Antibiotic Resistance in the Microbial World
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Antibiotic Assay Medium No. 3 (Assay Broth) Is Used for Microbiological Assay of Antibiotics. M042
HiMedia Laboratories Technical Data Antibiotic Assay Medium No. 3 (Assay Broth) is used for M042 microbiological assay of antibiotics. Antibiotic Assay Medium No. 3 (Assay Broth) is used for microbiological assay of antibiotics. Composition** Ingredients Gms / Litre Peptic digest of animal tissue (Peptone) 5.000 Beef extract 1.500 Yeast extract 1.500 Dextrose 1.000 Sodium chloride 3.500 Dipotassium phosphate 3.680 Potassium dihydrogen phosphate 1.320 Final pH ( at 25°C) 7.0±0.2 **Formula adjusted, standardized to suit performance parameters Directions Suspend 17.5 grams in 1000 ml distilled water. Heat if necessary to dissolve the medium completely. Sterilize by autoclaving at 15 lbs pressure (121°C) for 15 minutes. Advice:Recommended for the Microbiological assay of Amikacin, Bacitracin, Capreomycin, Chlortetracycline,Chloramphenicol,Cycloserine,Demeclocycline,Dihydrostreptomycin, Doxycycline, Gentamicin, Gramicidin, Kanamycin, Methacycline, Neomycin, Novobiocin, Oxytetracycline, Rolitetracycline, Streptomycin, Tetracycline, Tobramycin, Trolendomycin and Tylosin according to official methods . Principle And Interpretation Antibiotic Assay Medium is used in the performance of antibiotic assays. Grove and Randall have elucidated those antibiotic assays and media in their comprehensive treatise on antibiotic assays (1). Antibiotic Assay Medium No. 3 (Assay Broth) is used in the microbiological assay of different antibiotics in pharmaceutical and food products by the turbidimetric method. Ripperre et al reported that turbidimetric methods for determining the potency of antibiotics are inherently more accurate and more precise than agar diffusion procedures (2). Turbidimetric antibiotic assay is based on the change or inhibition of growth of a test microorganims in a liquid medium containing a uniform concentration of an antibiotic. After incubation of the test organism in the working dilutions of the antibiotics, the amount of growth is determined by measuring the light transmittance using spectrophotometer. -

Neomycin and Polymyxin B Sulfates and Gramicidin
NEOMYCIN AND POLYMYXIN B SULFATES AND GRAMICIDIN- neomycin sulfate, polymyxin b sulfate and gramicidin solution/ drops A-S Medication Solutions ---------- Neomycin and Polymyxin B Sulfates and Gramicidin Ophthalmic Solution, USP (Sterile) Rx only DESCRIPTION: Neomycin and Polymyxin B Sulfates and Gramicidin Ophthalmic Solution, USP is a sterile antimicrobial solution for ophthalmic use. Each mL contains: ACTIVES: Neomycin Sulfate, (equivalent to 1.75 mg neomycin base), Polymyxin B Sulfate equal to 10,000 Polymyxin B units, Gramicidin, 0.025 mg; INACTIVES: Sodium Chloride, Alcohol (0.5%), Poloxamer 188, Propylene Glycol, Purified Water. Hydrochloric Acid and/ or Ammonium Hydroxide may be added to adjust pH (4.7-6.0). PRESERVATIVE ADDED: Thimerosal 0.001%. Neomycin Sulfate is the sulfate salt of neomycin B and C, which are produced by the growth of Streptomyces fradiae Waksman (Fam. Streptomycetaceae). It has a potency equivalent of not less than 600 micrograms of neomycin base per milligram, calculated on an anhydrous basis. The structural formulae are: Polymyxin B Sulfate is the sulfate salt of polymyxin B1 and B2 which are produced by the growth of Bacillus polymyxa (Prazmowski) Migula (Fam. Bacillaceae). It has a potency of not less than 6,000 polymyxin B units per milligram, calculated on an anhydrous basis. The structural formulae are: Gramicidin (also called gramicidin D) is a mixture of three pairs of antibacterial substances (Gramicidin A, B and C) produced by the growth of Bacillus brevis Dubos (Fam. Bacillaceae). It has a potency of not less than 900 mcg of standard gramicidin per mg. The structural formulae are: CLINICAL PHARMACOLOGY: A wide range of antibacterial action is provided by the overlapping spectra of neomycin, polymyxin B sulfate, and gramicidin. -

