The Identification and Characterization of Novel Antibacterial Compounds Via Target-Based and Whole Cell Screening Approaches
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Synthesis and Biological Evaluation of Trisindolyl-Cycloalkanes and Bis- Indolyl Naphthalene Small Molecules As Potent Antibacterial and Antifungal Agents
Synthesis and Biological Evaluation of Trisindolyl-Cycloalkanes and Bis- Indolyl Naphthalene Small Molecules as Potent Antibacterial and Antifungal Agents Dissertation Zur Erlangung des akademischen Grades doctor rerum naturalium (Dr. rer. nat.) Vorgelegt der Naturwissenschaftlichen Fakultät I Institut für Pharmazie Fachbereich für Pharmazeutische Chemie der Martin-Luther-Universität Halle-Wittenberg von Kaveh Yasrebi Geboren am 09.14.1987 in Teheran/Iran (Islamische Republik) Gutachter: 1. Prof. Dr. Andreas Hilgeroth (Martin-Luther-Universität Halle-Wittenberg, Germany) 2. Prof. Dr. Sibel Süzen (Ankara Üniversitesi, Turkey) 3. Prof. Dr. Michael Lalk (Ernst-Moritz-Arndt-Universität Greifswald, Germany) Halle (Saale), den 21. Juli 2020 Selbstständigkeitserklärung Hiermit erkläre ich gemäß § 5 (2) b der Promotionsordnung der Naturwissenschaftlichen Fakultät I – Institut für Pharmazie der Martin-Luther-Universität Halle-Wittenberg, dass ich die vorliegende Arbeit selbstständig und ohne Benutzung anderer als der angegebenen Hilfsmittel und Quellen angefertigt habe. Alle Stellen, die wörtlich oder sinngemäß aus Veröffentlichungen entnommen sind, habe ich als solche kenntlich gemacht. Ich erkläre ferner, dass diese Arbeit in gleicher oder ähnlicher Form bisher keiner anderen Prüfbehörde zur Erlangung des Doktorgrades vorgelegt wurde. Halle (Saale), den 21. Juli 2020 Kaveh Yasrebi Acknowledgement This study was carried out from June 2015 to July 2017 in the Research Group of Drug Development and Analysis led by Prof. Dr. Andreas Hilgeroth at the Institute of Pharmacy, Martin-Luther-Universität Halle-Wittenberg. I would like to thank all the people for their participation who supported my work in this way and helped me obtain good results. First of all, I would like to express my gratitude to Prof. Dr. Andreas Hilgeroth for providing me with opportunity to carry out my Ph.D. -

Antimicrobial Resistance and Disinfectants Susceptibility of Persistent Bacteria in a Tertiary Care Hospital
Journal of Microbiology and Antimicrobials Vol. 2(7), pp. xx-xx, October 2010 Available online http://www.academicjournals.org/JMA ISSN 2141-2308 ©2010 Academic Journals Full Length Research Paper Antimicrobial resistance and disinfectants susceptibility of persistent bacteria in a tertiary care hospital Maria Lucia Morcerf Bouzada1, Vania Lucia Silva1, Felipe Augusto Sa Moreira1, Girlene Alves Silva2 and Claudio Galuppo Diniz1* 1Department of Parasitology, Microbiology and Immunology, Laboratory of Bacterial Physiology and Molecular Genetics, Institute of Biological Sciences, Federal University of Juiz de Fora, Juiz de Fora/MG,36036-900, Brazil. 2Department of Applied Nursing, School of Nursing, Federal University of Juiz de Fora, Juiz de Fora/MG, 36036-900, Brazil. Accepted 22 October, 2010 It is well known that putative pathogenic bacteria are ubiquitous and widely distributed in the hospital environment. This study aimed to detect bacterial persistence in the nosocomial environment (different critical areas of the hospital) after mopping by the cleaning staff. Susceptibility patterns to antimicrobial drugs and disinfectants commonly used in health services were also investigated by disk diffusion and agar dilution tests. Rinse water from mops was processed for isolation of Enterobacteriaceae (GNR), non-fermenting Gram-negative rods (NFGNR), coagulase-negative staphylococci (CNS) and enterococci (ENT). Microorganisms were biochemically characterized and 547 strains were recovered. Only CNS and NFGNR were isolated in all critical areas. Overall 67% of the isolated bacteria were resistant to more than three drugs, being considered as multiresistant. Disinfectants were effective in concentrations ranging from 0.125 to 1%. Hospitals provide reservoirs of multiresistant microorganisms borne by patients and staff, but the hospital environment may be an important repository. -

