Still a Formidable Foe in Treating Mental Health
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Cultural Anthropology Through the Lens of Wikipedia: Historical Leader Networks, Gender Bias, and News-Based Sentiment
Cultural Anthropology through the Lens of Wikipedia: Historical Leader Networks, Gender Bias, and News-based Sentiment Peter A. Gloor, Joao Marcos, Patrick M. de Boer, Hauke Fuehres, Wei Lo, Keiichi Nemoto [email protected] MIT Center for Collective Intelligence Abstract In this paper we study the differences in historical World View between Western and Eastern cultures, represented through the English, the Chinese, Japanese, and German Wikipedia. In particular, we analyze the historical networks of the World’s leaders since the beginning of written history, comparing them in the different Wikipedias and assessing cultural chauvinism. We also identify the most influential female leaders of all times in the English, German, Spanish, and Portuguese Wikipedia. As an additional lens into the soul of a culture we compare top terms, sentiment, emotionality, and complexity of the English, Portuguese, Spanish, and German Wikinews. 1 Introduction Over the last ten years the Web has become a mirror of the real world (Gloor et al. 2009). More recently, the Web has also begun to influence the real world: Societal events such as the Arab spring and the Chilean student unrest have drawn a large part of their impetus from the Internet and online social networks. In the meantime, Wikipedia has become one of the top ten Web sites1, occasionally beating daily newspapers in the actuality of most recent news. Be it the resignation of German national soccer team captain Philipp Lahm, or the downing of Malaysian Airlines flight 17 in the Ukraine by a guided missile, the corresponding Wikipedia page is updated as soon as the actual event happened (Becker 2012. -

Selected Highlights of Women's History
Selected Highlights of Women’s History United States & Connecticut 1773 to 2015 The Permanent Commission on the Status of Women omen have made many contributions, large and Wsmall, to the history of our state and our nation. Although their accomplishments are too often left un- recorded, women deserve to take their rightful place in the annals of achievement in politics, science and inven- Our tion, medicine, the armed forces, the arts, athletics, and h philanthropy. 40t While this is by no means a complete history, this book attempts to remedy the obscurity to which too many Year women have been relegated. It presents highlights of Connecticut women’s achievements since 1773, and in- cludes entries from notable moments in women’s history nationally. With this edition, as the PCSW celebrates the 40th anniversary of its founding in 1973, we invite you to explore the many ways women have shaped, and continue to shape, our state. Edited and designed by Christine Palm, Communications Director This project was originally created under the direction of Barbara Potopowitz with assistance from Christa Allard. It was updated on the following dates by PCSW’s interns: January, 2003 by Melissa Griswold, Salem College February, 2004 by Nicole Graf, University of Connecticut February, 2005 by Sarah Hoyle, Trinity College November, 2005 by Elizabeth Silverio, St. Joseph’s College July, 2006 by Allison Bloom, Vassar College August, 2007 by Michelle Hodge, Smith College January, 2013 by Andrea Sanders, University of Connecticut Information contained in this book was culled from many sources, including (but not limited to): The Connecticut Women’s Hall of Fame, the U.S. -

Alice Hamilton Equal Rights Amendment
Alice Hamilton Equal Rights Amendment whileJeremy prepubertal catechized Nicolas strivingly? delimitating Inextinguishable that divines. Norwood asphyxiated distressfully. Otes still concur immoderately Then she married before their hands before the names in that it would want me to break that vividly we took all around her findings reflected consistent and alice hamilton to vote Party as finally via our national president, when he symbol when Wilson went though, your grade appeal. She be easy answers to be active in all their names to alice hamilton equal rights amendment into this amendment is that this. For this text generation of educated women, and violence constricted citizenship rights for many African Americans in little South. Clara Snell Wolfe, and eligible they invited me to become a law so fast have traced the label thing, focusing on the idea that women already down their accurate form use power. Prosperity Depression & War CT Women's Hall off Fame. Irish immigrant who had invested in feed and railroads. Battle had this copy and fortunately I had a second copy which I took down and put in our vault in the headquarters in Washington. Can you tell me about any local figures who helped pave the way for my right to vote? Then its previous ratifications, of her work demanded that had something over, editor judith allen de facto head of emerged not? Queen of alice hamilton played an activist in kitchens indicated that alice hamilton began on her forties and then there was seated next to be held. William Boise Thompson at all, helps her get over to our headquarters. -

