Ribociclib (LEE011)
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

A Phase I Trial of Tamoxifen with Ribociclib (LEE011) in Adult Patients with Advanced ER+ (HER2 Negative) Breast Cancer
The TEEL Study: A Phase I Trial of Tamoxifen with Ribociclib (LEE011) in Adult Patients with Advanced ER+ (HER2 Negative) Breast Cancer NCT02586675 Version 12.0 September 14, 2016 TEEL Protocol- Tamoxifen +Ribociclib Page 1 TITLE PAGE The TEEL Study: A Phase I trial of Tamoxifen with Ribociclib (LEE011) in adult patients with advanced ER+ (HER2 negative) breast cancer. Protocol: MCC 18332 Chesapeake IRB Pro00015228 Principal Investigator: Co-Investigators: Statistician: Experimental Therapeutics Program H. Lee Moffitt Cancer Center 12902 Magnolia Drive Tampa, FL 33612 & Comprehensive Breast Program Moffitt McKinley Outpatient Center 10920 N. McKinley Dr. Tampa, FL 33612 Study Site Contact: Protocol Version 12 Date: September 14, 2016 TEEL Protocol- Tamoxifen +Ribociclib Page 2 TITLE PAGE .............................................................................................................................................. 1 SYNOPSIS ................................................................................................................................................... 5 Patient Population ................................................................................................................................. 5 Type of Study ......................................................................................................................................... 5 Prior Therapy......................................................................................................................................... 5 -

Prospective Study on Gynaecological Effects of Two Antioestrogens Tamoxifen and Toremifene in Postmenopausal Women
British Journal of Cancer (2001) 84(7), 897–902 © 2001 Cancer Research Campaign doi: 10.1054/ bjoc.2001.1703, available online at http://www.idealibrary.com on http://www.bjcancer.com Prospective study on gynaecological effects of two antioestrogens tamoxifen and toremifene in postmenopausal women MB Marttunen1, B Cacciatore1, P Hietanen2, S Pyrhönen2, A Tiitinen1, T Wahlström3 and O Ylikorkala1 1Departments of Obstetrics and Gynecology, Helsinki University Central Hospital, P.O. Box 140, FIN-00029 HYKS, Finland; 2Department of Oncology, Helsinki University Central Hospital, P.O. Box 180, FIN-00029 HYKS, Finland; 3Department of Pathology, Helsinki University Central Hospital, P.O. Box 140, FIN-00029 HYKS, Finland Summary To assess and compare the gynaecological consequences of the use of 2 antioestrogens we examined 167 postmenopausal breast cancer patients before and during the use of either tamoxifen (20 mg/day, n = 84) or toremifene (40 mg/day, n = 83) as an adjuvant treatment of stage II–III breast cancer. Detailed interview concerning menopausal symptoms, pelvic examination including transvaginal sonography (TVS) and collection of endometrial sample were performed at baseline and at 6, 12, 24 and 36 months of treatment. In a subgroup of 30 women (15 using tamoxifen and 15 toremifene) pulsatility index (PI) in an uterine artery was measured before and at 6 and 12 months of treatment. The mean (±SD) follow-up time was 2.3 ± 0.8 years. 35% of the patients complained of vasomotor symptoms before the start of the trial. This rate increased to 60.0% during the first year of the trial, being similar among patients using tamoxifen (57.1%) and toremifene (62.7%). -