Biological Function of Gramicidin: Studies on Gramicidin-Negative Mutants (Peptide Antibiotics/Sporulation/Dipicolinic Acid/Bacillus Brevis) PRANAB K
Proc. NatS. Acad. Sci. USA Vol. 74, No. 2, pp. 780-784, February 1977 Microbiology Biological function of gramicidin: Studies on gramicidin-negative mutants (peptide antibiotics/sporulation/dipicolinic acid/Bacillus brevis) PRANAB K. MUKHERJEE AND HENRY PAULUS Department of Metabolic Regulation, Boston Biomedical Research Institute, Boston, Massachusetts 02114; and Department of Biological Chemistry, Harvard Medical School, Boston, Massachusetts 02115 Communicated by Bernard D. Davis, October 28,1976 ABSTRACT By the use of a rapid radioautographic EXPERIMENTAL PROCEDURE screening rocedure, two mutants of Bacillus brevis ATCC 8185 that have lost the ability to produce gramicidin have been iso- lated. These mutants produced normal levels of tyrocidine and Bacterial Strains. Bacillus brevis ATCC 8185, the Dubos sporulated at the same frequency as the parent strain. Their strain, was obtained from the American Type Culture Collec- spores, however, were more heat-sensitive and had a reduced tion. Strain S14 is a streptomycin-resistant derivative of B. brevis 4ipicolinic acid content. Gramicidin-producing revertants oc- ATCC 8185, isolated on a streptomycin-gradient plate without curred at a relatively high frequency among tie survivors of mutagenesis. It grows well at 0.5 mg/ml of streptomycin, but prolonged heat treatment and had also regained the ability to produce heat-resistant spores. A normal spore phenotype could growth is retarded by streptomycin at 1.0 mg/ml. Strain B81 also be restored by the addition of gramicidin to cultures of the is a rifampicin-resistant derivative of strain S14, isolated on mutant strain at the end of exponential growth. On the other rifampicin-gradient plates after mutagenesis of spores with hand, the addition of dipicolinic acid could not cure the spore ethyl methanesulfonate (11). -

Topical Antibiotics for Impetigo: a Review of the Clinical Effectiveness and Guidelines
CADTH RAPID RESPONSE REPORT: SUMMARY WITH CRITICAL APPRAISAL Topical Antibiotics for Impetigo: A Review of the Clinical Effectiveness and Guidelines Service Line: Rapid Response Service Version: 1.0 Publication Date: February 21, 2017 Report Length: 23 Pages Authors: Rob Edge, Charlene Argáez Cite As: Topical antibiotics for impetigo: a review of the clinical effectiveness and guidelines. Ottawa: CADTH; 2017 Feb. (CADTH rapid response report: summary with critical appraisal). ISSN: 1922-8147 (online) Disclaimer: The information in this document is intended to help Canadian health care decision-makers, health care professionals, health systems leaders, and policy-makers make well-informed decisions and thereby improve the quality of health care services. While patients and others may access this document, the document is made available for informational purposes only and no representations or warranties are made with respect to its fitness for any particular purpose. The information in this document should not be used as a substitute for professional medical advice or as a substitute for the application of clinical judgment in respect of the care of a particular patient or other professional judgment in any decision-making process. The Canadian Agency for Drugs and Technologies in Health (CADTH) does not endorse any information, drugs, therapies, treatments, products, processes, or services. While care has been taken to ensure that the information prepared by CADTH in this document is accurate, complete, and up-to-date as at the applicable date the material was first published by CADTH, CADTH does not make any guarantees to that effect. CADTH does not guarantee and is not responsible for the quality, currency, propriety, accuracy, or reasonableness of any statements, information, or conclusions contained in any third-party materials used in preparing this document. -