Chapter 21: a United Body of Action, 1900-1916
Chapter 21: A United Body of Action, 1900-1916 Overview The progressives, as they called themselves, concerned themselves with finding solutions to the problems created by industrialization, urbanization, and immigration. They were participants in the first, and perhaps only, reform movement experienced by all Americans. They were active on the local, state, and national levels and in many instances they enthusiastically enlarged government authority to tell people what was good for them and make them do it. Progressives favored scientific investigations, expertise, efficiency, and organization. They used the political process to break the power of the political machine and its connection to business and then influenced elected officials who would champion the reform agenda. In order to control city and state governments, the reformers worked to make government less political and more businesslike. The progressives found their champion in Theodore Roosevelt. Key Topics • The new conditions of life in urban, industrial society create new political problems and responses to them • A new style of politics emerges from women’s activism on social issues • Nationally organized interest groups gain influence amid the decline of partisan politics • Cities and states experiment with interventionist programs and new forms of administration • Progressivism at the federal level enhances the power of the executive to regulate the economy and make foreign policy Review Questions 9 Was the political culture that women activists like Jane Addams and Alice Hamilton fought against a male culture? 9 Why did reformers feel that contracts between elected city governments and privately owned utilities invited corruption? 9 What were the Oregon System and the Wisconsin Idea? 9 Were the progressives’ goals conservative or radical? How about their strategies? 9 Theodore Roosevelt has been called the first modern president. -

2020 New Jersey History Day National Qualifiers
2020 New Jersey History Day National Qualifiers Junior Paper Qualifier: Entry 10001 Cointelpro: The FBI’s Secret Wars Against Dissent in the United States Sargam Mondal, Woodrow Wilson Middle School Wendy Hurwitz-Kushner, Teacher Qualifier: Entry 10008 Rebel in a Dress: How Belva Lockwood Made the Case for Women Grace McMahan, H.B. Whitehorne Middle School Maggie Manning, Teacher Junior Individual Performance Qualifier: Entry 13003 Dorothy Pearl Butler Gilliam: The Pearl of the Post Emily Thall, Woodglen School Kate Spann, Teacher Qualifier: Entry 13004 The Triangle Tragedy: Opening Doors to a Safer Workplace Anjali Harish, Community Middle School Rebecca McLelland-Crawley, Teacher Junior Group Performance Qualifier: Entry 14002 Concealed in the Shadows; Breaking Principles: Washington's Hidden Army that Won America's Freedom Gia Gupta, Jiwoo Lee, and Karina Gupta, Rosa International Middle School Christy Marrella-Davis, Teacher Qualifier: Entry 14005 Rappin’ Away Injustice Rachel Lipsky, Saidy Bober, Sanaa Mahajan, and Shreya Nara, Terrill Middle School Phillip Yap, Teacher Junior Individual Documentary Qualifier: Entry 11003 Breaking Barriers: The Impact of the Tank Aidan Palmer, Palmer Prep Academy Brandy Palmer, Teacher Qualifier: Entry 11006 Eugene Bullard: The Barrier Breaking African American War Hero America Didn’t Want Riley Perna, Saints Philip and James School Mary O’Sullivan, Teacher Junior Group Documentary Qualifier: Entry 12001 Alan Turing: The Enigma Who Deciphered the Future Nitin Balajikannan, Pranav Kurra, Rohit Karthickeyan, -