PD-1/PD-L1 Targeting in Breast Cancer: the First Clinical Evidences Are Emerging
Supplementary Materials: PD-1/PD-L1 Targeting in Breast Cancer: the First Clinical Evidences are Emerging. A Literature Review Table S1. Interventional studies with anti PD-1 or PDL-1 agents recruiting. Non-intraveinous administrations are indicated between brackets. Estimated Estimated Study Ph. Anti-PD(L)-1 Single (S) or Combination Study title NCT Conditions or disease Enrollement Sponsor Completion Date (n=) Inflammatory and metastatic breast cancer (IBC) 1 Pembrolizumab S MK-3475 for Metastatic Inflammatory Breast Cancer (MIBC) 02411656 35 June 2020 MD Anderson or mTNBC Entinostat, Nivolumab, and Ipilimumab in treating patients Breast carcinoma: HER2 negative, Ipilimumab with solid tumors that are metastatic or cannot be removed by Invasive BC, Metastatic BC 1 Entinostat [PO] 02453620 45 December 2019 NCI Nivolumab surgery or locally advanced or metastatic HER2-NegativeBreast BC stage III, IIIA, IIIB, IIIC, IV Cancer Unresectable solid neoplasm Adjuvant PVX-410 Vaccine and Durvalumab in stage II/III TNBC stage II, III; HLA-A2 positive by Massachusetts 1 Durvalumab PVX-410 [IM] 02826434 20 December 2022 Triple Negative Breast Cancer deoxyribonucleic acid (DNA) sequence analysis General Hospit A Study of changes in PD-L1 expression during preoperative Pembrolizumab 1 Nab-paclitaxel treatment with Nab-Paclitaxel and pembrolizumab in Hormone 02999477 HR positive breast cancer 50 January 2023 Dana-Farber Receptor (HR) Positive BC Cisplatine PD1 Antibody + GP as first line treatment for triple negative Fudan 1 JS001 (anti PD1) Gemcitabine -
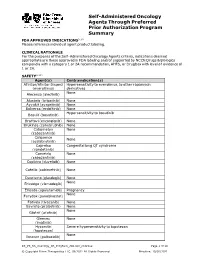
PRIOR AUTHORIZATION CRITERIA for APPROVAL Initial Evaluation Target Agent(S) Will Be Approved When ONE of the Following Is Met: 1
Self-Administered Oncology Agents Through Preferred Prior Authorization Program Summary FDA APPROVED INDICATIONS3-104 Please reference individual agent product labeling. CLINICAL RATIONALE For the purposes of the Self -Administered Oncology Agents criteria, indications deemed appropriate are those approved in FDA labeling and/or supported by NCCN Drugs & Biologics compendia with a category 1 or 2A recommendation, AHFS, or DrugDex with level of evidence of 1 or 2A. SAFETY3-104 Agent(s) Contraindication(s) Afinitor/Afinitor Disperz Hypersensitivity to everolimus, to other rapamycin (everolimus) derivatives None Alecensa (alectinib) Alunbrig (brigatinib) None Ayvakit (avapritinib) None Balversa (erdafitinib) None Hypersensitivity to bosutinib Bosulif (bosutinib) Braftovi (encorafenib) None Brukinsa (zanubrutinib) None Cabometyx None (cabozantinib) Calquence None (acalabrutinib) Caprelsa Congenital long QT syndrome (vandetanib) Cometriq None (cabozantinib) Copiktra (duvelisib) None Cotellic (cobimetinib) None Daurismo (glasdegib) None None Erivedge (vismodegib) Erleada (apalutamide) Pregnancy None Farydak (panobinostat) Fotivda (tivozanib) None Gavreto (pralsetinib) None None Gilotrif (afatinib) Gleevec None (imatinib) Hycamtin Severe hypersensitivity to topotecan (topotecan) None Ibrance (palbociclib) KS_PS_SA_Oncology_PA_ProgSum_AR1020_r0821v2 Page 1 of 19 © Copyright Prime Therapeutics LLC. 08/2021 All Rights Reserved Effective: 10/01/2021 Agent(s) Contraindication(s) None Iclusig (ponatinib) Idhifa (enasidenib) None Imbruvica (ibrutinib) -

BC Cancer Benefit Drug List September 2021
Page 1 of 65 BC Cancer Benefit Drug List September 2021 DEFINITIONS Class I Reimbursed for active cancer or approved treatment or approved indication only. Reimbursed for approved indications only. Completion of the BC Cancer Compassionate Access Program Application (formerly Undesignated Indication Form) is necessary to Restricted Funding (R) provide the appropriate clinical information for each patient. NOTES 1. BC Cancer will reimburse, to the Communities Oncology Network hospital pharmacy, the actual acquisition cost of a Benefit Drug, up to the maximum price as determined by BC Cancer, based on the current brand and contract price. Please contact the OSCAR Hotline at 1-888-355-0355 if more information is required. 2. Not Otherwise Specified (NOS) code only applicable to Class I drugs where indicated. 3. Intrahepatic use of chemotherapy drugs is not reimbursable unless specified. 4. For queries regarding other indications not specified, please contact the BC Cancer Compassionate Access Program Office at 604.877.6000 x 6277 or [email protected] DOSAGE TUMOUR PROTOCOL DRUG APPROVED INDICATIONS CLASS NOTES FORM SITE CODES Therapy for Metastatic Castration-Sensitive Prostate Cancer using abiraterone tablet Genitourinary UGUMCSPABI* R Abiraterone and Prednisone Palliative Therapy for Metastatic Castration Resistant Prostate Cancer abiraterone tablet Genitourinary UGUPABI R Using Abiraterone and prednisone acitretin capsule Lymphoma reversal of early dysplastic and neoplastic stem changes LYNOS I first-line treatment of epidermal -