Second and Third Generation Oral Fluoroquinolones
Therapeutic Class Overview Second and Third Generation Oral Fluoroquinolones Therapeutic Class • Overview/Summary: The second and third generation quinolones are approved to treat a variety of infections, including dermatologic, gastrointestinal, genitourinary, respiratory, as well as several miscellaneous infections.1-10 They are broad-spectrum agents that directly inhibit bacterial deoxyribonucleic acid (DNA) synthesis by blocking the actions of DNA gyrase and topoisomerase IV, which leads to bacterial cell death.11,12 The quinolones are most active against gram-negative bacilli and gram-negative cocci.12 Ciprofloxacin has the most potent activity against gram-negative bacteria. Norfloxacin, ciprofloxacin and ofloxacin have limited activity against streptococci and many anaerobes while levofloxacin and moxifloxacin have greater potency against gram-positive cocci, and moxifloxacin has enhanced activity against anaerobic bacteria.11-12 Gemifloxacin, levofloxacin and moxifloxacin are considered respiratory fluoroquinolones. They possess enhanced activity against Streptococcus pneumoniae while maintaining efficacy against Haemophilus influenzae, Moraxella catarrhalis and atypical pathogens. Resistance to the quinolones is increasing and cross-resistance among the various agents has been documented. Two mechanisms of bacterial resistance have been identified. These include mutations in chromosomal genes (DNA gyrase and/or topoisomerase IV) and altered drug permeability across the bacterial cell membranes.11-12 Clinical Guidelines support -

A TWO-YEAR RETROSPECTIVE ANALYSIS of ADVERSE DRUG REACTIONS with 5PSQ-031 FLUOROQUINOLONE and QUINOLONE ANTIBIOTICS 24Th Congress Of
A TWO-YEAR RETROSPECTIVE ANALYSIS OF ADVERSE DRUG REACTIONS WITH 5PSQ-031 FLUOROQUINOLONE AND QUINOLONE ANTIBIOTICS 24th Congress of V. Borsi1, M. Del Lungo2, L. Giovannetti1, M.G. Lai1, M. Parrilli1 1 Azienda USL Toscana Centro, Pharmacovigilance Centre, Florence, Italy 2 Dept. of Neurosciences, Psychology, Drug Research and Child Health (NEUROFARBA), 27-29 March 2019 Section of Pharmacology and Toxicology , University of Florence, Italy BACKGROUND PURPOSE On 9 February 2017, the Pharmacovigilance Risk Assessment Committee (PRAC) initiated a review1 of disabling To review the adverse drugs and potentially long-lasting side effects reported with systemic and inhaled quinolone and fluoroquinolone reactions (ADRs) of antibiotics at the request of the German medicines authority (BfArM) following reports of long-lasting side effects systemic and inhaled in the national safety database and the published literature. fluoroquinolone and quinolone antibiotics that MATERIAL AND METHODS involved peripheral and central nervous system, Retrospective analysis of ADRs reported in our APVD involving ciprofloxacin, flumequine, levofloxacin, tendons, muscles and joints lomefloxacin, moxifloxacin, norfloxacin, ofloxacin, pefloxacin, prulifloxacin, rufloxacin, cinoxacin, nalidixic acid, reported from our pipemidic given systemically (by mouth or injection). The period considered is September 2016 to September Pharmacovigilance 2018. Department (PVD). RESULTS 22 ADRs were reported in our PVD involving fluoroquinolone and quinolone antibiotics in the period considered and that affected peripheral or central nervous system, tendons, muscles and joints. The mean patient age was 67,3 years (range: 17-92 years). 63,7% of the ADRs reported were serious, of which 22,7% caused hospitalization and 4,5% caused persistent/severe disability. 81,8% of the ADRs were reported by a healthcare professional (physician, pharmacist or other) and 18,2% by patient or a non-healthcare professional. -