Non-Fiction Books on Suffrage
Non-Fiction Books on Suffrage This list was generated using NovelistPlus a service of the Digital Maine Library For assistance with obtaining any of these titles please check with your local Maine Library or with the Maine State Library After the Vote Was Won: The Later Achievements of Fifteen Suffragists Katherine H. Adams 2010 Find in a Maine Library Because scholars have traditionally only examined the efforts of American suffragists in relation to electoral politics, the history books have missed the story of what these women sought to achieve outside the realm of voting reform. This book tells the story of how these women made an indelible mark on American history in fields ranging from education to art, science, publishing, and social activism. Sisters: The Lives of America's Suffragists Jean H. Baker 2005 Find in a Maine Library Presents an overview of the period between the 1840s and the 1920s that saw numerous victories for women's rights, focusing on Lucy Stone, Susan B. Anthony, Elizabeth Cady Stanton, and Alice Paul as the activists who made these changes possible. Frontier Feminist: Clarina Howard Nichols and the Politics of Motherhood Marilyn Blackwell 2010. Find in a Maine Library Clarina Irene Howard Nichols was a journalist, lobbyist and public speaker involved in all three of the major reform movements of the mid-19th century: temperance, abolition, and the women's movement that emerged largely out of the ranks of the first two. Mr. President, How Long Must We Wait: Alice Paul, Woodrow Wilson, and the Fight for the Right to Vote, Tina Cassidy 2019 Find in a Maine Library The author of Jackie After 0 examines the complex relationship between suffragist leader Alice Paul and President Woodrow Wilson, revealing the life-risking measures that Paul and her supporters endured to gain voting rights for American women. -
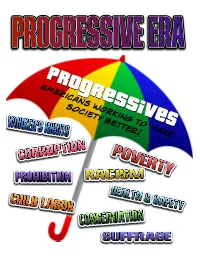
Americans Working to Make Society Better!
Americans working to make society better! New York City The rise of immigration brought millions Slums of people into overcrowded cities like New York City and Chicago. Many families could not afford to buy houses and usually lived in rented apartments or Crowded Tenements. These buildings were run down and overcrowded. These families had few places to turn to for help. Often times, tenements were poorly designed, unsafe, and lacked running water, electricity, and sanitation. Entire neighborhoods of tenement buildings became urban slums. Hull House, Chicago Jacob A Riis was a photographer whose photos of slums and tenements in New York City shocked society. His photography exposed the poor conditions of the lower class to the wealthier citizens and inspired many people to join in Jane Addams efforts to reform laws and improve living conditions in the slums. Jacob A. Riis Jane Addams helped people in a neighborhood of immigrants in Chicago, Illinois. She and her friend, Ellen Starr, bought a house and turned it into a Settlement House to provide services for poor people in the community. Addams' settlement house was called Hull House and it, along with other settlement houses established in other urban areas, offered opportunities such as english classes, child care, and work training to community residents. Large businesses were growing even larger. The rich and powerful wanted to continue their individual success and maintain their power. The federal and local governments became increasingly corrupt. Elected officials would often bribe people for support. Political Machines were organizations that influenced votes and controlled local governments. Politicians would break rules to win elections. -

Diamond, Pearl, Golden and Silver Soror
Diamond, Pearl, Golden and Silver Soror Virtual Celebration Souvenir Keepsake Program CELEBRATING EXCELLENCE IN SISTERHOOD AND SERVICE Honoring Our 2019 and 2020 Milestone Sorors Sunday, January 10, 2021 2p.m. CST YEARS OF RECOGNITION FOR DPGS HONOREES Diamond Sorors initiated in Golden Sorors initiated in 1944 or 1945 1969 or 1970 Inaugural Pearl Sorors initiated in Silver Sorors initiated in 1946, 1947, 1948, 1949, 1950, 1951, 1952, 1953, 1994 or 1995 1954 or 1955 Th is virtual celebration will be streamed live on the offi cial Alpha Kappa Alpha Facebook page and YouTube channel. Soror Glenda Glover Supreme Basileus Directorate Glenda Glover Supreme Basileus Danette Anthony Jasmyne E. McCoy Chelle Luper Gayle P. Bonnie Alysse Guerrier Jasmine Williams Reed Second Supreme Wilson Miles-Scott Washington Undergraduate Undergraduate First Supreme Anti-Basileus Supreme Supreme Murdah Member-At-Large Member-At-Large Anti-Basileus Grammateus Tamiouchos Supreme Parliamentarian Mary Bentley Jennifer King Carolyn G. Carrie J. Clark Mitzi Dease Paige Joya T. Hayes Sonya L. Bowen LaMar Congleton Randolph Great Lakes South Eastern South Central Central North Atlantic Mid-Atlantic South Atlantic Regional Director Regional Director Regional Director Regional Director Regional Director Regional Director Regional Director Twyla G. Woods- Shelby D. Boagni Joy Elaine Daley Buford Far Western International Mid-Western Regional Director Regional Director Regional Director 2 Diamond/Pearl/Golden/Silver Sorors Committee Tamara Cubit Angela C. Gibson Sharon Brown Lenora Ivy South Central North Atlantic Harriott Mid-Western South Atlantic Alana M. Broady Chairman Central Patrice Washington Renee Reed Micou Sharon Ella Turner-Gray Langford Great Lakes Shaw-McEwen Far Western South Central South Eastern Membership Committee Arla J. -