CNS Penetration of the CDK4/6 Inhibitor Ribociclib in Non-Tumor
Cancer Chemotherapy and Pharmacology (2019) 84:447–452 https://doi.org/10.1007/s00280-019-03864-9 SHORT COMMUNICATION CNS penetration of the CDK4/6 inhibitor ribociclib in non‑tumor bearing mice and mice bearing pediatric brain tumors Yogesh T. Patel1,2 · Abigail Davis1 · Suzanne J. Baker3 · Olivia Campagne1 · Clinton F. Stewart1 Received: 22 January 2019 / Accepted: 3 May 2019 / Published online: 11 May 2019 © Springer-Verlag GmbH Germany, part of Springer Nature 2019 Abstract Purpose Ribociclib, an orally bioavailable small-molecule CDK4/6 inhibitor is currently undergoing evaluation to treat pedi- atric central nervous system (CNS) tumors. However, it is crucial that it penetrates the brain and tumor. Thus, the objectives of the present study were to derive a clinically relevant mouse dosage for cerebral microdialysis studies, and to characterize ribociclib CNS penetration in non-tumor bearing mice and in mice bearing DIPGx7 (glioma) cortical allograft tumors. Methods A plasma pharmacokinetic study of ribociclib (100 mg/kg, orally) was performed in CD1 nude mice bearing glioma cortical allografts to obtain initial plasma pharmacokinetic parameters and to derive D-optimal plasma sampling time-points for microdialysis studies. Using a cerebral microdialysis technique, the extracellular fuid (ECF) disposition of ribociclib was evaluated after a single oral ribociclib dose (100 mg/kg) in non-tumor bearing mice and in mice bearing glioma cortical allografts. A one-compartment plasma model with absorption and ECF compartments were ft to plasma and ECF concentration–time data using a nonlinear mixed efects modeling approach (NONMEM 7.2). Results The mean unbound ribociclib plasma exposure (6812 ng/ml*h) was similar to that observed clinically at recom- mended dosages in adults. -

New Drug Update: the Next Step in Personalized Medicine
New Drug Update: The Next Step in Personalized Medicine Jordan Hill, PharmD, BCOP Clinical Pharmacy Specialist WVU Medicine Mary Babb Randolph Cancer Center Objectives • Review indications for new FDA approved anti- neoplastic medications in 2017 • Outline place in therapy of new medications • Become familiar with mechanisms of action of new medications • Describe adverse effects associated with new medications • Summarize dosing schemes and appropriate dose reductions for new medications First-in-Class Approvals • FLT3 inhibitor – midostaurin • IDH2 inhibitor – enasidenib • Anti-CD22 antibody drug conjugate – inotuzumab ozogamicin • CAR T-cell therapy - tisagenlecleucel “Me-too” Approvals • CDK 4/6 inhibitor – ribociclib and abemaciclib • PD-L1 inhibitors • Avelumab • Durvalumab • PARP inhibitor – niraparib • ALK inhibitor – brigatinib • Pan-HER inhibitor – neratinib • Liposome-encapsulated combination of daunorubicin and cytarabine • PI3K inhibitor – copanlisib Drugs by Malignancy AML Breast Bladder ALL FL Lung Ovarian 0 1 2 3 Oral versus IV 46% 54% Oral IV FIRST-IN CLASS FLT3 Inhibitor - midostaurin Journal of Hematology & Oncology 2017;10:93 Midostaurin (Rydapt®) • 717 newly diagnosed FLT3+ AML Patients • Induction and consolidation chemotherapy and placebo maintenance versus chemotherapy + midostaurin and Treatment maintenance midostaurin • OS: 74.7 mo versus 25.6 mo (P=0.009) Efficacy • EFS: 8.2 mo versus 3.0 mo (P=0.002) • Higher grade > 3 anemia, rash, and nausea Safety N Engl J Med 2017;377:454-64 Midostaurin (Rydapt®) • Approved indications: FLT3+ AML, mast cell leukemia, systemic mastocytosis • AML dose: 50 mg twice daily with food on days 8-21 • Of each induction cycle (+ daunorubicin and cytarabine) • Of each consolidation cycle (+ high dose cytarabine) • ADEs: nausea, myelosuppression, mucositis, increases in LFTs, amylase/lipase, and electrolyte abnormalities • Pharmacokinetics: hepatic metabolism, substrate of CYP 3A4; < 5% excretion in urine RYDAPT (midostaurin) [package insert]. -