Identification of Genes Involved in Acid Tolerance, Antimicrobial Resistance and Virulence of Enterococcus Faecium
Identification of genes involved in acid tolerance, antimicrobial resistance and virulence of Enterococcus faecium Thesis submitted by Hashimatul Fatma binti Hashim For the degree of DOCTOR OF PHILOSOPHY in the Faculty of Medical Sciences University College London Division of Microbial Diseases UCL Eastman Dental Institute 256 Gray’s Inn Road London WC1X 8LD UK 2016 Declaration I hereby certify that the work embodied in this thesis is the result of my own investigation, except where otherwise stated. 2 Abstract Enterococcus faecium is an opportunistic human nosocomial pathogen that has developed resistance to many existing antimicrobial therapies. Treatment of enterococcal infections is becoming increasingly challenging and there are limited therapeutic options against multidrug-resistant enterococci. The work described in this thesis aimed to identify genes involved in resistance to host stresses and virulence as these could potentially be future therapeutic targets. An E. faecium transposon mutant library was screened for altered resistance to lysozyme and to nisin as a model antimicrobial peptide. This approach led to the identification of several genes that contribute to lysozyme and nisin resistance. A number of mutants that were sensitive to nisin had a transposon insertion in a gene predicted to encode a tyrosine decarboxylase. It was shown that the tyrosine decarboxylase plays a role in acid tolerance and mediates virulence of E. faecium in a Galleria mellonella larvae infection model. A targeted genetic approach was used to examine the role of an E. faecium serine threonine protein kinase (Stk1) in antimicrobials resistance, host cell stresses and virulence. Disruption of the stk1 gene led to higher sensitivity to antibiotics that target the penicillin- binding proteins and bile salts compared to the wild type. -
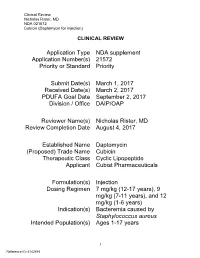
Clinical Review Nicholas Rister, MD NDA 021572 Cubicin (Daptomycin for Injection)
Clinical Review Nicholas Rister, MD NDA 021572 Cubicin (Daptomycin for injection) CLINICAL REVIEW Application Type NDA supplement Application Number(s) 21572 Priority or Standard Priority Submit Date(s) March 1, 2017 Received Date(s) March 2, 2017 PDUFA Goal Date September 2, 2017 Division / Office DAIP/OAP Reviewer Name(s) Nicholas Rister, MD Review Completion Date August 4, 2017 Established Name Daptomycin (Proposed) Trade Name Cubicin Therapeutic Class Cyclic Lipopeptide Applicant Cubist Pharmaceuticals Formulation(s) Injection Dosing Regimen 7 mg/kg (12-17 years), 9 mg/kg (7-11 years), and 12 mg/kg (1-6 years) Indication(s) Bacteremia caused by Staphylococcus aureus Intended Population(s) Ages 1-17 years 1 Reference ID: 4142515 Clinical Review Nicholas Rister, MD NDA 021572 Cubicin (Daptomycin for injection) Table of Contents 1 RECOMMENDATIONS/RISK BENEFIT ASSESSMENT ......................................... 7 1.1 Recommendation on Regulatory Action ............................................................. 7 1.2 Risk Benefit Assessment .................................................................................... 7 1.3 Recommendations for Postmarket Risk Evaluation and Mitigation Strategies ... 8 1.4 Recommendations for Postmarket Requirements and Commitments ................ 8 2 INTRODUCTION AND REGULATORY BACKGROUND ........................................ 8 2.1 Product Information ............................................................................................ 8 2.2 Tables of Currently Available Treatments -