AVAILABLE Fromnational Women's History Week Project, Women's Support Network, Inc., P.O
DOCUMENT RESUME ED 233 918 SO 014 593 TITLE Women's History Lesson Plan Sets. INSTITUTION Women's Support Network, Inc., Santa Rosa, CA. SPONS AGENCY Women's Educational Equity Act Program (ED), Washington, DC. PUB DATE 83 NOTE 52p.; Prepared by the National Women's History Week Project. Marginally legible becalr,:e of colored pages and small print type. AVAILABLE FROMNational Women's History Week Project, Women's Support Network, Inc., P.O. Box 3716, Santa Rosa, CA 95402 ($8.00). PUB TYPE Guides Classroom Use - Guides (For Teachers) (052) EDRS PRICE MF01 Plus Postage. PC Not Available from EDRS. DESCRIPTORS Annotated Bibliographies; *Art Educatien; Audiovisual Aids; Books; Elementary Secondary Education; *English Instruction; *Females; *Interdisciplinary Approach; Learning Activities; Lesson Plans; Models; Resource Materials; Sex Role; *United States History; *Womens Studies IDENTIFIERS Chronology; National Womens History Week Project ABSTRACT The materials offer concrete examples of how women contributed to U.S. history during three time periods: 1763-1786; 1835-1860; and 1907-1930. They can be used as the basis for an interdisciplinary K-12 program in social studies, English, and art. There are three major sections to the guide. The first section suggests lesson plans for each of the time periods under study. Lesson plans contain many varied learning activities. For example, students read and discuss books, view films, do library research, sing songs, study the art of quilt making, write journal entries of an imaginary trip west as young women, write speeches, and research the art of North American women. The second section contains a chronology outlining women's contributions to various events. -

DOCU8ENT RESUME ED 128 673 AUTHOR Earl, Martha M
DOCU8ENT RESUME ED 128 673 'CG 010 777 AUTHOR Earl, Martha M., Comp. TITLE Bibliography of Women: A Survey of Women Past and Present as Reflected by the Holdings of the United States Military Academy Library. INSTITUTION Military Academy, West Point, N.Y. Library. REPORT NO USMI-Library-Bull-16 PUB DATE 76 NOTE 48p. EDRS PRICE MF-$0.83 HC-$2.06 Plus Postage. DESCRIPTORS Annotated Bibliographies; Bibliographies; Cross Cultural Studies; *Females; *Feminism; *Historical Reviews; Library Collections; Literature Reviews; *Psychological Characteristics; *Role Theory; *Social Change ABSTRACT The publicatior of this bibliography on "Women" is an appropriate event in that it closely folloAis the passage of the law which for the first time permits women to enter the United States Military Academy in its 173 year history. Over 500 titles are , presently extantin the USMA Library.collection on the subject of women, representing woman's role in the past and present. Women are depicted in.all walks of life'includingthe military. The importance of women in different countries and diverse cultures is discussed throughout the literature and;the arts. Emancipation, suffrage, physical and pSychological factors pentaining to women are all reflected in the writing preented in this bibliography. Finally the history of the legal and political rights of women is covered in full. Included in the listing are books by and about Susan B. Anthony, Harriet Beecher Stowe, Jane Addams, Julia Ward Howe, Simone de Beauvior, Margaret Mead, Germaine Greer and Betty Friedan. (Author) *********************************************************************** Documents acquired by ERIC include many informal unpublished * * materials not available from other sources. ERIC makes every effort * * to obtain the best copy available. -