Milestones and Personalities in Science and Technology
History of Science Stories and anecdotes about famous – and not-so-famous – milestones and personalities in science and technology BUILDING BETTER SCIENCE AGILENT AND YOU For teaching purpose only December 19, 2016 © Agilent Technologies, Inc. 2016 1 Agilent Technologies is committed to the educational community and is willing to provide access to company-owned material contained herein. This slide set is created by Agilent Technologies. The usage of the slides is limited to teaching purpose only. These materials and the information contained herein are accepted “as is” and Agilent makes no representations or warranties of any kind with respect to the materials and disclaims any responsibility for them as may be used or reproduced by you. Agilent will not be liable for any damages resulting from or in connection with your use, copying or disclosure of the materials contained herein. You agree to indemnify and hold Agilent harmless for any claims incurred by Agilent as a result of your use or reproduction of these materials. In case pictures, sketches or drawings should be used for any other purpose please contact Agilent Technologies a priori. For teaching purpose only December 19, 2016 © Agilent Technologies, Inc. 2016 2 Table of Contents The Father of Modern Chemistry The Man Who Discovered Vitamin C Tags: Antoine-Laurent de Lavoisier, chemical nomenclature Tags: Albert Szent-Györgyi, L-ascorbic acid He Discovered an Entire Area of the Periodic Table The Discovery of Insulin Tags: Sir William Ramsay, noble gas Tags: Frederick Banting, -
Identification Product Identifier Product Name Neomycin Sulfate
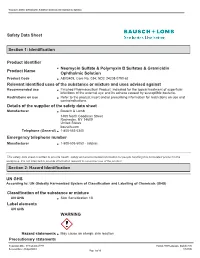
Neomycin Sulfate & Polymyxin B Sulfates & Gramicidin Ophthalmic Solution Safety Data Sheet Section 1: Identification Product identifier Neomycin Sulfate & Polymyxin B Sulfates & Gramicidin Product Name Ophthalmic Solution Product Code AB03409; Core No. 034; NDC 24208-0790-62 Relevant identified uses of the substance or mixture and uses advised against Recommended use Finished Pharmaceutical Product; Indicated for the topical treatment of superficial infections of the external eye and its adnexa caused by susceptible bacteria. Restrictions on use Refer to the product insert and/or prescribing information for restrictions on use and contraindications. Details of the supplier of the safety data sheet Manufacturer Bausch & Lomb 1400 North Goodman Street Rochester, NY 14609 United States bausch.com Telephone (General) 1-800-553-5340 Emergency telephone number Manufacturer 1-800-535-5053 - Infotrac This safety data sheet is written to provide health, safety and environmental information for people handling this formulated product in the workplace. It is not intended to provide information relevant to consumer use of the product. Section 2: Hazard Identification UN GHS According to: UN Globally Harmonized System of Classification and Labelling of Chemicals (GHS) Classification of the substance or mixture UN GHS Skin Sensitization 1B Label elements UN GHS WARNING Hazard statements May cause an allergic skin reaction Precautionary statements Preparation Date: 07/September/1994 Format: GHS Language: English (US) Revision Date: 24/April/2015 UN GHS Page 1 of 10 Neomycin Sulfate & Polymyxin B Sulfates & Gramicidin Ophthalmic Solution Prevention Wash thoroughly after handling. Response IF ON SKIN: Wash with plenty of soap and water. If skin irritation or rash occurs: Get medical advice/attention. -