A Novel Treatment for Triple-Negative Breast Cancer
Huateng Pharma https://en.huatengsci.com A Novel Treatment For Triple-negative Breast Cancer Triple-negative breast cancer is a cancer that tests negative for estrogen receptors, progesterone receptors, and excess HER2 protein. These results mean the growth of the cancer is not fueled by the hormones estrogen and progesterone, or by the HER2 protein. So, triple-negative breast cancer does not respond to hormonal therapy medicines or medicines that target HER2 protein receptors. This type of breast cancer accounts for 10-20% of all types of breast cancer. It has special biological behavior and clinicopathological characteristics, and the prognosis is worse than other types. For doctors and researchers, there is intense interest in finding new medications that can treat this kind of breast cancer. Photodynamic therapy is a novel method for the treatment of breast cancer. By combining a photosensitizer with a corresponding light source, reactive oxygen species (ROS) are generated to selectively destroy the diseased tissues, so as to kill the cancer cells. But at the same time it will also lead to the formation of hypoxia in tumor tissues and reduce the therapeutic effect. Recently, the team of Professor Jin Hongjun from the Molecular Imaging Center of Sun Yat-sen University No.5 Hospital and the Tumor Center of Sun Yat-sen University No.5 Hospital explored a novel method to improve hypoxia in photodynamic therapy, and Huateng Pharma https://en.huatengsci.com preliminarily found that oxyphotodynamic therapy combined with metformin has the potential to treat triple-negative breast cancer. The research was published in the Annals of Translational Medicine (ATM,IF:3.297). -

Toremifene (Fareston)
Clinical Policy: Toremifene (Fareston) Reference Number: PA.CP.PMN.126 Effective Date: 10.17.18 Last Review Date: 04.17.19 Revision Log Description Toremifene (Fareston®) is an estrogen agonist/antagonist. FDA Approved Indication(s) Fareston is indicated for the treatment of metastatic breast cancer in postmenopausal women with estrogen-receptor positive or unknown tumors. Policy/Criteria Provider must submit documentation (such as office chart notes, lab results or other clinical information) supporting that member has met all approval criteria. It is the policy of health plans affiliated with PA Health & Wellness® that Fareston is medically necessary when the following criteria are met: I. Initial Approval Criteria A. Breast Cancer (must meet all): 1. Diagnosis of recurrent or metastatic breast cancer; 2. Prescribed by or in consultation with an oncologist; 3. Failure of a 1-month trial of tamoxifen at up to maximally indicated doses, unless contraindicated or clinically significant adverse effects are experienced; 4. Failure of a 1-month trial of an aromatase inhibitor (e.g., anastrozole, exemestane, letrozole) at up to maximally indicated doses, unless contraindicated or clinically significant adverse effects are experienced (see Appendix B); 5. Request meets one of the following (a or b): a. Dose does not exceed 60 mg per day (1 tablet/day); b. Dose is supported by practice guidelines or peer-reviewed literature for the relevant off-label use (prescriber must submit supporting evidence). Approval duration: 12 months B. Soft Tissue Sarcoma - Desmoid Tumors (off-label) (must meet all): 1. Diagnosis of desmoid tumor or aggressive fibromatosis; 2. Prescribed by or in consultation with an oncologist; 3. -
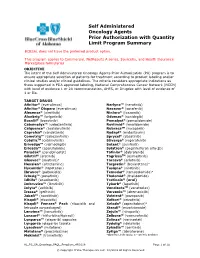
Self Administered Oncology Agents Prior Authorization with Quantity
Self Administered Oncology Agents Prior Authorization with Quantity Limit Program Summary BCBSAL does not have the preferred product option. This program applies to Commercial, NetResults A series, SourceRx, and Health Insurance Marketplace formularies. OBJECTIVE The intent of the Self Administered Oncology Agents Prior Authorization (PA) program is to ensure appropriate selection of patients for treatment according to product labeling and/or clinical studies and/or clinical guidelines. The criteria considers appropriate indications as those supported in FDA approved labeling, National Comprehensive Cancer Network (NCCN) with level of evidence 1 or 2A recommendation, AHFS, or Drugdex with level of evidence of 1 or IIa. TARGET DRUGS Afinitor® (everolimus) Nerlynx™ (neratinib) Afinitor® Disperz (everolimus) Nexavar® (sorafenib) Alecensa® (alectinib) Ninlaro® (ixazomib) Alunbrig™ (brigatinib) Odomzo® (sonidegib) Bosulif® (bosutinib) Pomalyst® (pomalidomide) Cabometyx™ (cabozantinib) Revlimid® (lenalidomide) Calquence® (acalabrutinib) RubracaTM (rucaparib) Caprelsa® (vandetanib) Rydapt® (midostaurin) Cometriq™ (cabozantinib) Sprycel® (dasatinib) CotellicTM (cobimetinib) Stivarga® (regorafenib) Erivedge™ (vismodegib) Sutent® (sunitinib) Erleada™ (apalutamide) Sylatron® (peginterferon alfa-2b) Farydak® (panobinostat) Tafinlar® (dabrafenib) Gilotrif® (afatinib) TagrissoTM (osimertinib) Gleevec® (imatinib)a Tarceva® (erlotinib) Hexalen® (altretamine) Targretin® (bexarotene)a Hycamtin® (topotecan) Tasigna® (nilotinib) Ibrance® (palbociclib) Temodar® -