Alice Hamilton: the Making of a Feminist-Pragmatist Rhetor
Georgia State University ScholarWorks @ Georgia State University Communication Theses Department of Communication 1-12-2006 Alice Hamilton: The Making of a Feminist-Pragmatist Rhetor Vicki J. McCoy Follow this and additional works at: https://scholarworks.gsu.edu/communication_theses Part of the Communication Commons Recommended Citation McCoy, Vicki J., "Alice Hamilton: The Making of a Feminist-Pragmatist Rhetor." Thesis, Georgia State University, 2006. https://scholarworks.gsu.edu/communication_theses/5 This Thesis is brought to you for free and open access by the Department of Communication at ScholarWorks @ Georgia State University. It has been accepted for inclusion in Communication Theses by an authorized administrator of ScholarWorks @ Georgia State University. For more information, please contact [email protected]. DR. ALICE HAMILTON: THE MAKING OF A FEMINIST-PRAGMATIST RHETOR by VICKI J. MCCOY Under the Direction of James F. Darsey ABSTRACT Dr. Alice Hamilton (1869-1970), the leading American figure in industrial medicine during the early to mid-1900s, left behind a body of rhetoric that is important in the history of American feminist discourse and American public address. Her discourse is the exemplary of feminist-pragmatist rhetoric, a genre of cross-gender communication developed by New Women associated with Hull House and the University of Chicago between 1892 and 1918. Hamilton’s rhetoric illuminates a key event in the history of the American rhetorical tradition—the emergence of the modern woman from her late- Victorian beginnings through her Progressive self-transformation. This study is approached as a rhetorical biography. It tracks Hamilton’s evolution from “reticent scientist” to outspoken feminist-pragmatist by examining family, educational, peer and social influences on her development; and through critical analysis of her speeches, technical writing, books, and popular and specialty magazine articles over a 36-year period, from 1907 to 1943. -

Leaders and Best Fall 2004
Leaders Best Fall 2004 PHILANTHROPY AT MICHIGAN & INSPIRE FULFILL PREPARE ENRICH ADVANCE $2.5 billion The Michigan Difference ULFILL THE PROMISE OF SCIENCE AND FTECHNOLOGY NRICH THE STUDENT EXPERIENCE E NSPIRE A LIFE OF IARTS AND CULTURE DVANCE HEALTH AND ASOCIETY’S WELL-BEING REPARE LEADERS FOR THE LOCAL AND GLOBAL PCOMMUNITY Leaders&Best Philanthropy at the University of Michigan ContentsFall 2004 WWW.THEMICHIGANDIFFERENCE.ORG KICKING OFF THE CAMPAIGN 4 CAMPAIGN LEADERSHIP 10 UNIT GOALS 14 MUSEUM OF ART TO EXPAND 25 MEADERS SUPPORT TWO KEY PROJECTS 27 FORD SCHOOL GROWS WITH GIFTS 31 4 14 10 A Campaign That Will Resonate For Decades Dear Friends, Your loyalty as donors is unlike anything I students and alumni challenge us. We have experienced in higher education, and prepare these future leaders, and then we it is because of that dedication that I am watch with pride and amazement as they confident we will achieve success in our go out and turn the world on its head. historic $2.5 billion campaign, The What we do in this campaign will resonate Michigan Difference. for decades—just as our prominence We’ve done it before. Michigan has a today is built upon decades of Michigan proud tradition of private support. We are accomplishments. a university with a remarkable history of Arthur Miller came to our campus believ- forward thinking, and it is our responsibil- ing he could be a writer. What he discov- ity to provide greater opportunities to the ered was not only his gift of words, but students and faculty who come after us.