of tables ........................................................................................................................ 5 List of abbreviations ............................................................................................................ 6 Glossary of terms ................................................................................................................. 9 Protocol summary .............................................................................................................. 10 Amendment 2 (17-Apr-2018) ............................................................................................ 14