An Update of Palmitoylethanolamide and Luteolin Effects in Preclinical
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Investigation of Key Genes and Pathways in Inhibition of Oxycodone on Vincristine-Induced Microglia Activation by Using Bioinformatics Analysis
Hindawi Disease Markers Volume 2019, Article ID 3521746, 10 pages https://doi.org/10.1155/2019/3521746 Research Article Investigation of Key Genes and Pathways in Inhibition of Oxycodone on Vincristine-Induced Microglia Activation by Using Bioinformatics Analysis Wei Liu,1 Jishi Ye,2 and Hong Yan 1 1Department of Anesthesiology, the Central Hospital of Wuhan, Tongji Medical College, Huazhong University of Science and Technology, Wuhan 430014, China 2Department of Anesthesiology, Renmin Hospital of Wuhan University, Wuhan, 430060 Hubei, China Correspondence should be addressed to Hong Yan; [email protected] Received 2 November 2018; Accepted 31 December 2018; Published 10 February 2019 Academic Editor: Hubertus Himmerich Copyright © 2019 Wei Liu et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. Introduction. The neurobiological mechanisms underlying the chemotherapy-induced neuropathic pain are only partially understood. Among them, microglia activation was identified as the key component of neuropathic pain. The aim of this study was to identify differentially expressed genes (DEGs) and pathways associated with vincristine-induced neuropathic pain by using bioinformatics analysis and observe the effects of oxycodone on these DEG expressions in a vincristine-induced microglia activation model. Methods. Based on microarray profile GSE53897, we identified DEGs between vincristine-induced neuropathic pain rats and the control group. Using the ToppGene database, the prioritization DEGs were screened and performed by gene ontology (GO) and signaling pathway enrichment. A protein-protein interaction (PPI) network was used to explore the relationship among DEGs. -
Inhibitory Effects of Phytochemicals on Metabolic Capabilities of CYP2D6*1 and CYP2D6*10 Using Cell-Based Models in Vitro
Acta Pharmacologica Sinica (2014) 35: 685–696 npg © 2014 CPS and SIMM All rights reserved 1671-4083/14 $32.00 www.nature.com/aps Original Article Inhibitory effects of phytochemicals on metabolic capabilities of CYP2D6*1 and CYP2D6*10 using cell-based models in vitro Qiang QU1, 2, Jian QU1, Lu HAN2, Min ZHAN1, Lan-xiang WU3, Yi-wen ZHANG1, Wei ZHANG1, Hong-hao ZHOU1, * 1Institute of Clinical Pharmacology, Hunan Key Laboratory of Pharmacogenetics, Xiangya Hospital, Central South University, Changsha 410078, China; 2Xiangya Hospital, Central South University, Changsha 410008, China; 3Institute of Life Sciences, Chongqing Medical University, Chongqing 400016, China Aim: Herbal products have been widely used, and the safety of herb-drug interactions has aroused intensive concerns. This study aimed to investigate the effects of phytochemicals on the catalytic activities of human CYP2D6*1 and CYP2D6*10 in vitro. Methods: HepG2 cells were stably transfected with CYP2D6*1 and CYP2D6*10 expression vectors. The metabolic kinetics of the enzymes was studied using HPLC and fluorimetry. Results: HepG2-CYP2D6*1 and HepG2-CYP2D6*10 cell lines were successfully constructed. Among the 63 phytochemicals screened, 6 compounds, including coptisine sulfate, bilobalide, schizandrin B, luteolin, schizandrin A and puerarin, at 100 μmol/L inhibited CYP2D6*1- and CYP2D6*10-mediated O-demethylation of a coumarin compound AMMC by more than 50%. Furthermore, the inhibition by these compounds was dose-dependent. Eadie-Hofstee plots demonstrated that these compounds competitively inhibited CYP2D6*1 and CYP2D6*10. However, their Ki values for CYP2D6*1 and CYP2D6*10 were very close, suggesting that genotype- dependent herb-drug inhibition was similar between the two variants. -
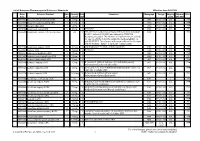
List of European Pharmacopoeia Reference Standards Effective From