Antibiotics & Common Infections ABX-2
- - Summaries: Trial SSTI Related toxicity rare - Evidence/Safety, Q&As/Extras: Nitrofurantion documents/GeriRxFiles-UTI.pdf http://www.rxfiles.ca/rxfiles/uploads/ Adults: UTIinOlder Geri-RxFiles RxFILES EXTRAS FROM lookup/59/2/e10 https://academic.oup.com/cid/article- Infections Tissue Skin &Soft IDSA2014: U.S. TISSUEINFECTIONS SKIN &SOFT assets/files/guidelines/en/1121.pdf https://www.cua.org/themes/web/ UTI Recurrent 2011: CUA 2163(16)34717-X/pdf http://www.jogc.com/article/S1701- UTI Recurrent SOGC 2010: 19April2013.pdf photos/custom/UTI%20Guidelines%20 https://saskpic.ipac-canada.org/ Settings Care UTI inContinuing 2013: SK MOH lookup/52/5/e103 https://academic.oup.com/cid/article- (UTI) Pylonephritis Cystitisand Acute Uncomplicated IDSA2010: U.S. CYSTITIS / UTI http://www.mumshealth.com MUMS Guidelines: http://www.bugsanddrugs.ca/ &Drugs: Bugs CANADIAN LINKS ABX-2 RELATED Skin Abscess: I&D +/- ABX I&D +/-ABX Skin Abscess: Clindamycin vs TMP/SMX vsTMP/SMX Clindamycin GUIDELINES/REFERENCES GUIDELINES/REFERENCES - Antibiotics & Common Infections &CommonInfections Antibiotics Stewardship, Effectiveness, Safety & Clinical Pearls-April2017 & Stewardship, Effectiveness,Safety ( Susceptibility of of Susceptibility 1) CYSTISIS UNCOMPLICATED CAUGHTOUREYE... FROMINSIDE THAT ABX-2: AFEWPEARLS Pad”. “Viral Prescription at allavailable These are friendly postersandthepatient suchasthe“GoneViral?”office/clinic extra supporttools on discussions inSaskatchewan. withproviders discussions detailing our springacademic Our tissue(SSTI)infections. and skin&soft willsupport The newchartsinthisnewsletter cystitis uncomplicated of onthetreatment topic tobringouttheABX-2 excited are We ONABX RxFILES ACADEMIC DETAILING pg9) (see Know youroptions! anaphylaxis). (e.g. allergy mediated atrueIgE will have ___ only “allergy”, penicillin 7) ALLERGY LACTAM BETA cellulitis. of treatment successful inthe essential -often 5) verywell. -
![Subpart J—Certain Other Dosage Forms [Reserved] PART](https://docslib.b-cdn.net/cover/6583/subpart-j-certain-other-dosage-forms-reserved-part-1016583.webp)
Subpart J—Certain Other Dosage Forms [Reserved] PART
Pt. 448 21 CFR Ch. I (4±1±96 Edition) (ii) Samples required: Subpart HÐRectal Dosage Forms (a) The oxytetracycline hydro- [Reserved] chloride used in making the batch: 10 packages, each containing approxi- mately 300 milligrams. Subpart IÐ[Reserved] (b) The polymyxin B sulfate used in making the batch: 10 packages, each Subpart JÐCertain Other Dosage containing approximately 300 milli- Forms [Reserved] grams. (c) The batch: A minimum of 30 tab- PART 448ÐPEPTIDE ANTIBIOTIC lets. DRUGS (b) Tests and methods of assayÐ(1) Po- tencyÐ(i) Oxytetracycline content. Pro- Subpart AÐBulk Drugs ceed as directed in § 436.106 of this chap- ter, preparing the sample for assay as Sec. 448.10 Bacitracin. follows: Place a representative number 448.10a Sterile bacitracin. of tablets into a high-speed glass blend- 448.13 Bacitracin zinc. er jar containing sufficient 0.1N hydro- 448.13a Sterile bacitracin zinc. chloric acid to obtain a stock solution 448.15a Sterile capreomycin sulfate. of convenient concentration containing 448.20a Sterile colistimethate sodium. not less than 150 micrograms of oxytet- 448.21 Colistin sulfate. racycline per milliliter (estimated). 448.23 Cyclosporine. Blend for 3 to 5 minutes. Remove an al- 448.25 Gramicidin. iquot of the stock solution and further 448.30 Polymyxin B sulfate. dilute with sterile distilled water to 448.30a Sterile polymyxin B sulfate. the reference concentration of 0.24 448.75 Tyrothricin. microgram of oxytetracycline per mil- liliter (estimated). Subpart BÐOral Dosage Forms (ii) Polymyxin B content. Proceed as 448.121 Colistin sulfate for oral suspension. directed in § 436.105 of this chapter, pre- 448.123 Cyclosporine oral dosage forms. -