Fluoroquinolones in Children: a Review of Current Literature and Directions for Future Research
Academic Year 2015 - 2016 Fluoroquinolones in children: a review of current literature and directions for future research Laurens GOEMÉ Promotor: Prof. Dr. Johan Vande Walle Co-promotor: Dr. Kevin Meesters, Dr. Pauline De Bruyne Dissertation presented in the 2nd Master year in the programme of Master of Medicine in Medicine 1 Deze pagina is niet beschikbaar omdat ze persoonsgegevens bevat. Universiteitsbibliotheek Gent, 2021. This page is not available because it contains personal information. Ghent Universit , Librar , 2021. Table of contents Title page Permission for loan Introduction Page 4-6 Methodology Page 6-7 Results Page 7-20 1. Evaluation of found articles Page 7-12 2. Fluoroquinolone characteristics in children Page 12-20 Discussion Page 20-23 Conclusion Page 23-24 Future perspectives Page 24-25 References Page 26-27 3 1. Introduction Fluoroquinolones (FQ) are a class of antibiotics, derived from modification of quinolones, that are highly active against both Gram-positive and Gram-negative bacteria. In 1964,naladixic acid was approved by the US Food and Drug Administration (FDA) as first quinolone (1). Chemical modifications of naladixic acid resulted in the first generation of FQ. The antimicrobial spectrum of FQ is broader when compared to quinolones and the tissue penetration of FQ is significantly deeper (1). The main FQ agents are summed up in table 1. FQ owe its antimicrobial effect to inhibition of the enzymes bacterial gyrase and topoisomerase IV which have essential and distinct roles in DNA replication. The antimicrobial spectrum of FQ include Enterobacteriacae, Haemophilus spp., Moraxella catarrhalis, Neiserria spp. and Pseudomonas aeruginosa (1). And FQ usually have a weak activity against methicillin-resistant Staphylococcus aureus (MRSA). -

Quinupristin/Dalfopristin
Reprinted from www.antimicrobe.org Quinupristin/Dalfopristin Antibiotic Class: Streptogramin Antimicrobial Activity: Gram-positive bacteria. In-vitro data suggests streptogramins possess activity against gram-negative upper respiratory tract pathogens and gram-negative anaerobes. Mechanism of Action: Inhibition of mRNA translation by binding to the 50S subunit of bacterial ribosomes. Pharmacodynamics: Predominantly independent of concentration once above four times the MIC of common Staphylococci and Streptococci. Pharmacokinetics: (7.5mg/kg dose at steady state) Cmax: 3.2 and 7.96mg/L (quinupristin and dalfopristin respectively) Half-life: 3.07 and 1.04 hours (quinupristin and dalfopristin respectively) Volume of distribution: 0.45 and 0.24L/kg (quinupristin and dalfopristin respectively) Adverse Effects: Venous irritation due to quinupristin/dalfopristin is common. In comparative trials approximately 40% of patients experienced infusion site adverse reactions compared to 25% of comparator treated patients. Increasing the infusion volume or administering the drug via central line may attenuate this reaction. In two compassionate use studies, arthralgias (9.1%) and myalgias (6.6%) were the most common adverse event related to quinupristin/dalfopristin. Hyperbilirubinemia was documented in up to 25% of quinupristin/dalfopristin treated patients in compassionate use/non-comparative studies. Dosage: Intravenous only – available as 500mg (150mg quinupristin and 350mg dalfopristin) and 600mg (180mg quinupristin and 420mg dalfopristin) powder for reconstitution vials Serious or life-threatening infections associated with vancomycin-resistant Enterococcus faecium – 7.5mg/kg every 8 hours Complicated skin and skin structure infection caused by methicillin-susceptible S. aureus or S. pyogenes – 7.5mg/kg every 12 hours Disease state based dosing: Hepatic failure: Although no dosage official dosage adjustment recommendations exist, pharmacokinetic data in patients with hepatic cirrhosis (Childs-Pugh class A or B) suggest that dosage adjustments may be necessary. -