List of European Pharmacopoeia Reference Standards Effective from 2021/10/6 Order Reference Standard Batch Quantity Sale Information Monograph Storage Shipping Shipment Price Code n° per vial Unit group with DGD Y0001552 Abacavir for peak identification CRS 1 10 mg 1 2589 +5°C+/-3°C A1A 79 € Y0001551 Abacavir for system suitability CRS 1 10 mg 1 2589 +5°C+/-3°C A1A 79 € Y0001561 Abacavir sulfate CRS 1 20 mg 1 2589 +5°C+/-3°C A1A 79 € Y0002199 Acamprosate calcium CRS 1 80 mg 1 See leaflet 1585 +5°C+/-3°C A1A 79 € Y0000055 Acamprosate calcium - reference spectrum 1 n/a 1 This reference standard was officially withdrawn from monograph 1585 L 79 € 01/2017:1585 on 01/01/2021 and replaced by Y0002199 Acamprosate calcium. The reference will however remain available for sale for a further 6 months (subject to stock availability), i.e. until 01/07/2021. The reference will remain visible in the catalogue until 01/01/2022. ; Batch 1 is valid until 1 January 2022 Y0000116 Acamprosate impurity A CRS 2 110 mg 1 3-aminopropane-1-sulfonic acid (homotaurine) 1585 +5°C+/-3°C A1A 79 € Y0000500 Acarbose CRS 3 100 mg 1 See leaflet 2089 +5°C+/-3°C A1A 79 € Y0000354 Acarbose for identification CRS 1 10 mg 1 2089 +5°C+/-3°C A1A 79 € Y0000427 Acarbose for peak identification CRS 4 20 mg 1 2089 +5°C+/-3°C A1A 79 € A0040000 Acebutolol hydrochloride CRS 1 50 mg 1 0871 +5°C+/-3°C A1A 79 € Y0000359 Acebutolol impurity B CRS 2 10 mg 1 N-[3-acetyl-4-[(2RS)-2-hydroxy-3-[(1-methylethyl)amino] 0871 +5°C+/-3°C A1A 79 € propoxy]phenyl]acetamide (diacetolol) Y0000127 Acebutolol -

Alkaloids Used As Medicines: Structural Phytochemistry Meets Biodiversity—An Update and Forward Look
molecules Review Alkaloids Used as Medicines: Structural Phytochemistry Meets Biodiversity—An Update and Forward Look Michael Heinrich 1,2,* , Jeffrey Mah 1 and Vafa Amirkia 1 1 Research Group ‘Pharmacognosy and Phytotherapy’, UCL School of Pharmacy, University of London, 29–39 Brunswick Sq., London WC1N 1AX, UK; [email protected] (J.M.); [email protected] (V.A.) 2 Graduate Institute of Integrated Medicine, College of Chinese Medicine, and Chinese Medicine Research Center, China Medical University, No. 100, Section 1, Jingmao Road, Beitun District, Taichung 406040, Taiwan * Correspondence: [email protected]; Tel.: +44-20-7753-5844 Abstract: Selecting candidates for drug developments using computational design and empirical rules has resulted in a broad discussion about their success. In a previous study, we had shown that a species’ abundance [as expressed by the GBIF (Global Biodiversity Information Facility)] dataset is a core determinant for the development of a natural product into a medicine. Our overarching aim is to understand the unique requirements for natural product-based drug development. Web of Science was queried for research on alkaloids in combination with plant systematics/taxonomy. All alkaloids containing species demonstrated an average increase of 8.66 in GBIF occurrences between 2014 and 2020. Medicinal Species with alkaloids show higher abundance compared to non-medicinal alkaloids, often linked also to cultivation. Alkaloids with high biodiversity are often simple alkaloids found in multiple species with the presence of ’driver species‘ and are more likely to be included in early-stage drug development compared to ‘rare’ alkaloids. Similarly, the success of an alkaloid Citation: Heinrich, M.; Mah, J.; Amirkia, V. -
Analytical Reference Standards
Cerilliant Quality ISO GUIDE 34 ISO/IEC 17025 ISO 90 01:2 00 8 GM P/ GL P Analytical Reference Standards 2 011 Analytical Reference Standards 20 811 PALOMA DRIVE, SUITE A, ROUND ROCK, TEXAS 78665, USA 11 PHONE 800/848-7837 | 512/238-9974 | FAX 800/654-1458 | 512/238-9129 | www.cerilliant.com company overview about cerilliant Cerilliant is an ISO Guide 34 and ISO 17025 accredited company dedicated to producing and providing high quality Certified Reference Standards and Certified Spiking SolutionsTM. We serve a diverse group of customers including private and public laboratories, research institutes, instrument manufacturers and pharmaceutical concerns – organizations that require materials of the highest quality, whether they’re conducing clinical or forensic testing, environmental analysis, pharmaceutical research, or developing new testing equipment. But we do more than just conduct science on their behalf. We make science smarter. Our team of experts includes numerous PhDs and advance-degreed specialists in science, manufacturing, and quality control, all of whom have a passion for the work they do, thrive in our collaborative atmosphere which values innovative thinking, and approach each day committed to delivering products and service second to none. At Cerilliant, we believe good chemistry is more than just a process in the lab. It’s also about creating partnerships that anticipate the needs of our clients and provide the catalyst for their success. to place an order or for customer service WEBSITE: www.cerilliant.com E-MAIL: [email protected] PHONE (8 A.M.–5 P.M. CT): 800/848-7837 | 512/238-9974 FAX: 800/654-1458 | 512/238-9129 ADDRESS: 811 PALOMA DRIVE, SUITE A ROUND ROCK, TEXAS 78665, USA © 2010 Cerilliant Corporation. -

Optimal Management for Alcoholic Liver Disease: Conventional Medications, Natural Therapy Or Combination?