Design and Syntheses of Gramicidin S Analogs, Cyclo(-X-Leu-XD
The Journal of Antibiotics (2011) 64, 583–585 & 2011 Japan Antibiotics Research Association All rights reserved 0021-8820/11 $32.00 www.nature.com/ja NOTE Design and syntheses of gramicidin S analogs, cyclo(-X-Leu-X-D-Phe-Pro-)2 (X¼His, Lys, Orn, Dab and Dap) Makoto Tamaki1, Kenta Fujinuma1, Takuji Harada1, Kazumasa Takanashi1, Mitsuno Shindo2, Masahiro Kimura2 and Yoshiki Uchida2 The Journal of Antibiotics (2011) 64, 583–585; doi:10.1038/ja.2011.43; published online 25 May 2011 Keywords: gramicidin S; polycationic analog; structure-activity relationship; synthesis 1,1¢ 2,2¢ 3,3¢ 4,4¢ 5,5¢ 1–3 Gramicidin S (GS), cyclo(-Val -Orn -Leu -D-Phe -Pro -)2, solid phase peptide synthesis on oxime resin (loading of oxime group: is a potent cyclopeptide antibiotic isolated from Bacillus brevis.Its 0.35 mmol gÀ1 resins) (Scheme 1).8 Yresidue(Y¼His(3-Bom), Lys(Z), secondary structure has been established as an antiparallel b-sheet Orn(Z), Dab(Z) and Dap(Z)) as a C-terminal amino acid residue was conformation with amphiphilicity.4,5 The conformation is charac- used based on the propensity of the biosynthetic precursor of GS teristically featured with the orientation of side chains in such a way to form a conformation highly favorable for head–tail cyclization.2,3 that the charged Orn side chains are situated on one side of the The cyclization-cleavage of H-D-Phe-Pro-Y-Leu-Y-D-Phe-Pro-Y-Leu- molecule and the hydrophobic Val and Leu side chains are situated on Y-oxime from the resin was performed in 1,4-dioxane with 2 equiv the other side. -

History of Microbiology Milton Wainwright University of Sheffield Joshua Lederbergl the Rockefeller University
History of Microbiology Milton Wainwright University of Sheffield Joshua Lederbergl The Rockefeller University I. Observations without Application ness of the nature and etiology of disease, with the II. The Spontaneous Generation Controversy result that the majority of the traditional killer dis- III. Tools of the Trade eases have now been conquered. Similar strides IV. Microorganisms as Causal Agents of have been made in the use of microorganisms in Disease industry. and more recently attempts are being made V. Chemotherapy and Antibiosis to apply our knowledge of microbial ecology and VI. Microbial Metabolism and Applied physiology to help solve environmental problems. A Microbiology dramatic development and broadening of the subject VII. Nutrition, Comparative Biochemistry, and of microbiology has taken place since World War II. Other Aspects of Metabolism Microbial genetics, molecular biology, and bio- VIII. Microbial Genetics technology in particular have blossomed. It is to be IX. Viruses and Lysogeny: The Plasmid hoped that these developments are sufficiently op- Concept portune to enable us to conquer the latest specter of X. Virology disease facing us, namely AIDS. Any account of the XI. Mycology and Protozoology, history of a discipline is. by its very nature, a per- Microbiology’s Cinderellas sonal view: hopefully, what follows includes all the XII. Modern Period major highlights in the development of our science. The period approximating 1930-1950 was a ‘vi- cennium” of extraordinary transformation of micro- Glossary biology, just prior to the landmark publication on the structure of DNA by Watson and Crick in 1953. Antibiotics Antimicrobial agents produced b) We have important milestones for the vicennium: living organisms Jordan and Falk (1928) and “System of Bacteriol- Bacterial genetics Study of genetic elements and ogy” (1930) at its start are magisterial reviews of hereditary in bacteria prior knowledge and thought. -