Nitrofurantoin Administration for the Prevention of Short-Term Catheter
Study Title: Nitrofurantoin Administration for the Prevention of Short-Term Catheter Associated Urinary Tract Infection After Pelvic Surgery (NAUTICA): A Randomized Controlled Trial ClinicalTrials.gov ID: NCT03287089 Date: July 6, 2018 STUDY OBJECTIVES Primary Objective To evaluate the efficacy of administration of nitrofurantoin prophylaxis after catheter discontinuation for the prevention of catheter-associated urinary tract infections in patients with postoperative short-term catheterization following pelvic reconstructive surgery. The primary outcome will be the treatment of clinically suspected and/or culture-proven UTI within 30 days of surgery. Secondary Objectives 1. To evaluate adverse outcomes related to study medications in each group 2. To evaluate medication compliance BACKGROUND Urinary tract infections (UTI) are the most common hospital-acquired infections, accounting for nearly 30% of cases of nosocomial infections and affecting nearly 1 million people per year.1-3 They account for nearly 8.1 million visits to health care providers and cost an estimated $1.6 billion a year in the United States alone.3,4 Following pelvic reconstructive and urinary incontinence surgery, UTIs are one of the most common complications.4,5 The baseline risk of UTI associated with pelvic floor surgery ranges between 5-35%, increasing greatly with catheterization.3 In women who are undergoing surgery for urinary incontinence, the risk of UTI ranges between 8.9% to 34%.4,6,7 Risk factors for urinary tract infections in women undergoing pelvic floor -

Bacterial Prostatitis
REVIEW CURRENT OPINION Bacterial prostatitis Bradley C. Gill a,b and Daniel A. Shoskesa,b Purpose of review The review provides the infectious disease community with a urologic perspective on bacterial prostatitis. Specifically, the article briefly reviews the categorization of prostatitis by type and provides a distillation of new findings published on bacterial prostatitis over the past year. It also highlights key points from the established literature. Recent findings Cross-sectional prostate imaging is becoming more common and may lead to more incidental diagnoses of acute bacterial prostatitis. As drug resistance remains problematic in this condition, the reemergence of older antibiotics such as fosfomycin, has proven beneficial. With regard to chronic bacterial prostatitis, no clear clinical risk factors emerged in a large epidemiological study. However, bacterial biofilm formation has been associated with more severe cases. Surgery has a limited role in bacterial prostatitis and should be reserved for draining of a prostatic abscess or the removal of infected prostatic stones. Summary Prostatitis remains a common and bothersome clinical condition. Antibiotic therapy remains the basis of treatment for both acute and chronic bacterial prostatitis. Further research into improving prostatitis treatment is indicated. Keywords acute bacterial prostatitis, bacterial prostatitis, category I prostatitis, category II prostatitis, chronic bacterial prostatitis, male pelvic pain INTRODUCTION and August 2015 were identified among the first Prostatitis is a bothersome condition but carries 600 search results. The titles of English language potential for serious morbidity from sepsis, abscess, articles were examined and those pertaining to non- or fistula if insufficiently managed. Nearly one in six bacterial prostatitis, chronic pelvic pain, and animal men report a history of prostatitis, resulting in over or basic science models were excluded. -