Submit a Manuscript: http://www.wjgnet.com/esps/ World J Gastroenterol 2016 January 7; 22(1): 0000-0000 Help Desk: http://www.wjgnet.com/esps/helpdesk.aspx ISSN 1007-9327 (print) ISSN 2219-2840 (online) DOI: 10.3748/wjg.v22.i1.0000 © 2016 Baishideng Publishing Group Inc. All rights reserved. TOPIC HIGHLIGHT 2016 Alcoholic Liver Disease: Global view Optimal management for alcoholic liver disease: Conventional medications, natural therapy or combination? Moon-Sun Kim, Madeleine Ong, Xianqin Qu Moon-Sun Kim, Madeleine Ong, XianQin Qu, School of disease (ALD) is defined by histological lesions on the Medical & Molecular Biosciences, University of Technology liver that can range from simple hepatic steatosis to Sydney, NSW 2007, Australia more advanced stages such as alcoholic steatohepatitis, cirrhosis, hepatocellular carcinoma and liver failure. As Moon-Sun Kim, Faculty of Pharmacy, University of Sydney, one of the oldest forms of liver injury known to humans, NSW 2006, Australia ALD is still a leading cause of liver-related morbidity Author contributions: Qu X, Kim MS and Ong M contributed and mortality and the burden is exerting on medical to writing the manuscript. Kim MS produced the figures and systems with hospitalization and management costs Ong M thoroughly edited the manuscript rising constantly worldwide. Although the biological mechanisms, including increasing of acetaldehyde, Conflict-of-interest statement: No conflict of interest. oxidative stress with induction of cytochrome p450 2E1, inflammatory cytokine release, abnormal lipid Open-Access: This article is an open-access article which was metabolism and induction of hepatocyte apoptosis, selected by an in-house editor and fully peer-reviewed by external by which chronic alcohol consumption triggers serious reviewers. -

Identification of the Kappa-Opioid Receptor As a Therapeutic Target for Oligodendrocyte Remyelination
The Journal of Neuroscience, July 27, 2016 • 36(30):7925–7935 • 7925 Cellular/Molecular Identification of the Kappa-Opioid Receptor as a Therapeutic Target for Oligodendrocyte Remyelination Feng Mei,1,5* X Sonia R. Mayoral,1* Hiroko Nobuta,2 XFei Wang,5 X Caroline Desponts,3 Daniel S. Lorrain,3 XLan Xiao,5 X Ari J. Green,1,4 David Rowitch,2 Jennifer Whistler,1,6 and XJonah R. Chan1,6 1Department of Neurology, University of California, San Francisco, California 94158, 2Department of Pediatrics and Neurosurgery, Eli and Edythe Broad Institute for Stem Cell Research and Regeneration Medicine and Howard Hughes Medical Institute, University of California, San Francisco, California 94143, 3Inception Sciences, San Diego, California 92121, 4Department of Ophthalmology, University of California, San Francisco, California 94158, 5Department of Histology and Embryology, Chongqing Key Laboratory of Neurobiology, Third Military Medical University, Chongqing, 400038, China, and 6Program in Neuroscience, University of California, San Francisco, California 94158 Remyelinating therapies seek to promote restoration of function and normal cellular architecture following demyelination in diseases, such as multiple sclerosis (MS). Functional screening for small molecules or novel targets for remyelination is a major hurdle to the identification and development of rational therapeutics for MS. Recent findings and technical advances provide us with a unique opportunity to provide insight into the cell autonomous mechanisms for remyelination and address this unmet need. Upon screening a G-protein-coupled receptor small-molecule library, we report the identification of a cluster of -opioid receptor (KOR) agonists that significantly promotes oligodendrocyte differentiation and myelination. KOR agonists were validated in purified rat oligodendroglial cultures, and the (Ϯ)U-50488 compound proved to be most effective for differentiation. -

Selective Opioid Growth Factor Receptor Antagonists Based on a Stilbene Isostere