Mode of Action of Daptomycin, a Lipopeptide Antibiotic
Mode of Action of Daptomycin, a Lipopeptide Antibiotic by Jawad Kadhum Muraih A thesis presented to the University of Waterloo in fulfillment of the thesis requirement for the degree of Doctor of Philosophy in Chemistry (Biochemistry) Waterloo, Ontario, Canada, 2012 © Jawad Kadhum Muraih 2012 Author’s Declaration I hereby declare that I am the sole author of this thesis. This is a true copy of the thesis, including any required final revisions, as accepted by my examiners. I understand that my thesis may be made electronically available to the public. Jawad K. Muraih iii Abstract Daptomycin is a lipopeptide antibiotic that contains 13 amino acids and an N-terminally at- tached fatty acyl residue. The antibiotic kills Gram-positive bacteria by membrane depolariza- tion. It has long been assumed that the mode of action of daptomycin involves the formation of oligomers on the bacterial cell membrane; however, at the outset of my studies, this had not been experimentally demonstrated. In the work described in this thesis, I have used fluorescence energy transfer (FRET) be- tween native daptomycin and an NBD-labeled daptomycin derivative to demonstrate that the antibiotic indeed forms oligomers on bacterial cell membranes. In a liposome model, oligomer formation depends on calcium and on phosphatidylglycerol (PG). The oligomer forms rapidly and is stable for a length of time longer than required for the bactericidal effect. Through vari- ation of the ratio of FRET donor (native daptomycin) and acceptor (NBD-daptomycin), I have determined that the oligomer consists of approximately 6–7 molecules, or, depending on the structure of the oligomer, possibly up to twice that number. -

The Lipopeptide Antibiotic Daptomycin: Its Interaction with Calcium and Membranes and the Effects of Membrane Lipid Composition on Its Activity
The Lipopeptide Antibiotic Daptomycin: Its Interaction With Calcium And Membranes And The Effects Of Membrane Lipid Composition On Its Activity by Robert Mackay Taylor A thesis presented to the University of Waterloo in fulfillment of the thesis requirement for the degree of Doctor of Philosophy in Chemistry Waterloo, Ontario, Canada, 2018 ©Robert Mackay Taylor 2018 Examining Committee Membership The following served on the Examining Committee for this thesis. The decision of the Examining Committee is by majority vote. External Examiner Dr. Richard M. Epand, PhD. Professor Emeritus, McMaster University Biochemistry and Biomedical Sciences Supervisor Dr. Scott D. Taylor, PhD. Professor, University of Waterloo Chemistry Internal Member Dr. Michael Palmer, PhD. M.D., Dr. habil Associate Professor, University of Waterloo Chemistry Internal-external Member Dr. Zoya Leonenko, PhD. Professor, University of Waterloo Physics and Astronomy Other Member(s) Dr. Thorsten Dieckmann, PhD. Associate Professor, University of Waterloo Associate Chair (Graduate Studies and Research) Chemistry Dr. John Honek, PhD. Professor, University of Waterloo Chemistry ii Author’s Declaration I hereby declare that I am the sole author of this thesis. This is a true copy of the thesis, including any required final revisions, as accepted by my examiners. I understand that my thesis may be made electronically available to the public. iii Abstract Daptomycin (Dap) is a calcium-dependent cyclic lipodepsipeptide antibiotic used clinically to treat infections with pathogenic Gram-positive bacteria, including methicillin-resistant Staphylococcus aureus (MRSA). It targets the cell membrane, which must contain phosphatidylglycerol (PG) for activity. Although Dap was discovered over 30 years ago, its mechanism of action is still debated among researchers.