Computational Antibiotics Book
Andrew V DeLong, Jared C Harris, Brittany S Larcart, Chandler B Massey, Chelsie D Northcutt, Somuayiro N Nwokike, Oscar A Otieno, Harsh M Patel, Mehulkumar P Patel, Pratik Pravin Patel, Eugene I Rowell, Brandon M Rush, Marc-Edwin G Saint-Louis, Amy M Vardeman, Felicia N Woods, Giso Abadi, Thomas J. Manning Computational Antibiotics Valdosta State University is located in South Georgia. Computational Antibiotics Index • Computational Details and Website Access (p. 8) • Acknowledgements (p. 9) • Dedications (p. 11) • Antibiotic Historical Introduction (p. 13) Introduction to Antibiotic groups • Penicillin’s (p. 21) • Carbapenems (p. 22) • Oxazolidines (p. 23) • Rifamycin (p. 24) • Lincosamides (p. 25) • Quinolones (p. 26) • Polypeptides antibiotics (p. 27) • Glycopeptide Antibiotics (p. 28) • Sulfonamides (p. 29) • Lipoglycopeptides (p. 30) • First Generation Cephalosporins (p. 31) • Cephalosporin Third Generation (p. 32) • Fourth-Generation Cephalosporins (p. 33) • Fifth Generation Cephalosporin’s (p. 34) • Tetracycline antibiotics (p. 35) Computational Antibiotics Antibiotics Covered (in alphabetical order) Amikacin (p. 36) Cefempidone (p. 98) Ceftizoxime (p. 159) Amoxicillin (p. 38) Cefepime (p. 100) Ceftobiprole (p. 161) Ampicillin (p. 40) Cefetamet (p. 102) Ceftoxide (p. 163) Arsphenamine (p. 42) Cefetrizole (p. 104) Ceftriaxone (p. 165) Azithromycin (p.44) Cefivitril (p. 106) Cefuracetime (p. 167) Aziocillin (p. 46) Cefixime (p. 108) Cefuroxime (p. 169) Aztreonam (p.48) Cefmatilen ( p. 110) Cefuzonam (p. 171) Bacampicillin (p. 50) Cefmetazole (p. 112) Cefalexin (p. 173) Bacitracin (p. 52) Cefodizime (p. 114) Chloramphenicol (p.175) Balofloxacin (p. 54) Cefonicid (p. 116) Cilastatin (p. 177) Carbenicillin (p. 56) Cefoperazone (p. 118) Ciprofloxacin (p. 179) Cefacetrile (p. 58) Cefoselis (p. 120) Clarithromycin (p. 181) Cefaclor (p. -

A Study on the Efficacy and Corneal Penetration of Besifloxacin in Routine Cataract Surgery Cases
A STUDY ON THE EFFICACY AND CORNEAL PENETRATION OF BESIFLOXACIN IN ROUTINE CATARACT SURGERY CASES Thesis submitted to THE TAMILNADU Dr.M.G.R. MEDICAL UNIVERSITY Chennai - 600 032. In partial fulfillment of the requirements For the award of the degree of MASTER OF PHARMACY in PHARMACY PRACTICE Submitted by Reg. No.: 261640151 DEPARTMENT OF PHARMACY PRACTICE PERIYAR COLLEGE OF PHARMACEUTICAL SCIENCES TIRUCHIRAPPALLI – 620 021. An ISO 9001:2015 Certified Institution SEPTEMBER – 2018 Dr. A. M. ISMAIL, M.Pharm., Ph.D., Professor Emeritus Periyar College of Pharmaceutical Sciences Tiruchirappalli – 620 021. CERTIFICATE This is to certify that the thesis entitled “A STUDY ON THE EFFICACY AND CORNEAL PENETRATION OF BESIFLOXACIN IN ROUTINE CATARACT SURGERY CASES” submitted by B. NIVETHA, B. Pharm., during September 2018 for the award of the degree of “MASTER OF PHARMACY in PHARMACY PRACTICE” under the Tamilnadu Dr.M.G.R. Medical University, Chennai is a bonafide record of research work done in the Department of Pharmacy Practice, Periyar College of Pharmaceutical Sciences and at Vasan Eye Care Hospital, Tiruchirappalli under my guidance and direct supervision during the academic year 2017-18. Place: Tiruchirappalli – 21. Date: 10th Sep 2018 (Dr. A. M. ISMAIL) Dr. R. SENTHAMARAI, M.Pharm., Ph.D., Principal Periyar College of Pharmaceutical sciences Tiruchirappalli – 620 021. CERTIFICATE This is to certify that the thesis entitled “A STUDY ON THE EFFICACY AND CORNEAL PENETRATION OF BESIFLOXACIN IN ROUTINE CATARACT SURGERY CASES” submitted by B. NIVETHA, B. Pharm., during September 2018 for the award of the degree of “MASTER OF PHARMACY in PHARMACY PRACTICE” under the Tamilnadu Dr.M.G.R.