HHS Public Access Author manuscript Author ManuscriptAuthor Manuscript Author Bioorg Med Manuscript Author Chem. Author Manuscript Author manuscript; available in PMC 2018 August 15. Published in final edited form as: Bioorg Med Chem. 2017 August 15; 25(16): 4464–4474. doi:10.1016/j.bmc.2017.06.035. Selective opioid growth factor receptor antagonists based on a stilbene isostere David P. Stockdalea, Michelle B. Titunickb, Jessica M. Bieglerc,d, Jessie L. Reedc,d, Alyssa M. Hartunga, David F. Wiemera, Patricia J. McLaughlinb,d, and Jeffrey D. Neighborsc,d aDepartment of Chemistry, The University of Iowa, Iowa City, IA 52242-1294, United States bDepartment of Neural and Behavioral Sciences, Pennsylvania State University College of Medicine, Hershey, PA 17033, United States cDepartment of Pharmacology and Medicine, Pennsylvania State University College of Medicine, Hershey, PA 17033, United States dPennsylvania State University Cancer Institute, Hershey, PA 17033, United States Abstract As part of an ongoing drug development effort aimed at selective opioid receptor ligands based on the pawhuskin natural products we have synthesized a small set of amide isosteres. These amides were centered on lead compounds which are selective antagonists for the delta and kappa opioid receptors. The amide isomers revealed here show dramatically different activity from the parent stilbene compounds. Three of the isomers synthesized showed antagonist activity for the opioid growth factor (OGF)/opioid growth factor receptor (OGFR) axis which is involved in cellular and organ growth control. This cellular signaling mechanism is targeted by “low-dose” naltrexone therapy which is being tested clinically for multiple sclerosis, Crohn’s disease, cancer, and wound healing disorders. -

Toxicology Reference Laboratory
TOXICOLOGY REFERENCE LABORATORY Laboratory User Guide ROOM 708, BLOCK P PRINCESS MARGARET HOSPITAL 2-10 Princess Margaret Hospital Road Lai Chi Kok Tel: 2990 1941 Fax: 2990 1942 http://trl.home Version 6.1 Effective date: 1/July/2014 Contents Contents ..................................................................................................................................................... 2 Introduction ............................................................................................................................................... 4 Staff ............................................................................................................................................................ 5 Honorary Medical Staff .......................................................................................................................... 5 Scientific Staff ........................................................................................................................................ 5 Technical Staff ........................................................................................................................................ 5 Supportive Staff ...................................................................................................................................... 6 How to Make Laboratory Request .......................................................................................................... 7 Instruction for Referring Clinician ........................................................................................................ -

By Submitted in Partial Satisfaction of the Requirements for Degree of in In
Repurposing renin angiotensin pathway inhibitors as disease modifying therapeutics for Parkinson’s Disease by Gha-hyun Kim THESIS Submitted in partial satisfaction of the requirements for degree of DOCTOR OF PHILOSOPHY in Pharmaceutical Sciences and Pharmacogenomics in the GRADUATE DIVISION of the UNIVERSITY OF CALIFORNIA, SAN FRANCISCO Approved: ______________________________________________________________________________Su Guo Chair ______________________________________________________________________________Marina Sirota ______________________________________________________________________________Jason Gestwicki ______________________________________________________________________________ ______________________________________________________________________________ Committee Members ii To Suk Jeong Kim, fighting against Parkinson’s disease iii