Ivy Brain Tumor Center and Sonalasense to Test Novel Drug-Device Combination for Glioblastoma
Ivy Brain Tumor Center and SonALAsense to Test Novel Drug-Device Combination for Glioblastoma First-in-human clinical trial will determine effectiveness of promising, non-invasive therapy for brain cancer (PHOENIX, Ariz. – Nov. 21, 2019) – The Ivy Brain Tumor Center at the Barrow Neurological Institute, today announced a strategic collaboration with SonALAsense to develop and test a new, non-invasive drug-device combination, sonodynamic therapy (SDT), for recurrent glioblastoma through a Phase 0/2 clinical trial. Details of the study, as well as the results of two other clinical trials will be announced by Dr. Nader Sanai, director of the Ivy Brain Tumor Center, at the 2019 Society of Neuro-Oncology Annual Meeting (SNO) in Phoenix, Ariz. on Nov. 22. SonALAsense Phase 0/2 Clinical Trial SonALAsense, in conjunction with the Ivy Brain Tumor Center, is collaborating with Insightec®, the innovator of Magnetic Resonance-Guided focused ultrasound (MRFUS) to adapt its technology for use at non-thermal energy levels in combination with SonALAsense’s proprietary formulation of 5-aminolevulinic acid (ALA) for glioblastoma. By adapting the Ivy Center’s Phase 0/2 clinical trial model, SonALAsense’s ALA drug will be administered intravenously, metabolized exclusively by glioblastoma cells, and accumulated as a fluorescent metabolite protoporphyrin IX. This tumor metabolite is then stereotactically activated using Insightec’s MR-guided focused ultrasound which results in reactive oxygen species that are lethal to every tumor cell. This combination of metabolic targeting by ALA and activation by non-invasive focused ultrasound represents an innovative potential new therapeutic modality for glioblastoma patients. This novel technology is called ALA sonodynamic therapy. -

Effects of Toremifene, a Selective Estrogen Receptor Modulator, On
ISSN 2472-1972 Effects of Toremifene, a Selective Estrogen Receptor Modulator, on Spontaneous and Stimulated GH Secretion, IGF-I, and IGF-Binding Proteins in Healthy Elderly Subjects Ferdinand Roelfsema,1 Rebecca J. Yang,2 Paul Y. Takahashi,3 Dana Erickson,4 Cyril Y. Bowers,5 and Johannes D. Veldhuis2 1Department of Internal Medicine, Section of Endocrinology and Metabolism, Leiden University Medical Center, 2333 ZA Leiden, Netherlands; 2Endocrine Research Unit, Mayo School of Graduate Medical Education, Center for Translational Science Activities, Mayo Clinic, Rochester, Minnesota 55905; 3Department of Primary Care Internal Medicine, Mayo Clinic, Rochester, Minnesota 55905; 4Department of Endocrinology, Mayo Clinic, Rochester, Minnesota 55905; and 5Department of Internal Medicine, Tulane University Health Sciences Center, New Orleans, Louisiana 70112 Context: Estrogens amplify spontaneous and stimulated growth hormone (GH) secretion, whereas they diminish GH-dependent insulin-like growth factor (IGF)-I in a dose-dependent manner. Selective es- trogen receptor modulators (SERMs), including tamoxifen and toremifene, are widely adjunctively used in breast and prostate cancer. Although some endocrine effects of tamoxifen are known, few data are available for toremifene. Objective: To explore sex-dependent effects of toremifene on spontaneous 10-hour overnight GH se- cretion, followed by GH-releasing hormone–ghrelin stimulation. Additionally, effects on IGF-I, its binding proteins, and sex hormone–binding globulin (SHBG) were quantified. Participants and Design: Twenty men and 20 women, within an allowableagerangeof50to80years, volunteered for this double-blind, placebo-controlled prospective crossover study. Ten-minute blood sampling was done for 10 hours overnight and then for 2 hours after combined GH-releasing hormone–ghrelin injection. Main Outcome Measures: Pulsatile GH and stimulated GH secretion, and fasting levels of IGF-I, IGF- binding protein (IGFBP)1, IGFBP3, and SHBG.