ACKNOWLEDGEMENTS “There is still a lot to learn and there is always great stuff out there. Even mistakes can be wonderful.” Robin Williams, who also struggled to combat Parkinson’s disease, accurately portrayed my PhD journey and thesis work. First and foremost, I want to thank Dr. Su Guo, my thesis advisor, mentor, and pharmacogenomics class professor. During the time when I was deciding on a lab to conduct my Pharmaceutical Sciences pathway project, Su was very inviting towards me joining the lab that allowed me to develop my PharmD thesis and transition into the PhD program. Without significant experience in molecular biology and neuroscience, Su was very patient and understanding as -

Morphine Withdrawal Attenuating Effect, Toxicity and Alkaloid Composition of Sophora Alopecuroides L. Var. Alopecuroides
Research Journal of Pharmacognosy (RJP) 4(1), 2017: 59-66 Received: Aug 2016 Accepted: Oct 2016 Original article Morphine withdrawal attenuating effect, toxicity and alkaloid composition of Sophora alopecuroides L. var. alopecuroides S. Kianbakht1*, R. Hajiaghaee1, A. Ramezani Salehabad2 1Medicinal Plants Research Center, Institute of Medicinal Plants, ACECR, Karaj, Iran. 2Behsazan Machinery Manufacturing Company, Rafsanjan, Kerman Province, Iran. Abstract Background and objectives: The seeds of Sophora alopecuroides L. var. alopecuroides may benefit treatment of opioid dependence. Therefore, the plant alkaloid composition, toxicity and effects on morphine withdrawal were studied. Methods: The alkaloid composition was determined by GC and GC/MS analysis. Mice were made dependent by morphine injected 3 times a day for 3 days. The withdrawal jumping and diarrhea were induced by administration of naloxone 2 h after the 10th injection of morphine on the day 4. The ethanol 90% extract (100, 200, 300 mg/kg), alkaloid fraction (5, 10, 20 mg/kg), morphine (50 mg/kg) or saline were injected 30 min before naloxone. All drugs were injected subcutaneously to groups each consisting of 10 mice. To assess toxicity, different doses of the ethanol or aqueous extracts dissolved in normal saline were gavaged once to groups each consisting of 30 mice. Afterward, the numbers of dead animals within 72 h after gavage were counted and LD50 was calculated. Results: Matrine, cytisine, sophoridine, n-methyl cytisine, sophocarpine and sophoramine were the major alkaloids. All doses of the total extract, alkaloid fraction and morphine decreased jumping and diarrhea significantly compared to the saline (p<0.001). The effects of the total extract and alkaloid fraction were not significantly different from morphine (p>0.05). -

(12) Patent Application Publication (10) Pub. No.: US 2013/0252924 A1 Penninger Et Al
US 20130252924A1 (19) United States (12) Patent Application Publication (10) Pub. No.: US 2013/0252924 A1 Penninger et al. (43) Pub. Date: Sep. 26, 2013 (54) COMPOUNDS AND METHODS FOR Publication Classification TREATING PAIN (51) Int. C. (75) Inventors: Josef Penninger, Vienna (AT); Graham A63/675 (2006.01) Gregory Neely, Sydney (AU); Shane A613 L/496 (2006.01) McManus, Vienna (AT); Henrik A613 L/50 (2006.01) Nilsson, Vienna (AT) A613 L/435 (2006.01) A613 L/506 (2006.01) (73) Assignee: AKRON MOLECULES GMBH, A 6LX3L/277 (2006.01) Vienna (AT) (52) U.S. C. CPC ............. A6 IK3I/675 (2013.01); A61 K3I/506 (21) Appl. No.: 13/884,920 (2013.01); A61 K3I/277 (2013.01); A61 K 3 1/50 (2013.01); A61K3I/435 (2013.01); (22) PCT Fled: Nov. 11, 2011 A6 IK3I/496 (2013.01) USPC ........ 514/81: 514/252.19; 514/521; 514/247; (86) PCT NO.: 514/352: 514/253.06 S371 (c)(1), (2), (4) Date: May 10, 2013 (57) ABSTRACT (30) Foreign Application Priority Data The present invention relates to new therapies to treat pain and related diseases, as well as pharmaceutical compounds Nov. 11, 2010 (EP) .................................. 1O190922.4 for use in said therapies. Patent Application Publication Sep. 26, 2013 Sheet 1 of 25 US 2013/0252924 A1 Fig. 1 A : B Control painless Avoidance 8. 8 9 40 is 20 LE 3 35' as 3. 3s. 45 Temperature C C Paser re. SR + UAS-DCR2 Transgene 0.150- Control c X pairessp . -- store 1.65 Citroff s 0.050- ty F.